

Learn how trauma changes the brain and how neuroplasticity and trauma research offer hope for healing, recovery, and building new pathways for well-being.
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually, with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet millions of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June.You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
It's easy to feel like a different person after a traumatic event. Maybe you're more anxious, quicker to react, or just feel disconnected from yourself. This isn't just in your head; it's a real personality change after trauma. So, does trauma change the brain? Absolutely. During a traumatic event, our brains shift into overdrive to protect us. The challenge is that this survival mode can get stuck long after the threat is gone. But here’s the hopeful part: these changes aren't permanent. The science of neuroplasticity and trauma shows us our brains can heal and create new pathways for safety and calm.
Despite the rough weather, our ships have an amazing ability to repair and reroute. Trauma may alter our course –– but it doesn't define our destination. And It doesn’t define who we are.
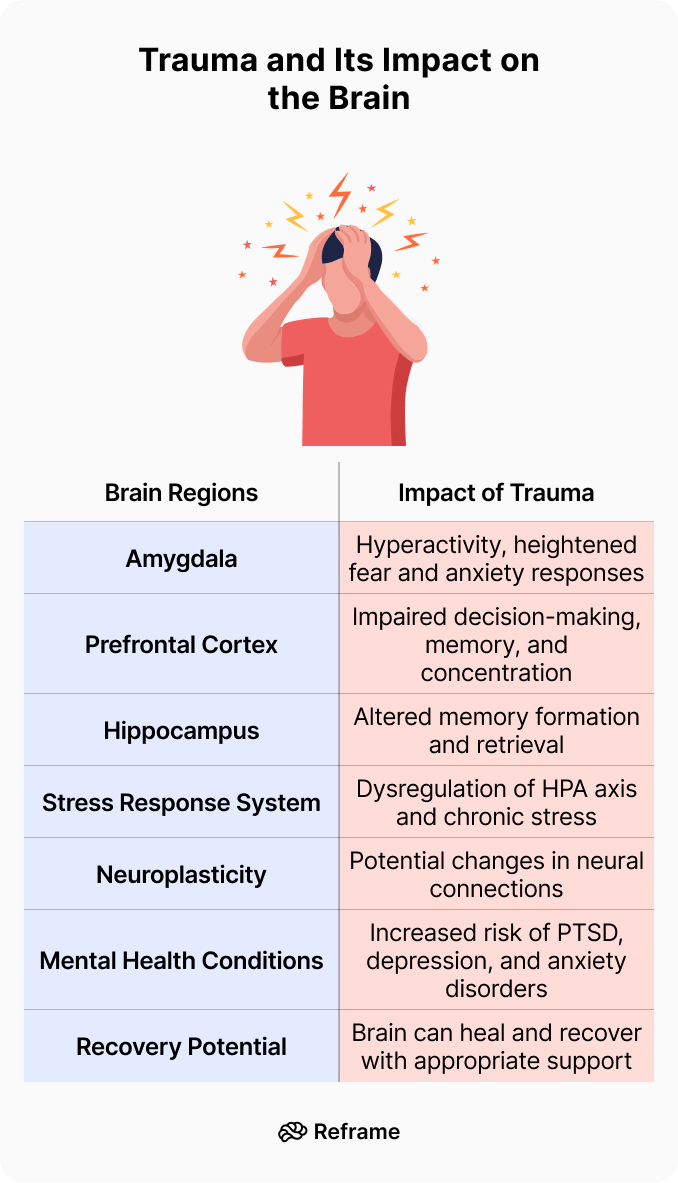
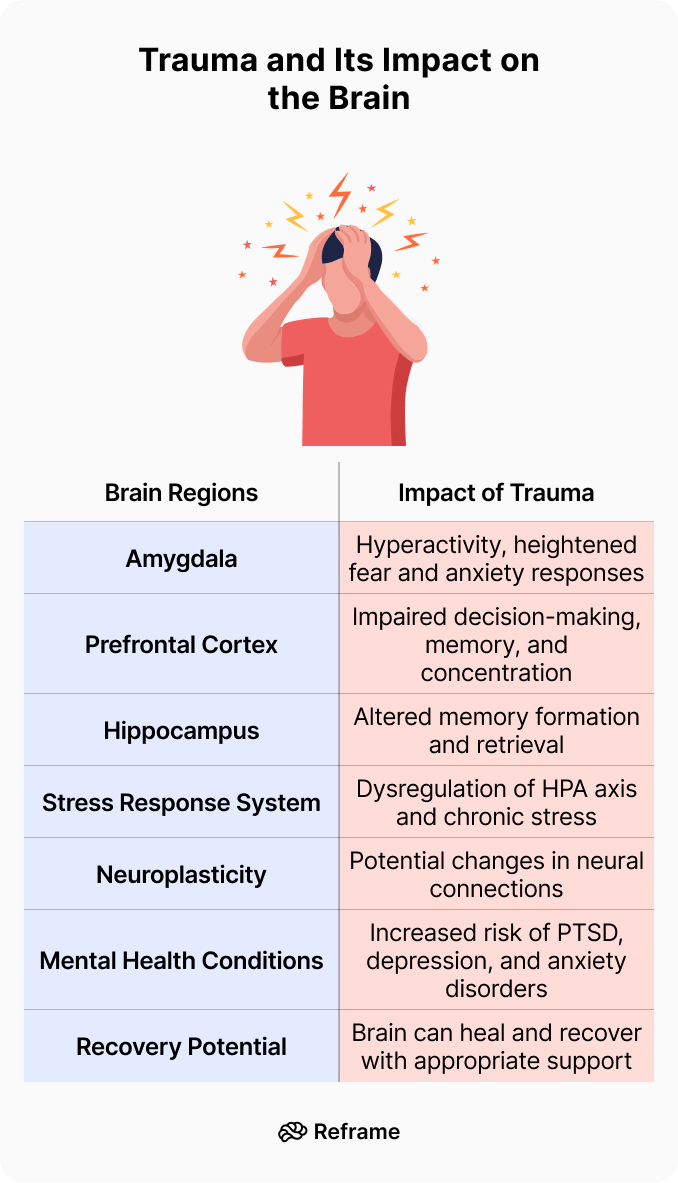
Trauma can cause lasting changes in the brain, altering its structure and function in many ways. Let's explore how this happens –– and how to heal.
When you experience a traumatic event, your brain’s survival instincts take over. The amygdala, your brain's emotional alarm system, goes on high alert, while the prefrontal cortex—the part responsible for logic and decision-making—takes a backseat. This triggers the classic "fight, flight, or freeze" response, flooding your body with stress hormones to help you survive the perceived threat. In a non-traumatic situation, this system would return to normal once the danger has passed. However, trauma can cause this alarm system to get stuck in the "on" position, fundamentally altering how your brain processes information and perceives threats in the world around you.
Living with a brain that's constantly on guard is incredibly taxing. It can lead to a persistent state of hypervigilance, where you feel on edge even in safe environments. Because trauma can also impact the hippocampus, the area responsible for memory, you might struggle with fragmented or intrusive memories of the event. These long-term changes can make emotional regulation feel like an uphill battle, leading many to seek ways to quiet the noise. The good news is that our brains have an incredible ability to adapt and form new connections. This process, known as neuroplasticity, is the key to healing and offers a hopeful path forward.
Trauma is a deeply distressing or disturbing experience that overwhelms our ability to cope. It can be a single event, multiple events, or a set of circumstances that is experienced as physically or emotionally harmful. It can be caused by one-time horrible experiences –– like physical abuse, sexual assault, witnessing violence, or surviving natural disasters –– or enduring long-term neglect or emotional abuse.
Trauma changes the brain. It alters its structure and function, affecting how we process emotions, how we think –– and even our risk for mental health issues. Understanding these changes is crucial for those of us who have experienced trauma, as it provides insight into why we may struggle with certain aspects of our lives.
When we live through trauma, our brains respond to protect us from harm. Think of its response as a built-in alarm system.
When faced with danger, the brain shifts into reactive mode, activating the sympathetic nervous system and signaling the release of stress hormones, preparing the body for survival mode –– fight, flight, or freeze. Our heart rate increases, our muscles tense up for action, and our senses become hyper-alert.
However, when trauma occurs repeatedly or is particularly severe, this protective mechanism can go into overdrive, leading to changes in the brain's structure and function.
For instance, trauma can shrink certain parts of the brain, such as the hippocampus (a region involved in learning and memory) and enlarge others, like the amygdala (the area responsible for fear responses).
It’s easy to look at the aftereffects of trauma and feel like something inside is broken. But what if we shifted that perspective? Newer research suggests that many of the changes our brains undergo aren't signs of damage, but are actually clever adaptations for survival. When faced with harsh or unpredictable environments, especially during childhood, the brain rewires itself to stay safe. A heightened sense of alert or a quickness to react weren’t flaws; they were features that helped you get through an incredibly difficult time. Viewing these traits as survival strategies, rather than defects, can be a powerful and compassionate step on the path to healing.
When trauma happens, especially if it's early in life and ongoing, it can cause significant, long-lasting changes to the brain’s structure. Key areas are affected, including the hippocampus (which manages memory), the prefrontal cortex (our hub for planning and decision-making), and the amygdala (the brain’s emotion and fear center). Trauma can make the amygdala overactive, essentially keeping the body’s alarm system on high alert. At the same time, it can weaken the prefrontal cortex’s ability to regulate those intense emotional responses. This imbalance is why someone might feel constantly on edge or react strongly to minor stressors. This state of high alert, fueled by stress hormones like cortisol, can disrupt normal brain development and affect long-term physical and mental health.
This brings us to an important concept called neuroplasticity — our brain's ability to change by forming new connections between neurons (brain cells). While neuroplasticity allows us to learn new skills and adapt to different environments, it also means our brains are vulnerable to negative influences like trauma.
This means repeated exposure to traumatic events can "rewire" our brains — altering how we think, feel and behave.
There is an upside: just as our brains can change in response to negative experiences, they also have the ability to heal and recover.
So, how does the brain actually heal? The answer lies in its incredible capacity for neuroplasticity. For a long time, scientists believed our brains were pretty much set in stone after childhood. We now know that’s not true — the brain is constantly changing and adapting throughout our entire lives. This happens in two main ways: structurally and functionally. Structural plasticity refers to physical changes, like the brain creating new connections between neurons. Functional plasticity is about changes in how different brain areas communicate and work together. While trauma can cause negative changes on both fronts, the reverse is also true. Through intentional healing practices, we can encourage positive structural and functional shifts, effectively rewiring our brains for recovery and well-being.
Understanding that the brain can change is one thing, but knowing *how* it changes can be incredibly empowering. It’s not a vague, abstract process; it’s a series of concrete biological mechanisms. When we understand these core mechanisms, we can see how our efforts to heal directly influence our brain's biology. This knowledge helps demystify recovery, transforming it from a hopeful wish into a tangible process we can actively participate in. It shows us that healing isn't just about feeling better, but about fundamentally reshaping the neural circuits that influence our thoughts, emotions, and behaviors. Let’s look at a few of the key ways our brains build new pathways and pave the road to well-being.
One of the most fundamental principles of neuroplasticity is that “cells that fire together, wire together.” This is called synaptic plasticity. Think of it like creating a path in a grassy field. The first time you walk it, it’s tough going. But the more you use that same path, the clearer and easier it becomes to follow. In your brain, every time you repeat a thought, feeling, or action, you strengthen the neural connection responsible for it. At the same time, your brain is capable of neurogenesis — growing entirely new brain cells. Positive experiences and healthy habits can encourage this growth, giving you fresh resources to build new, healthier pathways while the old, trauma-worn paths gradually fade from disuse.
Beyond creating new connections, your brain can also change how it uses its existing resources. Epigenetics is a fascinating process where life experiences can act like switches, turning certain genes on or off without altering your DNA. While trauma might flip on genes related to stress and fear, healing practices can help flip them off again. Another process, white matter plasticity, is like upgrading your brain’s pathways from dirt roads to superhighways. As you consistently practice new, healthy behaviors, the brain wraps these important pathways in a fatty coating called myelin. This insulation makes the signals travel much faster and more efficiently, making your new habits feel more automatic and natural over time.
These changes in the brain aren't just happening in the background; they show up in our day-to-day lives. Trauma can leave lasting “imprints” on our brain and stress systems, making it much harder to manage everyday pressures. This is why trauma significantly increases the risk for mental health conditions like Post-Traumatic Stress Disorder (PTSD) and depression. Even without a specific diagnosis, you might notice the effects as heightened anxiety, feeling emotionally numb, or having a shorter fuse than you used to. It’s as if your internal alarm system, once designed to protect you, is now stuck in the “on” position, seeing potential threats everywhere.
When your brain is constantly on high alert, it’s completely exhausting. This state of hypervigilance can cause you to change your behaviors to feel safe. For instance, repeated exposure to traumatic events can rewire our brains, leading us to avoid people, places, or activities that remind us of the experience. It’s also common to look for ways to quiet this internal noise, which is why many people turn to coping mechanisms like alcohol to find temporary relief. This isn't a sign of weakness; it's a sign that your brain is trying to find a way to cope with an overwhelming amount of stress and fear.
Trauma can make emotional regulation a struggle.
Emotional regulation is our ability to manage and respond to emotional experiences in a healthy way.
Trauma can disrupt this process. It can lead to an overactive amygdala (the part of the brain that governs fear responses) and underactivity in the prefrontal cortex (which helps us control emotions and make rational decisions.) This imbalance can result in heightened emotional reactions and difficulty managing stress.
Having a history of trauma can result in intense feelings –– of anxiety, depression, or anger. We may struggle to calm down once we’re upset, or grapple with persistent feelings of sadness or worry. These symptoms demonstrate the changes trauma causes in specific brain regions involved in emotional regulation.
Neuroimaging studies have found alterations in the anterior cingulate cortex (which plays a key role in emotion processing and regulation) and in the insula (involved in our awareness of our emotional states).Healing involves restoring balance within these neural circuits — helping us regain control over our emotions.
Cognition is an umbrella term for the mental processes that make our lives happen, from recognizing familiar faces to solving complex problems. It involves various functions such as attention, memory, and decision-making — all of which trauma impairs.
People who have experienced trauma often report difficulties with attention: they struggle to focus or are easily distracted. Memory issues are also common, including challenges in recalling specific details about events or learning new information. Decision-making can become overwhelming; we avoid making choices altogether or act impulsively instead.
The prefrontal cortex — a region involved in executive functions like decision-making and impulse control — can be affected by trauma. Similarly, prolonged trauma-related stress may cause shrinkage in the hippocampus, an area crucial for memory formation and retrieval.
If you often struggle with cognitive or emotional tasks that others find easy, trauma could play a role.
“Executive functions” might sound like a term for a CEO, but it’s really about the management skills our brain uses every day. Think of it as your brain's control panel for planning, organizing, staying focused, and managing impulses. When trauma affects the prefrontal cortex—the brain's command center—these skills can take a hit. This can make it tough to follow through on plans, switch between tasks, or resist acting on a sudden urge. Research shows that trauma can lead to lasting difficulties with these skills, including working memory and the ability to control impulses. It’s not a personal failing; it's a neurological response to overwhelming experiences, making everyday decision-making feel like a monumental effort.
Experiencing trauma doesn't just affect emotional regulation and cognitive functions. It can also increase your risk for mental illnesses — much as an untreated wound can make us more susceptible to infections.
There’s a strong link between trauma and an increased risk for post-traumatic stress disorder (PTSD), depression, and substance abuse disorders. For instance, individuals who have experienced traumatic events are up to six times more likely to develop PTSD — a condition characterized by intrusive memories, avoidance behaviors, negative changes in mood and cognition, and hyperarousal or reactivity.
Underlying these are changes to those key brain regions — the amygdala, prefrontal cortex, and hippocampus — as well as disruptions to brain chemicals that regulate mood and reward.
What’s more, trauma can lead to dysregulation of the body's stress response system, the hypothalamic-pituitary-adrenal (HPA) axis, resulting in elevated levels of the stress hormone cortisol. Over time, this can contribute to depressive symptoms. Similarly, changes in dopamine — a neurotransmitter involved in reward processing — may make us more vulnerable to substance abuse after trauma. If any of this sounds like you, it’s okay to seek out professional help. You deserve to heal!
Have you ever felt like you were watching your life from outside your own body, as if it were a movie? This experience is known as dissociation, and it’s a common response to trauma. Think of it as your brain’s emergency escape hatch. When an experience is too overwhelming or painful to process, the brain can create a sense of distance to protect you. This feeling of being disconnected from your body, thoughts, or surroundings is a powerful coping mechanism. It’s not a flaw or a weakness; it’s a testament to your mind’s incredible ability to endure the unbearable by temporarily checking out.
This disconnection isn't just mental; it has a profound physical component. Dissociation can make it difficult to be aware of your body's internal signals—a sense known as interoceptive awareness. You might not notice you're hungry until you're starving, or realize you're exhausted until you can barely stand. This happens because, for many trauma survivors, internal bodily sensations can become linked to traumatic memories. To shield you from reliving that pain, your brain might turn down the volume on these signals. It’s another protective measure, but one that can leave you feeling like a stranger in your own skin, making it hard to practice self-care.
Living with this disconnect can be challenging, but it’s important to remember that these neural pathways aren't permanent. Trauma can create overactive or unhelpful neural routes that keep us stuck in these patterns, but our brains are capable of change. The first step toward reconnecting with your body is simply acknowledging this separation without judgment. Practices like mindful drinking or gentle body-scan meditations can help you slowly and safely tune back into your body’s signals. By building new, healthier pathways, you can begin to feel more present and grounded in your own experience, reclaiming the connection that trauma tried to sever.
While trauma can lead to significant changes in the brain, it's crucial to remember that our brains are not static. They possess a remarkable ability for change and growth, called neuroplasticity.
Just as traumatic experiences can alter our brain, positive experiences and interventions can help reshape it.
Research on neuroplasticity provides hope for trauma survivors. Therapeutic interventions like cognitive behavioral therapy (CBT), eye movement desensitization and reprocessing (EMDR), and mindfulness-based practices have been shown to promote healing.
These therapies illustrate how understanding neuroscience can inform effective treatment strategies. They offer hope — and they show us that while trauma may change our brains, we have the power to change them back.
Just as physical therapy can help you regain strength after an injury, certain therapeutic approaches can help your brain heal and form new, healthier pathways. This isn't just about talking through your problems; it's about actively engaging in practices that leverage neuroplasticity to your advantage. These methods provide structured ways to process traumatic memories, manage overwhelming emotions, and develop new coping skills. By consistently engaging in these therapies, you can help your brain move out of a constant state of high alert and into a place of safety and balance, effectively rewiring the circuits that were impacted by trauma.
Cognitive Behavioral Therapy, or CBT, is a practical, goal-oriented approach that helps you identify and challenge negative thought patterns and behaviors. After a traumatic experience, it’s common to get stuck in cycles of thinking that reinforce fear and anxiety. CBT gives you the tools to break these cycles. It works by helping you develop healthier thought patterns, which can strengthen connections within the prefrontal cortex — the part of your brain responsible for rational thinking and decision-making. By changing your thoughts, you can change how you feel and react, empowering you to respond to triggers in a more balanced way.
Mindfulness is the practice of paying attention to the present moment without judgment. For those of us healing from trauma, our minds can often be stuck in the past or worrying about the future. Mindfulness-based treatments gently guide your attention back to the here and now, which can be incredibly grounding. Practices like meditation, deep breathing, and body scans help reduce stress and calm an overactive nervous system. This focus on present-moment awareness doesn't just feel good; it actively promotes overall brain health and helps create a sense of inner peace and stability amidst the chaos of recovery.
Healing from trauma is not a journey you have to take alone. In fact, safe and supportive relationships are one of the most powerful catalysts for recovery. When we connect with people who make us feel seen, heard, and valued, it sends a powerful signal to our nervous system that we are safe. These connections can be with friends, family, a partner, or a therapist. Healthy relationships provide a secure base from which we can explore difficult emotions and experiences. They act as a buffer against stress and remind us that we are not defined by what happened to us, fostering a sense of belonging and hope.
A helpful framework for understanding the power of relationships in healing is the "3 C's": Connect, Co-Regulate, and Co-Reflect. Connection is about forming strong, trusting bonds. Co-regulation is the process of calming your nervous system through interaction with a safe person — think of a soothing conversation or a comforting hug. Co-reflection involves making sense of your experiences with someone you trust. Research shows that strong, supportive relationships can help protect the brain from the harmful effects of trauma, creating an environment where healing is not just possible, but probable.
While therapy and relationships are crucial, the small choices you make every day also play a significant role in your brain's ability to heal. Think of these lifestyle changes as the foundational support system for your recovery. Things like how you sleep, move your body, and nourish yourself directly impact your brain's chemistry and structure. By adopting habits that promote overall well-being, you create an internal environment that is ripe for healing. These consistent, positive actions can help regulate your nervous system, reduce inflammation, and support the growth of new neural connections, making your therapeutic work even more effective.
Never underestimate the healing power of a good night's sleep. While you rest, your brain is hard at work repairing cells, consolidating memories, and clearing out toxins. Sleep is essential for brain growth and recovery, helping to strengthen the pathways that send information between brain cells. Alongside rest, regular physical activity is a game-changer for mental health. Exercise like running or yoga releases endorphins, which are natural mood lifters, and helps reduce levels of stress hormones. Moving your body is a powerful way to process stored tension and reconnect with yourself in a positive, empowering way.
Your environment — both internal and external — can either support or hinder your healing process. Creating a supportive environment means intentionally cultivating spaces, relationships, and mindsets that make you feel safe and nurtured. This could mean setting boundaries with certain people, decluttering your living space to create a sense of calm, or curating the content you consume online. It’s about making conscious choices that protect your energy and promote peace. This isn't about avoiding the world, but about building a personal sanctuary that gives your nervous system a chance to rest and your brain the space it needs to heal.
Two powerful ways to shape your internal environment are practicing gratitude and building community. Gratitude is more than just saying "thank you"; it's a practice that trains your brain to look for the positive, which can help you stay hopeful even on difficult days. You can start by simply thinking of three things you're thankful for each morning. At the same time, connecting with others through healthy friendships or volunteering can provide a profound sense of purpose and belonging. These acts of connection remind you that you are part of something larger than yourself, which is an incredibly powerful force for healing.
Remember: our brains are shaped by experiences, but they're also primed for growth and transformation. Trauma changes our brain –– but healing can, too!
With resilience, therapeutic interventions, and the remarkable power of neuroplasticity on our side, healing is within reach.
Trauma can significantly alter the brain's structure and function, but it doesn't write our destiny.
Are the changes to my brain and personality after trauma permanent? This is such an important question, and the hopeful answer is no, they are not permanent. While trauma can create deep-seated patterns in the brain that make you feel like a different person, these pathways aren't set in stone. Your brain has an incredible ability to adapt and rewire itself throughout your life, a process called neuroplasticity. Through intentional healing practices, you can create new, healthier neural connections, helping your brain learn that it's safe again.
Why do I feel so jumpy and on edge all the time now? That feeling of being constantly on high alert is a common aftereffect of trauma. It happens because the brain's alarm system, the amygdala, gets stuck in overdrive. It learned from the traumatic experience that danger could be anywhere, so it keeps your body flooded with stress hormones to be ready for a threat, even when there isn't one. This state, known as hypervigilance, is exhausting, but it's your brain's attempt to protect you. Healing involves gently teaching this part of your brain that it can stand down and rest.
You mentioned trauma is an 'adaptation.' Does that mean my brain isn't actually damaged? Exactly. It's a powerful shift in perspective to see these changes not as damage, but as your brain's clever adaptations for survival. A heightened sense of alert or a quickness to react weren't flaws; they were features that helped you get through an incredibly difficult time. Viewing these traits as survival strategies, rather than defects, can be a more compassionate way to approach your healing journey. You're not broken; you're a survivor whose brain did what it had to do.
It feels like I'm just 'stuck' in my trauma. How can my brain actually change? Feeling stuck is completely understandable. The neural pathways created by trauma can feel like deep ruts that are hard to get out of. The key is neuroplasticity. Think of it like creating new paths in a field. At first, the old, trauma-worn path is the easiest to take. But every time you engage in a healing activity—whether it's a therapy session, a mindfulness practice, or a safe conversation—you start walking a new path. The more you use these new, healthier pathways, the stronger they become, while the old ones gradually fade from disuse.
Besides therapy, what are some practical things I can do to support my brain's healing? Therapy is a cornerstone of healing, but your daily habits are incredibly important, too. Prioritizing sleep is one of the best things you can do, as your brain does major repair work while you rest. Regular physical movement, like a walk or some gentle yoga, helps process stored stress hormones and reconnect you with your body. Also, creating a safe and calming personal environment can give your nervous system a much-needed break, signaling to your brain that it's okay to relax.
It's easy to feel like a different person after a traumatic event. Maybe you're more anxious, quicker to react, or just feel disconnected from yourself. This isn't just in your head; it's a real personality change after trauma. So, does trauma change the brain? Absolutely. During a traumatic event, our brains shift into overdrive to protect us. The challenge is that this survival mode can get stuck long after the threat is gone. But here’s the hopeful part: these changes aren't permanent. The science of neuroplasticity and trauma shows us our brains can heal and create new pathways for safety and calm.
Despite the rough weather, our ships have an amazing ability to repair and reroute. Trauma may alter our course –– but it doesn't define our destination. And It doesn’t define who we are.
Trauma can cause lasting changes in the brain, altering its structure and function in many ways. Let's explore how this happens –– and how to heal.
When you experience a traumatic event, your brain’s survival instincts take over. The amygdala, your brain's emotional alarm system, goes on high alert, while the prefrontal cortex—the part responsible for logic and decision-making—takes a backseat. This triggers the classic "fight, flight, or freeze" response, flooding your body with stress hormones to help you survive the perceived threat. In a non-traumatic situation, this system would return to normal once the danger has passed. However, trauma can cause this alarm system to get stuck in the "on" position, fundamentally altering how your brain processes information and perceives threats in the world around you.
Living with a brain that's constantly on guard is incredibly taxing. It can lead to a persistent state of hypervigilance, where you feel on edge even in safe environments. Because trauma can also impact the hippocampus, the area responsible for memory, you might struggle with fragmented or intrusive memories of the event. These long-term changes can make emotional regulation feel like an uphill battle, leading many to seek ways to quiet the noise. The good news is that our brains have an incredible ability to adapt and form new connections. This process, known as neuroplasticity, is the key to healing and offers a hopeful path forward.
Trauma is a deeply distressing or disturbing experience that overwhelms our ability to cope. It can be a single event, multiple events, or a set of circumstances that is experienced as physically or emotionally harmful. It can be caused by one-time horrible experiences –– like physical abuse, sexual assault, witnessing violence, or surviving natural disasters –– or enduring long-term neglect or emotional abuse.
Trauma changes the brain. It alters its structure and function, affecting how we process emotions, how we think –– and even our risk for mental health issues. Understanding these changes is crucial for those of us who have experienced trauma, as it provides insight into why we may struggle with certain aspects of our lives.
When we live through trauma, our brains respond to protect us from harm. Think of its response as a built-in alarm system.
When faced with danger, the brain shifts into reactive mode, activating the sympathetic nervous system and signaling the release of stress hormones, preparing the body for survival mode –– fight, flight, or freeze. Our heart rate increases, our muscles tense up for action, and our senses become hyper-alert.
However, when trauma occurs repeatedly or is particularly severe, this protective mechanism can go into overdrive, leading to changes in the brain's structure and function.
For instance, trauma can shrink certain parts of the brain, such as the hippocampus (a region involved in learning and memory) and enlarge others, like the amygdala (the area responsible for fear responses).
It’s easy to look at the aftereffects of trauma and feel like something inside is broken. But what if we shifted that perspective? Newer research suggests that many of the changes our brains undergo aren't signs of damage, but are actually clever adaptations for survival. When faced with harsh or unpredictable environments, especially during childhood, the brain rewires itself to stay safe. A heightened sense of alert or a quickness to react weren’t flaws; they were features that helped you get through an incredibly difficult time. Viewing these traits as survival strategies, rather than defects, can be a powerful and compassionate step on the path to healing.
When trauma happens, especially if it's early in life and ongoing, it can cause significant, long-lasting changes to the brain’s structure. Key areas are affected, including the hippocampus (which manages memory), the prefrontal cortex (our hub for planning and decision-making), and the amygdala (the brain’s emotion and fear center). Trauma can make the amygdala overactive, essentially keeping the body’s alarm system on high alert. At the same time, it can weaken the prefrontal cortex’s ability to regulate those intense emotional responses. This imbalance is why someone might feel constantly on edge or react strongly to minor stressors. This state of high alert, fueled by stress hormones like cortisol, can disrupt normal brain development and affect long-term physical and mental health.
This brings us to an important concept called neuroplasticity — our brain's ability to change by forming new connections between neurons (brain cells). While neuroplasticity allows us to learn new skills and adapt to different environments, it also means our brains are vulnerable to negative influences like trauma.
This means repeated exposure to traumatic events can "rewire" our brains — altering how we think, feel and behave.
There is an upside: just as our brains can change in response to negative experiences, they also have the ability to heal and recover.
So, how does the brain actually heal? The answer lies in its incredible capacity for neuroplasticity. For a long time, scientists believed our brains were pretty much set in stone after childhood. We now know that’s not true — the brain is constantly changing and adapting throughout our entire lives. This happens in two main ways: structurally and functionally. Structural plasticity refers to physical changes, like the brain creating new connections between neurons. Functional plasticity is about changes in how different brain areas communicate and work together. While trauma can cause negative changes on both fronts, the reverse is also true. Through intentional healing practices, we can encourage positive structural and functional shifts, effectively rewiring our brains for recovery and well-being.
Understanding that the brain can change is one thing, but knowing *how* it changes can be incredibly empowering. It’s not a vague, abstract process; it’s a series of concrete biological mechanisms. When we understand these core mechanisms, we can see how our efforts to heal directly influence our brain's biology. This knowledge helps demystify recovery, transforming it from a hopeful wish into a tangible process we can actively participate in. It shows us that healing isn't just about feeling better, but about fundamentally reshaping the neural circuits that influence our thoughts, emotions, and behaviors. Let’s look at a few of the key ways our brains build new pathways and pave the road to well-being.
One of the most fundamental principles of neuroplasticity is that “cells that fire together, wire together.” This is called synaptic plasticity. Think of it like creating a path in a grassy field. The first time you walk it, it’s tough going. But the more you use that same path, the clearer and easier it becomes to follow. In your brain, every time you repeat a thought, feeling, or action, you strengthen the neural connection responsible for it. At the same time, your brain is capable of neurogenesis — growing entirely new brain cells. Positive experiences and healthy habits can encourage this growth, giving you fresh resources to build new, healthier pathways while the old, trauma-worn paths gradually fade from disuse.
Beyond creating new connections, your brain can also change how it uses its existing resources. Epigenetics is a fascinating process where life experiences can act like switches, turning certain genes on or off without altering your DNA. While trauma might flip on genes related to stress and fear, healing practices can help flip them off again. Another process, white matter plasticity, is like upgrading your brain’s pathways from dirt roads to superhighways. As you consistently practice new, healthy behaviors, the brain wraps these important pathways in a fatty coating called myelin. This insulation makes the signals travel much faster and more efficiently, making your new habits feel more automatic and natural over time.
These changes in the brain aren't just happening in the background; they show up in our day-to-day lives. Trauma can leave lasting “imprints” on our brain and stress systems, making it much harder to manage everyday pressures. This is why trauma significantly increases the risk for mental health conditions like Post-Traumatic Stress Disorder (PTSD) and depression. Even without a specific diagnosis, you might notice the effects as heightened anxiety, feeling emotionally numb, or having a shorter fuse than you used to. It’s as if your internal alarm system, once designed to protect you, is now stuck in the “on” position, seeing potential threats everywhere.
When your brain is constantly on high alert, it’s completely exhausting. This state of hypervigilance can cause you to change your behaviors to feel safe. For instance, repeated exposure to traumatic events can rewire our brains, leading us to avoid people, places, or activities that remind us of the experience. It’s also common to look for ways to quiet this internal noise, which is why many people turn to coping mechanisms like alcohol to find temporary relief. This isn't a sign of weakness; it's a sign that your brain is trying to find a way to cope with an overwhelming amount of stress and fear.
Trauma can make emotional regulation a struggle.
Emotional regulation is our ability to manage and respond to emotional experiences in a healthy way.
Trauma can disrupt this process. It can lead to an overactive amygdala (the part of the brain that governs fear responses) and underactivity in the prefrontal cortex (which helps us control emotions and make rational decisions.) This imbalance can result in heightened emotional reactions and difficulty managing stress.
Having a history of trauma can result in intense feelings –– of anxiety, depression, or anger. We may struggle to calm down once we’re upset, or grapple with persistent feelings of sadness or worry. These symptoms demonstrate the changes trauma causes in specific brain regions involved in emotional regulation.
Neuroimaging studies have found alterations in the anterior cingulate cortex (which plays a key role in emotion processing and regulation) and in the insula (involved in our awareness of our emotional states).Healing involves restoring balance within these neural circuits — helping us regain control over our emotions.
Cognition is an umbrella term for the mental processes that make our lives happen, from recognizing familiar faces to solving complex problems. It involves various functions such as attention, memory, and decision-making — all of which trauma impairs.
People who have experienced trauma often report difficulties with attention: they struggle to focus or are easily distracted. Memory issues are also common, including challenges in recalling specific details about events or learning new information. Decision-making can become overwhelming; we avoid making choices altogether or act impulsively instead.
The prefrontal cortex — a region involved in executive functions like decision-making and impulse control — can be affected by trauma. Similarly, prolonged trauma-related stress may cause shrinkage in the hippocampus, an area crucial for memory formation and retrieval.
If you often struggle with cognitive or emotional tasks that others find easy, trauma could play a role.
“Executive functions” might sound like a term for a CEO, but it’s really about the management skills our brain uses every day. Think of it as your brain's control panel for planning, organizing, staying focused, and managing impulses. When trauma affects the prefrontal cortex—the brain's command center—these skills can take a hit. This can make it tough to follow through on plans, switch between tasks, or resist acting on a sudden urge. Research shows that trauma can lead to lasting difficulties with these skills, including working memory and the ability to control impulses. It’s not a personal failing; it's a neurological response to overwhelming experiences, making everyday decision-making feel like a monumental effort.
Experiencing trauma doesn't just affect emotional regulation and cognitive functions. It can also increase your risk for mental illnesses — much as an untreated wound can make us more susceptible to infections.
There’s a strong link between trauma and an increased risk for post-traumatic stress disorder (PTSD), depression, and substance abuse disorders. For instance, individuals who have experienced traumatic events are up to six times more likely to develop PTSD — a condition characterized by intrusive memories, avoidance behaviors, negative changes in mood and cognition, and hyperarousal or reactivity.
Underlying these are changes to those key brain regions — the amygdala, prefrontal cortex, and hippocampus — as well as disruptions to brain chemicals that regulate mood and reward.
What’s more, trauma can lead to dysregulation of the body's stress response system, the hypothalamic-pituitary-adrenal (HPA) axis, resulting in elevated levels of the stress hormone cortisol. Over time, this can contribute to depressive symptoms. Similarly, changes in dopamine — a neurotransmitter involved in reward processing — may make us more vulnerable to substance abuse after trauma. If any of this sounds like you, it’s okay to seek out professional help. You deserve to heal!
Have you ever felt like you were watching your life from outside your own body, as if it were a movie? This experience is known as dissociation, and it’s a common response to trauma. Think of it as your brain’s emergency escape hatch. When an experience is too overwhelming or painful to process, the brain can create a sense of distance to protect you. This feeling of being disconnected from your body, thoughts, or surroundings is a powerful coping mechanism. It’s not a flaw or a weakness; it’s a testament to your mind’s incredible ability to endure the unbearable by temporarily checking out.
This disconnection isn't just mental; it has a profound physical component. Dissociation can make it difficult to be aware of your body's internal signals—a sense known as interoceptive awareness. You might not notice you're hungry until you're starving, or realize you're exhausted until you can barely stand. This happens because, for many trauma survivors, internal bodily sensations can become linked to traumatic memories. To shield you from reliving that pain, your brain might turn down the volume on these signals. It’s another protective measure, but one that can leave you feeling like a stranger in your own skin, making it hard to practice self-care.
Living with this disconnect can be challenging, but it’s important to remember that these neural pathways aren't permanent. Trauma can create overactive or unhelpful neural routes that keep us stuck in these patterns, but our brains are capable of change. The first step toward reconnecting with your body is simply acknowledging this separation without judgment. Practices like mindful drinking or gentle body-scan meditations can help you slowly and safely tune back into your body’s signals. By building new, healthier pathways, you can begin to feel more present and grounded in your own experience, reclaiming the connection that trauma tried to sever.
While trauma can lead to significant changes in the brain, it's crucial to remember that our brains are not static. They possess a remarkable ability for change and growth, called neuroplasticity.
Just as traumatic experiences can alter our brain, positive experiences and interventions can help reshape it.
Research on neuroplasticity provides hope for trauma survivors. Therapeutic interventions like cognitive behavioral therapy (CBT), eye movement desensitization and reprocessing (EMDR), and mindfulness-based practices have been shown to promote healing.
These therapies illustrate how understanding neuroscience can inform effective treatment strategies. They offer hope — and they show us that while trauma may change our brains, we have the power to change them back.
Just as physical therapy can help you regain strength after an injury, certain therapeutic approaches can help your brain heal and form new, healthier pathways. This isn't just about talking through your problems; it's about actively engaging in practices that leverage neuroplasticity to your advantage. These methods provide structured ways to process traumatic memories, manage overwhelming emotions, and develop new coping skills. By consistently engaging in these therapies, you can help your brain move out of a constant state of high alert and into a place of safety and balance, effectively rewiring the circuits that were impacted by trauma.
Cognitive Behavioral Therapy, or CBT, is a practical, goal-oriented approach that helps you identify and challenge negative thought patterns and behaviors. After a traumatic experience, it’s common to get stuck in cycles of thinking that reinforce fear and anxiety. CBT gives you the tools to break these cycles. It works by helping you develop healthier thought patterns, which can strengthen connections within the prefrontal cortex — the part of your brain responsible for rational thinking and decision-making. By changing your thoughts, you can change how you feel and react, empowering you to respond to triggers in a more balanced way.
Mindfulness is the practice of paying attention to the present moment without judgment. For those of us healing from trauma, our minds can often be stuck in the past or worrying about the future. Mindfulness-based treatments gently guide your attention back to the here and now, which can be incredibly grounding. Practices like meditation, deep breathing, and body scans help reduce stress and calm an overactive nervous system. This focus on present-moment awareness doesn't just feel good; it actively promotes overall brain health and helps create a sense of inner peace and stability amidst the chaos of recovery.
Healing from trauma is not a journey you have to take alone. In fact, safe and supportive relationships are one of the most powerful catalysts for recovery. When we connect with people who make us feel seen, heard, and valued, it sends a powerful signal to our nervous system that we are safe. These connections can be with friends, family, a partner, or a therapist. Healthy relationships provide a secure base from which we can explore difficult emotions and experiences. They act as a buffer against stress and remind us that we are not defined by what happened to us, fostering a sense of belonging and hope.
A helpful framework for understanding the power of relationships in healing is the "3 C's": Connect, Co-Regulate, and Co-Reflect. Connection is about forming strong, trusting bonds. Co-regulation is the process of calming your nervous system through interaction with a safe person — think of a soothing conversation or a comforting hug. Co-reflection involves making sense of your experiences with someone you trust. Research shows that strong, supportive relationships can help protect the brain from the harmful effects of trauma, creating an environment where healing is not just possible, but probable.
While therapy and relationships are crucial, the small choices you make every day also play a significant role in your brain's ability to heal. Think of these lifestyle changes as the foundational support system for your recovery. Things like how you sleep, move your body, and nourish yourself directly impact your brain's chemistry and structure. By adopting habits that promote overall well-being, you create an internal environment that is ripe for healing. These consistent, positive actions can help regulate your nervous system, reduce inflammation, and support the growth of new neural connections, making your therapeutic work even more effective.
Never underestimate the healing power of a good night's sleep. While you rest, your brain is hard at work repairing cells, consolidating memories, and clearing out toxins. Sleep is essential for brain growth and recovery, helping to strengthen the pathways that send information between brain cells. Alongside rest, regular physical activity is a game-changer for mental health. Exercise like running or yoga releases endorphins, which are natural mood lifters, and helps reduce levels of stress hormones. Moving your body is a powerful way to process stored tension and reconnect with yourself in a positive, empowering way.
Your environment — both internal and external — can either support or hinder your healing process. Creating a supportive environment means intentionally cultivating spaces, relationships, and mindsets that make you feel safe and nurtured. This could mean setting boundaries with certain people, decluttering your living space to create a sense of calm, or curating the content you consume online. It’s about making conscious choices that protect your energy and promote peace. This isn't about avoiding the world, but about building a personal sanctuary that gives your nervous system a chance to rest and your brain the space it needs to heal.
Two powerful ways to shape your internal environment are practicing gratitude and building community. Gratitude is more than just saying "thank you"; it's a practice that trains your brain to look for the positive, which can help you stay hopeful even on difficult days. You can start by simply thinking of three things you're thankful for each morning. At the same time, connecting with others through healthy friendships or volunteering can provide a profound sense of purpose and belonging. These acts of connection remind you that you are part of something larger than yourself, which is an incredibly powerful force for healing.
Remember: our brains are shaped by experiences, but they're also primed for growth and transformation. Trauma changes our brain –– but healing can, too!
With resilience, therapeutic interventions, and the remarkable power of neuroplasticity on our side, healing is within reach.
Trauma can significantly alter the brain's structure and function, but it doesn't write our destiny.
Are the changes to my brain and personality after trauma permanent? This is such an important question, and the hopeful answer is no, they are not permanent. While trauma can create deep-seated patterns in the brain that make you feel like a different person, these pathways aren't set in stone. Your brain has an incredible ability to adapt and rewire itself throughout your life, a process called neuroplasticity. Through intentional healing practices, you can create new, healthier neural connections, helping your brain learn that it's safe again.
Why do I feel so jumpy and on edge all the time now? That feeling of being constantly on high alert is a common aftereffect of trauma. It happens because the brain's alarm system, the amygdala, gets stuck in overdrive. It learned from the traumatic experience that danger could be anywhere, so it keeps your body flooded with stress hormones to be ready for a threat, even when there isn't one. This state, known as hypervigilance, is exhausting, but it's your brain's attempt to protect you. Healing involves gently teaching this part of your brain that it can stand down and rest.
You mentioned trauma is an 'adaptation.' Does that mean my brain isn't actually damaged? Exactly. It's a powerful shift in perspective to see these changes not as damage, but as your brain's clever adaptations for survival. A heightened sense of alert or a quickness to react weren't flaws; they were features that helped you get through an incredibly difficult time. Viewing these traits as survival strategies, rather than defects, can be a more compassionate way to approach your healing journey. You're not broken; you're a survivor whose brain did what it had to do.
It feels like I'm just 'stuck' in my trauma. How can my brain actually change? Feeling stuck is completely understandable. The neural pathways created by trauma can feel like deep ruts that are hard to get out of. The key is neuroplasticity. Think of it like creating new paths in a field. At first, the old, trauma-worn path is the easiest to take. But every time you engage in a healing activity—whether it's a therapy session, a mindfulness practice, or a safe conversation—you start walking a new path. The more you use these new, healthier pathways, the stronger they become, while the old ones gradually fade from disuse.
Besides therapy, what are some practical things I can do to support my brain's healing? Therapy is a cornerstone of healing, but your daily habits are incredibly important, too. Prioritizing sleep is one of the best things you can do, as your brain does major repair work while you rest. Regular physical movement, like a walk or some gentle yoga, helps process stored stress hormones and reconnect you with your body. Also, creating a safe and calming personal environment can give your nervous system a much-needed break, signaling to your brain that it's okay to relax.

Explore the fascinating neuroscience of self-esteem and self-confidence in this article, as we follow Sam, a successful executive grappling with social anxiety. Discover how understanding the distinct brain regions and mechanisms tied to these aspects of our psyche can empower us to handle stress, change unhealthy habits, and enhance our overall well-being.
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually, with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet millions of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
Meet Sam, a 35-year-old executive, wallflowering it at a bustling party. He's a wizard with spreadsheets but finds social situations a whirlpool of anxiety. To calm his nerves, he drinks — a coping strategy that’s starting to become problematic.
Sam’s situation allows us to see where self-esteem and self-confidence collide. While these terms — self-esteem and self-confidence — are often used interchangeably in conversation, they are different.
At their root, confidence comes from the Latin fidere — to trust. Esteem, on the other hand, stems from the Latin aestimare, which means to value or appraise.
Self-esteem refers to trusting our own abilities or knowledge; self-esteem alludes to our own self-worth.
In this article, we’ll explore Sam’s story and continue to tease out the differences between self-esteem and self-confidence.
While self-esteem is defined as our overall self-worth and value, self-confidence relates to our trust in our own abilities, qualities, skills, or judgment.
Here are other key, albeit nuanced, differences:
It is possible to have both self-confidence as a worker and low self-esteem as a person. We don’t need a healthy self-esteem to have the self-confidence to meet life's challenges and participate in enjoyable, rewarding activities.

While they don’t correspond to different brain areas, self-esteem and self-confidence do involve different regions of the brain.
If we think back to Sam, professionally, he brims with self-confidence — he’s got a firm belief in his abilities derived from his success as an executive. This aspect of his persona, likely rooted in his posterior parietal cortex, allows him to navigate his job with assurance and poise.
Although the research is ongoing, the posterior parietal cortex is believed to be one of the regions and linked to self-confidence. It’s involved in perceptual decision-making, including self-related decisions (like whether to trust ourselves to accomplish something).
When Sam’s thrown into a social situation, a setting he’s less familiar with, his self-confidence wavers. Perhaps he flashes back to the embarrassing thing he said at the company party, which reinforced his negative self-image in social settings. Maybe he works too-long hours, leading to loneliness and isolation — and making him feel especially inept at parties. This lack of belief in his social skills triggers his anxiety, leading him to seek comfort in alcohol.
Self-esteem is linked to the medial prefrontal cortex and the insula. What’s fascinating is that the insula shows increased prediction error responses in those of us with low self-esteem, suggesting its role in self-esteem fluctuations.
A Dartmouth study found that individuals exhibiting a robust white matter connection between the medial prefrontal cortex (an area of the brain involved in self-awareness) and the ventral striatum (a region associated with feelings of reward) tend to demonstrate higher levels of enduring self-esteem.
Both self-esteem and self-confidence involve our perception of ourselves. Recognizing their distinct but interconnected relationship can help Sam — and all of us — find healthier strategies to handle uncomfortable situations.
After all, our brain is malleable, thanks to neuroplasticity — the brain's remarkable ability to reorganize itself by forming new neural connections.
Understanding the science of self-confidence can be a game-changer in our quest to be our best selves.
Each time we successfully accomplish a task, our brain responds by releasing dopamine, a neurotransmitter associated with pleasure and reward. This dopamine surge reinforces our belief in our abilities, bolstering our self-confidence.
Studies show that visualizing our success can stimulate the same brain regions, promoting self-confidence. This implies that mental rehearsal — envisioning ourselves mastering tasks — can stimulate the same dopamine pathways and, in turn, enhance our self-confidence. It's a fascinating instance of mind over matter: we can consciously utilize our brain's inherent mechanisms to foster self-confidence.
Understanding the ways our brain works helps us help ourselves where we most need it. For instance, if Sam starts wants to can navigate social gatherings without resorting to excessive drinking, he can visualize himself telling an excellent joke to a group at a party, or he can attend networking workshops (both of which bolster his self-confidence). He can also work on accepting himself regardless of his social prowess (boosting his self-esteem).
With these insights, let's outline a few practical steps to build healthier habits:
So there you have it! Understanding the science behind self-confidence and self-esteem can be seriously beneficial. By consistently practicing positive self-perception and self-compassion, we can shape our brain's neural pathways to naturally encourage healthier self-esteem.
We're all capable of transforming our brains and, by extension, our lives. Let's embrace this empowering journey, one neural pathway at a time.
Meet Sam, a 35-year-old executive, wallflowering it at a bustling party. He's a wizard with spreadsheets but finds social situations a whirlpool of anxiety. To calm his nerves, he drinks — a coping strategy that’s starting to become problematic.
Sam’s situation allows us to see where self-esteem and self-confidence collide. While these terms — self-esteem and self-confidence — are often used interchangeably in conversation, they are different.
At their root, confidence comes from the Latin fidere — to trust. Esteem, on the other hand, stems from the Latin aestimare, which means to value or appraise.
Self-esteem refers to trusting our own abilities or knowledge; self-esteem alludes to our own self-worth.
In this article, we’ll explore Sam’s story and continue to tease out the differences between self-esteem and self-confidence.
While self-esteem is defined as our overall self-worth and value, self-confidence relates to our trust in our own abilities, qualities, skills, or judgment.
Here are other key, albeit nuanced, differences:
It is possible to have both self-confidence as a worker and low self-esteem as a person. We don’t need a healthy self-esteem to have the self-confidence to meet life's challenges and participate in enjoyable, rewarding activities.

While they don’t correspond to different brain areas, self-esteem and self-confidence do involve different regions of the brain.
If we think back to Sam, professionally, he brims with self-confidence — he’s got a firm belief in his abilities derived from his success as an executive. This aspect of his persona, likely rooted in his posterior parietal cortex, allows him to navigate his job with assurance and poise.
Although the research is ongoing, the posterior parietal cortex is believed to be one of the regions and linked to self-confidence. It’s involved in perceptual decision-making, including self-related decisions (like whether to trust ourselves to accomplish something).
When Sam’s thrown into a social situation, a setting he’s less familiar with, his self-confidence wavers. Perhaps he flashes back to the embarrassing thing he said at the company party, which reinforced his negative self-image in social settings. Maybe he works too-long hours, leading to loneliness and isolation — and making him feel especially inept at parties. This lack of belief in his social skills triggers his anxiety, leading him to seek comfort in alcohol.
Self-esteem is linked to the medial prefrontal cortex and the insula. What’s fascinating is that the insula shows increased prediction error responses in those of us with low self-esteem, suggesting its role in self-esteem fluctuations.
A Dartmouth study found that individuals exhibiting a robust white matter connection between the medial prefrontal cortex (an area of the brain involved in self-awareness) and the ventral striatum (a region associated with feelings of reward) tend to demonstrate higher levels of enduring self-esteem.
Both self-esteem and self-confidence involve our perception of ourselves. Recognizing their distinct but interconnected relationship can help Sam — and all of us — find healthier strategies to handle uncomfortable situations.
After all, our brain is malleable, thanks to neuroplasticity — the brain's remarkable ability to reorganize itself by forming new neural connections.
Understanding the science of self-confidence can be a game-changer in our quest to be our best selves.
Each time we successfully accomplish a task, our brain responds by releasing dopamine, a neurotransmitter associated with pleasure and reward. This dopamine surge reinforces our belief in our abilities, bolstering our self-confidence.
Studies show that visualizing our success can stimulate the same brain regions, promoting self-confidence. This implies that mental rehearsal — envisioning ourselves mastering tasks — can stimulate the same dopamine pathways and, in turn, enhance our self-confidence. It's a fascinating instance of mind over matter: we can consciously utilize our brain's inherent mechanisms to foster self-confidence.
Understanding the ways our brain works helps us help ourselves where we most need it. For instance, if Sam starts wants to can navigate social gatherings without resorting to excessive drinking, he can visualize himself telling an excellent joke to a group at a party, or he can attend networking workshops (both of which bolster his self-confidence). He can also work on accepting himself regardless of his social prowess (boosting his self-esteem).
With these insights, let's outline a few practical steps to build healthier habits:
So there you have it! Understanding the science behind self-confidence and self-esteem can be seriously beneficial. By consistently practicing positive self-perception and self-compassion, we can shape our brain's neural pathways to naturally encourage healthier self-esteem.
We're all capable of transforming our brains and, by extension, our lives. Let's embrace this empowering journey, one neural pathway at a time.

Ever wondered how a simple Himalayan salt lamp can transform your well-being? Dive into our latest blog post that brings the surprising benefits of salt lamps to light.
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually, with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet millions of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
Picture this: You've come home after a long day at work. Emails flooded your inbox, your commute was a nightmare, and your stress levels were through the roof. Instead of crashing into bed right away, you decide to take a breather. You switch on your salt lamp, watch as the soft, warm light fills your room, and immediately start to feel your tension melting away.
Ahh ... relaxation! But what exactly is going on here? Is there something about these chunky hunks of pinkish-orange rock that makes them more than just a pretty night light? Let's find out!
Salt lamps are usually made from Himalayan pink salt, a rock salt from the Punjab region in Pakistan. They emit a soft, warm glow when lit, but their benefits may go beyond mere aesthetics: they interact with ions in the atmosphere.
Air contains both positive and negative ions. These aren't just abstract physics concepts — they can impact how we feel and function. Electronics, like your phone or computer, create positive ions. An excess of these might contribute to feelings of stress and lethargy.
Salt lamps, on the other hand, are believed to produce negative ions. These are the same type of ions found abundantly in nature, particularly around waterfalls or after a thunderstorm. These settings often leave us feeling refreshed and revitalized — no wonder people flock to Niagara Falls!
But does a salt lamp really generate enough negative ions to make a noticeable difference? Truth be told, the jury's still out. Some studies suggest that the concentration of negative ions may be too low to have a significant impact — more research is needed to confirm these claims.
Regardless of the ion theory, there's another angle to consider: the power of light. Salt lamps emit a warm, comforting light that some people find calming. This relates to a well-established form of therapy called light therapy, which has been shown to help regulate mood and sleep.
Though salt lamps aren't specifically designed for light therapy, the glow they emit can simulate a sunrise or sunset. This may help signal our brains to wind down and prepare for sleep, potentially improving sleep quality.
Salt lamps — whether or not they pump out enough negative ions to make a noticeable difference — could also help us on our journey to cut back on or quit alcohol.
Changing a habit as ingrained as drinking often involves altering the environment in which we live. For many people, coming home from work might be directly associated with cracking open a beer or pouring a glass of wine. Breaking that cycle may mean changing the cues we associate with drinking.
Here's where a Himalayan salt lamp comes in. Switching on the lamp creates a shift in atmosphere — one that can become associated with booze-free relaxation and healing.
The warm, dim light of a salt lamp can also play a role in your bedtime routine, signaling your brain to prepare for sleep. Improved sleep can have a profound impact on overall well-being, reducing the risk of falling back on alcohol as a coping mechanism.
Now that we've brushed up on the science behind salt lamps, let's talk about incorporating them into your daily routine to help you get the most out of them.

If you would like to use your salt lamp as part of your journey in cutting back or quitting alcohol, here are some ideas to try:
Salt lamps are intriguing and can potentially offer some benefits, but they're not a silver bullet for health and well-being. They should be seen as a complement to a healthy lifestyle, not a replacement for good nutrition, exercise, and proper sleep.
But while a Himalayan salt lamp is not a magic stress reducer or cravings buster, it can be a part of a holistic approach. Sometimes, the smallest changes can lead the way. So go ahead, switch on your salt lamp, take a deep breath, and embrace the calm. After all, we could all use a bit of light in our lives, couldn't we?
Picture this: You've come home after a long day at work. Emails flooded your inbox, your commute was a nightmare, and your stress levels were through the roof. Instead of crashing into bed right away, you decide to take a breather. You switch on your salt lamp, watch as the soft, warm light fills your room, and immediately start to feel your tension melting away.
Ahh ... relaxation! But what exactly is going on here? Is there something about these chunky hunks of pinkish-orange rock that makes them more than just a pretty night light? Let's find out!
Salt lamps are usually made from Himalayan pink salt, a rock salt from the Punjab region in Pakistan. They emit a soft, warm glow when lit, but their benefits may go beyond mere aesthetics: they interact with ions in the atmosphere.
Air contains both positive and negative ions. These aren't just abstract physics concepts — they can impact how we feel and function. Electronics, like your phone or computer, create positive ions. An excess of these might contribute to feelings of stress and lethargy.
Salt lamps, on the other hand, are believed to produce negative ions. These are the same type of ions found abundantly in nature, particularly around waterfalls or after a thunderstorm. These settings often leave us feeling refreshed and revitalized — no wonder people flock to Niagara Falls!
But does a salt lamp really generate enough negative ions to make a noticeable difference? Truth be told, the jury's still out. Some studies suggest that the concentration of negative ions may be too low to have a significant impact — more research is needed to confirm these claims.
Regardless of the ion theory, there's another angle to consider: the power of light. Salt lamps emit a warm, comforting light that some people find calming. This relates to a well-established form of therapy called light therapy, which has been shown to help regulate mood and sleep.
Though salt lamps aren't specifically designed for light therapy, the glow they emit can simulate a sunrise or sunset. This may help signal our brains to wind down and prepare for sleep, potentially improving sleep quality.
Salt lamps — whether or not they pump out enough negative ions to make a noticeable difference — could also help us on our journey to cut back on or quit alcohol.
Changing a habit as ingrained as drinking often involves altering the environment in which we live. For many people, coming home from work might be directly associated with cracking open a beer or pouring a glass of wine. Breaking that cycle may mean changing the cues we associate with drinking.
Here's where a Himalayan salt lamp comes in. Switching on the lamp creates a shift in atmosphere — one that can become associated with booze-free relaxation and healing.
The warm, dim light of a salt lamp can also play a role in your bedtime routine, signaling your brain to prepare for sleep. Improved sleep can have a profound impact on overall well-being, reducing the risk of falling back on alcohol as a coping mechanism.
Now that we've brushed up on the science behind salt lamps, let's talk about incorporating them into your daily routine to help you get the most out of them.

If you would like to use your salt lamp as part of your journey in cutting back or quitting alcohol, here are some ideas to try:
Salt lamps are intriguing and can potentially offer some benefits, but they're not a silver bullet for health and well-being. They should be seen as a complement to a healthy lifestyle, not a replacement for good nutrition, exercise, and proper sleep.
But while a Himalayan salt lamp is not a magic stress reducer or cravings buster, it can be a part of a holistic approach. Sometimes, the smallest changes can lead the way. So go ahead, switch on your salt lamp, take a deep breath, and embrace the calm. After all, we could all use a bit of light in our lives, couldn't we?

Stress is impossible to avoid, but we can learn to better manage it through different meditations. Here’s a closer look at some of the most popular and effective meditations for stress relief.
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually, with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet millions of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
How do you manage your stress? Maybe you regularly get a massage, journal, use different supplements, or try to manage it through physical activity like exercise. All of these are great tools. But if you’re wondering how to reduce stress or looking for effective stress management techniques and have never tried meditation, it’s probably worth giving it a shot.
Thankfully, many different types of meditations for stress relief are available to us. If you’ve tried one and it didn’t work for you, you can always try something else! The important thing is to find one that works and be consistent with it. So, what are some ways to reduce stress with meditation? And what are the best meditations for stress relief? Let’s dive in.

One reason meditation is so effective for stress relief is that it triggers our body’s relaxation response. In fact, it has the opposite effect of stress by activating our parasympathetic nervous system — a network of nerves that relaxes our body after periods of stress or danger.
Whenever we’re under a great amount of mental or physical stress, our body goes into “flight or fright” mode, releasing the stress hormone cortisol. Over time, chronic stress can lead to inflammation, high blood pressure, and physical damage in every part of our body. It also takes a toll on our emotional and mental health, putting us at greater risk for depression, anxiety, and sleep issues.
Meditation helps restore our body to a calm state, lowering our heart rate and blood pressure. Numerous studies have shown that meditation is a particularly effective stress-management tool, helping reprogram our brain and increase our stress resiliency. In fact, one study found that meditation helped alleviate stress after just eight weeks of regular practice.
Similarly, research has shown that meditation may also improve symptoms of stress-related conditions, such as irritable bowel syndrome, post-traumatic stress disorder, and fibromyalgia.
While there’s no one right way to go about meditating, several meditations for stress relief have proven to be particularly popular and effective. Here are some of them:
Mantra meditation is a simple meditation that has proven effective as a stress relief technique. Many people find that mantra meditation is a good starting point as it involves choosing a simple word or phrase that we can repeat to ourselves out loud or silently. This can be a spiritual word like “Om” or a word or phrase such as “Calm” or “I am at peace.” It doesn’t matter what word, sound, or phrase we choose — just that we’re comfortable with it.
The goal is to repeat the mantra for several minutes, focusing only on the sound and feel of our mantra — nothing else. If you find other thoughts creeping into your head, try not to berate yourself, but instead gently redirect your focus back to your mantra. It’s best to practice this meditation in a quiet, comfortable place.
Mindfulness meditation is one of the most popular meditations for stress relief. It’s a simple practice that involves being fully present with what we’re experiencing in the present moment. It can be particularly beneficial in helping us slow down our racing thoughts, let go of negativity, and calm our mind and body. The goal is to be focused solely on “the now” by acknowledging and accepting our thoughts, feelings, and sensations without judgment.
For instance, we can practice mindfulness by closing our eyes, taking a couple of deep breaths, and noticing any thoughts that start arising. The goal isn’t to stop our thoughts or judge them, but to observe and accept them. It can be helpful to imagine our thoughts as clouds passing by: our job is to just watch them float by. If we find ourselves starting to judge our thoughts, try not to be hard on yourself. Instead, return to your breath and refocus on the present moment.

Similar to mindfulness, the body scan meditation helps bring awareness to our body. Oftentimes, our body carries stress in the form of tension that we’re not even aware of. By mentally scanning our body, we’re bringing awareness to every single part of our body, noticing any aches, pains, tensions, or general discomfort. The goal isn’t to relieve the pain completely, but to get familiar with it and learn from it so we can better manage it.
We can start by bringing our attention down to our feet and observing any sensations. If there’s noticeable pain, acknowledge it and any thoughts or emotions that accompany it, and then gently breathe through it. Visualize the tension leaving your body. Continue doing this for each area of your body, gradually moving up from your feet through the top of your head.
Breathing meditation is another popular form of meditation for stress release, enjoyed by many for its ease and simplicity. Our breath provides a natural rhythm that we can focus on and get lost in. Box breathing in particular can help produce relaxation. We can practice box breathing by slowly breathing in through our nose and counting to four, holding our breath for four seconds, and slowly exhaling through our mouth for four seconds. Hold another four seconds, then inhale and start the cycle again.
We can practice breathing meditation for a few minutes at a time, or for longer if we’re trying to relax, such as in the evening before going to bed.
The loving-kindness meditation is also simple to perform and can be used to reduce stress and boost well-being. During this meditation, we focus on sending good and loving thoughts and energy toward ourselves and others. For instance, we might wish ourselves peace, happiness, and contentment. We can even repeat different phrases to ourselves, such as “May I be happy,” or “May I be healthy, peaceful, and strong,” or “May I give and receive appreciation today.”
We can start by focusing on ourselves and then extending these same thoughts and feelings toward our loved ones and the world at large. Try starting with a spouse, child, parent, or friend. Stay in the moment and try to savor your gratitude and love for them. Repeat any phrases you need to for as long as you want.
Walking meditation is particularly effective because it combines the benefits of meditation with the benefits of exercise. Plus, if we walk outside, we also benefit from being in nature, which is a natural stress-reliever.
The key is to remove distractions and get moving. You can walk at whatever pace you like, but try to leave your phone behind. Instead, tune into the sights and sounds around you, or simply allow your mind to wander. Walking medication can also be a good meditation to start with for those of us without much meditation experience. It’s especially useful for people who like to stay active or who might feel stressed by the idea of sitting in quiet and stillness.
Those of us who don’t enjoy walking but still want to move might try incorporating qigong, tai chi, or yoga. These can also help produce a meditative state of mind.
There are many different types of meditations out there, but these are some of the most popular and effective meditations for stress relief. Keep in mind that even brief, 10-minute meditations can be beneficial. Again, the goal is to find a meditation that works best for us, and then stick with it. Consistency is key!
Finally, if you’re having trouble managing your stress and find yourself turning to alcohol to help you cope, consider joining Reframe. We can help you cut back on your drinking and put you on track to develop healthier lifestyle habits, including better ways to manage stress.
How do you manage your stress? Maybe you regularly get a massage, journal, use different supplements, or try to manage it through physical activity like exercise. All of these are great tools. But if you’re wondering how to reduce stress or looking for effective stress management techniques and have never tried meditation, it’s probably worth giving it a shot.
Thankfully, many different types of meditations for stress relief are available to us. If you’ve tried one and it didn’t work for you, you can always try something else! The important thing is to find one that works and be consistent with it. So, what are some ways to reduce stress with meditation? And what are the best meditations for stress relief? Let’s dive in.

One reason meditation is so effective for stress relief is that it triggers our body’s relaxation response. In fact, it has the opposite effect of stress by activating our parasympathetic nervous system — a network of nerves that relaxes our body after periods of stress or danger.
Whenever we’re under a great amount of mental or physical stress, our body goes into “flight or fright” mode, releasing the stress hormone cortisol. Over time, chronic stress can lead to inflammation, high blood pressure, and physical damage in every part of our body. It also takes a toll on our emotional and mental health, putting us at greater risk for depression, anxiety, and sleep issues.
Meditation helps restore our body to a calm state, lowering our heart rate and blood pressure. Numerous studies have shown that meditation is a particularly effective stress-management tool, helping reprogram our brain and increase our stress resiliency. In fact, one study found that meditation helped alleviate stress after just eight weeks of regular practice.
Similarly, research has shown that meditation may also improve symptoms of stress-related conditions, such as irritable bowel syndrome, post-traumatic stress disorder, and fibromyalgia.
While there’s no one right way to go about meditating, several meditations for stress relief have proven to be particularly popular and effective. Here are some of them:
Mantra meditation is a simple meditation that has proven effective as a stress relief technique. Many people find that mantra meditation is a good starting point as it involves choosing a simple word or phrase that we can repeat to ourselves out loud or silently. This can be a spiritual word like “Om” or a word or phrase such as “Calm” or “I am at peace.” It doesn’t matter what word, sound, or phrase we choose — just that we’re comfortable with it.
The goal is to repeat the mantra for several minutes, focusing only on the sound and feel of our mantra — nothing else. If you find other thoughts creeping into your head, try not to berate yourself, but instead gently redirect your focus back to your mantra. It’s best to practice this meditation in a quiet, comfortable place.
Mindfulness meditation is one of the most popular meditations for stress relief. It’s a simple practice that involves being fully present with what we’re experiencing in the present moment. It can be particularly beneficial in helping us slow down our racing thoughts, let go of negativity, and calm our mind and body. The goal is to be focused solely on “the now” by acknowledging and accepting our thoughts, feelings, and sensations without judgment.
For instance, we can practice mindfulness by closing our eyes, taking a couple of deep breaths, and noticing any thoughts that start arising. The goal isn’t to stop our thoughts or judge them, but to observe and accept them. It can be helpful to imagine our thoughts as clouds passing by: our job is to just watch them float by. If we find ourselves starting to judge our thoughts, try not to be hard on yourself. Instead, return to your breath and refocus on the present moment.

Similar to mindfulness, the body scan meditation helps bring awareness to our body. Oftentimes, our body carries stress in the form of tension that we’re not even aware of. By mentally scanning our body, we’re bringing awareness to every single part of our body, noticing any aches, pains, tensions, or general discomfort. The goal isn’t to relieve the pain completely, but to get familiar with it and learn from it so we can better manage it.
We can start by bringing our attention down to our feet and observing any sensations. If there’s noticeable pain, acknowledge it and any thoughts or emotions that accompany it, and then gently breathe through it. Visualize the tension leaving your body. Continue doing this for each area of your body, gradually moving up from your feet through the top of your head.
Breathing meditation is another popular form of meditation for stress release, enjoyed by many for its ease and simplicity. Our breath provides a natural rhythm that we can focus on and get lost in. Box breathing in particular can help produce relaxation. We can practice box breathing by slowly breathing in through our nose and counting to four, holding our breath for four seconds, and slowly exhaling through our mouth for four seconds. Hold another four seconds, then inhale and start the cycle again.
We can practice breathing meditation for a few minutes at a time, or for longer if we’re trying to relax, such as in the evening before going to bed.
The loving-kindness meditation is also simple to perform and can be used to reduce stress and boost well-being. During this meditation, we focus on sending good and loving thoughts and energy toward ourselves and others. For instance, we might wish ourselves peace, happiness, and contentment. We can even repeat different phrases to ourselves, such as “May I be happy,” or “May I be healthy, peaceful, and strong,” or “May I give and receive appreciation today.”
We can start by focusing on ourselves and then extending these same thoughts and feelings toward our loved ones and the world at large. Try starting with a spouse, child, parent, or friend. Stay in the moment and try to savor your gratitude and love for them. Repeat any phrases you need to for as long as you want.
Walking meditation is particularly effective because it combines the benefits of meditation with the benefits of exercise. Plus, if we walk outside, we also benefit from being in nature, which is a natural stress-reliever.
The key is to remove distractions and get moving. You can walk at whatever pace you like, but try to leave your phone behind. Instead, tune into the sights and sounds around you, or simply allow your mind to wander. Walking medication can also be a good meditation to start with for those of us without much meditation experience. It’s especially useful for people who like to stay active or who might feel stressed by the idea of sitting in quiet and stillness.
Those of us who don’t enjoy walking but still want to move might try incorporating qigong, tai chi, or yoga. These can also help produce a meditative state of mind.
There are many different types of meditations out there, but these are some of the most popular and effective meditations for stress relief. Keep in mind that even brief, 10-minute meditations can be beneficial. Again, the goal is to find a meditation that works best for us, and then stick with it. Consistency is key!
Finally, if you’re having trouble managing your stress and find yourself turning to alcohol to help you cope, consider joining Reframe. We can help you cut back on your drinking and put you on track to develop healthier lifestyle habits, including better ways to manage stress.

Ever wondered why an unanswered text from a friend leaves you feeling uneasy? Dive into our latest blog about emotional permanence — the glue that makes our feelings of reassurance in relationships stick.
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually, with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet millions of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
Picture your best friend, partner, or a close family member. Now, imagine them in the middle of a hectic day — they’re juggling calls, wrapping up meetings, and trying to meet a looming deadline. In the middle of all this, you send them a text expressing that you're having a tough day and could use some cheer. They read it but don't reply immediately. Minutes turn into hours, and the response never comes. You start to wonder: “Do they still care about me?”
The psychological concept in play is emotional permanence. Understanding it can help alleviate the anxiety that can arise in situations like the one described above.
Emotional permanence is the understanding that people's emotions — such as their love for you — continue to exist even when they are not immediately observable. In other words, just because someone isn't around to tell you they love you at this very moment doesn't mean they don't care for you anymore.
Emotional permanence is a linchpin in healthy relationships: it ensures trust, creates a sense of security, and strengthens bonds. Understanding this concept can put us at ease when a loved one is not actively showing their affection. Just because we don’t get an immediate response doesn't mean their feelings have changed or they have abandoned us — they might just be having a busy day!
It sounds simple, but this concept is often trickier than it appears. Many of us struggle with feelings of uncertainty about the constancy of others' affections when they're not physically near us.
What causes emotional permanence? The answer lies deep within our brain, in an area known as the prefrontal cortex. This part of the brain is responsible for higher cognitive functions such as decision-making, empathy, and — most importantly for today’s topic — the understanding of permanence.
A child’s first developmental milestone is “object permanence” — an idea that children learn at an early age, usually by the age of two. This is what peek-a-boo is all about: understanding that objects continue to exist even when they vanish out of sight. We learn that things that go out of sight usually don’t disappear for good — now we see it, now we don’t, but we probably will see it again. For example, when mom leaves the room, she hasn't ceased to exist; she's just watering the plants outside
Emotional permanence, in comparison, is a bit more complex. Unlike object permanence, it's not necessarily a milestone that we all hit at a certain age: it continues to develop as we mature, and it’s tied closely to our personal experiences, emotional intelligence, and mental health.
Emotional permanence is the bedrock of our social interactions and emotional stability. Research has shown that it’s a critical component of secure attachment in adults, influencing our friendships, family ties, and romantic relationships. Securely attached adults trust that their loved ones' feelings for them are enduring — even in their absence.
So why do we — with our fully-developed prefrontal cortex — still struggle with this concept at times? Stress, anxiety, and past experiences can often cloud our judgment and lead us to question the stability of people's emotions towards us.
Insecurity, fear of abandonment, or past experiences of unreliable affection can mess with our emotional permanence. It's natural to feel insecure or anxious occasionally, but when these feelings persist, they can become a roadblock in our emotional well-being.
Moreover, humans are social creatures, wired to connect with others. We thrive on reciprocity in our relationships — the mutual exchange of feelings and actions. When this reciprocity is disturbed or doubted (with or without a reason), it can make us question our value in the relationship.
Over time, losing our emotional GPS can lead to abandonment issues. We are left feeling adrift and can end up interpreting every missed phone call or unanswered text as rejection or abandonment.

So what are some ways we can give our emotional permanence a boost? Here are a few ideas that can help:
Emotional permanence is an invisible thread that connects us to our loved ones. With practice and patience, we can cultivate it and foster deeper, healthier relationships
Picture your best friend, partner, or a close family member. Now, imagine them in the middle of a hectic day — they’re juggling calls, wrapping up meetings, and trying to meet a looming deadline. In the middle of all this, you send them a text expressing that you're having a tough day and could use some cheer. They read it but don't reply immediately. Minutes turn into hours, and the response never comes. You start to wonder: “Do they still care about me?”
The psychological concept in play is emotional permanence. Understanding it can help alleviate the anxiety that can arise in situations like the one described above.
Emotional permanence is the understanding that people's emotions — such as their love for you — continue to exist even when they are not immediately observable. In other words, just because someone isn't around to tell you they love you at this very moment doesn't mean they don't care for you anymore.
Emotional permanence is a linchpin in healthy relationships: it ensures trust, creates a sense of security, and strengthens bonds. Understanding this concept can put us at ease when a loved one is not actively showing their affection. Just because we don’t get an immediate response doesn't mean their feelings have changed or they have abandoned us — they might just be having a busy day!
It sounds simple, but this concept is often trickier than it appears. Many of us struggle with feelings of uncertainty about the constancy of others' affections when they're not physically near us.
What causes emotional permanence? The answer lies deep within our brain, in an area known as the prefrontal cortex. This part of the brain is responsible for higher cognitive functions such as decision-making, empathy, and — most importantly for today’s topic — the understanding of permanence.
A child’s first developmental milestone is “object permanence” — an idea that children learn at an early age, usually by the age of two. This is what peek-a-boo is all about: understanding that objects continue to exist even when they vanish out of sight. We learn that things that go out of sight usually don’t disappear for good — now we see it, now we don’t, but we probably will see it again. For example, when mom leaves the room, she hasn't ceased to exist; she's just watering the plants outside
Emotional permanence, in comparison, is a bit more complex. Unlike object permanence, it's not necessarily a milestone that we all hit at a certain age: it continues to develop as we mature, and it’s tied closely to our personal experiences, emotional intelligence, and mental health.
Emotional permanence is the bedrock of our social interactions and emotional stability. Research has shown that it’s a critical component of secure attachment in adults, influencing our friendships, family ties, and romantic relationships. Securely attached adults trust that their loved ones' feelings for them are enduring — even in their absence.
So why do we — with our fully-developed prefrontal cortex — still struggle with this concept at times? Stress, anxiety, and past experiences can often cloud our judgment and lead us to question the stability of people's emotions towards us.
Insecurity, fear of abandonment, or past experiences of unreliable affection can mess with our emotional permanence. It's natural to feel insecure or anxious occasionally, but when these feelings persist, they can become a roadblock in our emotional well-being.
Moreover, humans are social creatures, wired to connect with others. We thrive on reciprocity in our relationships — the mutual exchange of feelings and actions. When this reciprocity is disturbed or doubted (with or without a reason), it can make us question our value in the relationship.
Over time, losing our emotional GPS can lead to abandonment issues. We are left feeling adrift and can end up interpreting every missed phone call or unanswered text as rejection or abandonment.

So what are some ways we can give our emotional permanence a boost? Here are a few ideas that can help:
Emotional permanence is an invisible thread that connects us to our loved ones. With practice and patience, we can cultivate it and foster deeper, healthier relationships

Discover the science-backed power of gratitude to reduce stress and make lasting changes. Learn how gratitude rewires your brain and boosts health — get inspired with 15 journal prompts today. So grab your journal and move into joy!
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually, with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet millions of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
Think of your mind as a garden, with every thought and emotion a seed that you sow. Just as a well-tended garden will blossom, nurturing your mind with gratitude can cultivate a sense of well-being — and empower you to make lasting changes in your life.
In our fast-paced world, stress can often feel overwhelming, leading us to seek relief in harmful coping mechanisms like excessive drinking.
But there’s a better way to get through the rough patches — gratitude.
Practicing gratitude can be a powerful antidote to stress and a catalyst for positive change. These 15 journal prompts can help you along the journey.
Expressing gratitude activates the prefrontal cortex and the ventral striatum, brain regions associated with positive emotions and reward.
The prefrontal cortex, a region responsible for regulating emotions and decision-making, lights up with activity when we practice gratitude. This activation triggers the release of feel-good neurotransmitters like dopamine and serotonin, creating a cascade of positive feelings.
Additionally, expressing gratitude stimulates the ventral striatum, an area linked to pleasure and motivation. It's like pressing a "happiness button" in the brain. As a result, we experience an increased sense of well-being, contentment, and optimism.
The brain is remarkably adaptive and can rewire itself based on our experiences. When we consistently practice gratitude, we strengthen the neural connections associated with positive emotions and reward. This rewiring leads to an enduring positive outlook on life, making us more resilient in the face of challenges.
Not only does gratitude affect the brain — it also influences our overall mental and physical health. Gratitude lowers our levels of stress, anxiety, and depression. It can improve our sleep quality and immune system.
By embracing the science of gratitude, we can tap into our brain's natural capacity for happiness and well-being. It empowers us to reshape our thought patterns, amplify positive emotions — and, ultimately, make lasting changes in our lives.

Incorporating mindfulness into your gratitude practice can enhance its effectiveness. When we are fully present in the moment, we can savor and appreciate even the smallest things in life. Take a deep breath, immerse yourself in the present, and let gratitude flow through you.
We've explored the power of gratitude and provided you with 15 journal prompts — now it's time to take action! Here are three simple yet powerful steps you can take today:
By nurturing gratitude, we can reduce stress, foster well-being, and empower ourselves to make lasting changes — and help us reach our goals to cut back on drinking.
Change takes time, and small steps can lead to significant transformations.
So, grab your journal and immerse yourself in the practice of gratitude. Allow it to transform your perspective, strengthen your resilience, and guide you towards joy.
Think of your mind as a garden, with every thought and emotion a seed that you sow. Just as a well-tended garden will blossom, nurturing your mind with gratitude can cultivate a sense of well-being — and empower you to make lasting changes in your life.
In our fast-paced world, stress can often feel overwhelming, leading us to seek relief in harmful coping mechanisms like excessive drinking.
But there’s a better way to get through the rough patches — gratitude.
Practicing gratitude can be a powerful antidote to stress and a catalyst for positive change. These 15 journal prompts can help you along the journey.
Expressing gratitude activates the prefrontal cortex and the ventral striatum, brain regions associated with positive emotions and reward.
The prefrontal cortex, a region responsible for regulating emotions and decision-making, lights up with activity when we practice gratitude. This activation triggers the release of feel-good neurotransmitters like dopamine and serotonin, creating a cascade of positive feelings.
Additionally, expressing gratitude stimulates the ventral striatum, an area linked to pleasure and motivation. It's like pressing a "happiness button" in the brain. As a result, we experience an increased sense of well-being, contentment, and optimism.
The brain is remarkably adaptive and can rewire itself based on our experiences. When we consistently practice gratitude, we strengthen the neural connections associated with positive emotions and reward. This rewiring leads to an enduring positive outlook on life, making us more resilient in the face of challenges.
Not only does gratitude affect the brain — it also influences our overall mental and physical health. Gratitude lowers our levels of stress, anxiety, and depression. It can improve our sleep quality and immune system.
By embracing the science of gratitude, we can tap into our brain's natural capacity for happiness and well-being. It empowers us to reshape our thought patterns, amplify positive emotions — and, ultimately, make lasting changes in our lives.

Incorporating mindfulness into your gratitude practice can enhance its effectiveness. When we are fully present in the moment, we can savor and appreciate even the smallest things in life. Take a deep breath, immerse yourself in the present, and let gratitude flow through you.
We've explored the power of gratitude and provided you with 15 journal prompts — now it's time to take action! Here are three simple yet powerful steps you can take today:
By nurturing gratitude, we can reduce stress, foster well-being, and empower ourselves to make lasting changes — and help us reach our goals to cut back on drinking.
Change takes time, and small steps can lead to significant transformations.
So, grab your journal and immerse yourself in the practice of gratitude. Allow it to transform your perspective, strengthen your resilience, and guide you towards joy.

Unresolved trauma can feel like a ferocious bear lurking in our lives. Explore eight potent strategies to heal— and tame this 'invisible bear.' From understanding the brain-body connection to harnessing the power of each other, we dive deep into neuroscience-backed methods to reduce stress and enable recovery. Embark on this transformative journey with us.
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually, with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet millions of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
Imagine walking through a beautiful forest: the sun is shining, birds are singing, and it seems that all is well. Suddenly, a bear appears directly in front of you. Your heart races, adrenaline surges through your veins, and your body prepares for fight or flight. This is trauma: an intense response to a deeply distressing event that overwhelms our ability to cope.
Now imagine if that bear followed you home and lurked in every corner of your life. That's how living with unresolved trauma can feel. It can manifest in various ways and affect each of us uniquely — from anxiety and depression to substance abuse to physical illness.
Spotting and understanding our own "invisible bear" is the first step towards healing.
In this article, we'll explore eight potent strategies for taming the beast of trauma and reclaiming control over our lives.
Trauma refers to a deeply distressing or disturbing experience that has profound impacts on our mental, physical, and emotional well-being. This can include events such as abuse, neglect, loss of a loved one, accidents, or exposure to violence or disaster.
When we encounter an event or situation that we perceive as physically or emotionally threatening, and it overwhelms our ability to cope, it can result in trauma. This can lead to long-term consequences: post-traumatic stress disorder (PTSD), anxiety, depression, and challenges with self-regulation — and changes in our brains.
It's essential to remember that trauma is highly subjective — what may be traumatic for one of us may not be for another. Our perception of the event, our personal resilience, and our available support systems can significantly influence the impact of the traumatic event.
The connection between the brain and body is a profound one. Picture it as a bustling two-way highway with constant traffic — our thoughts, feelings, and physiological responses— flowing in both directions.
Our brain, the command center, sends out signals based on our thoughts and emotions. These signals manifest physically as changes in heart rate, blood pressure, and muscle tension. Simultaneously, our body sends feedback to the brain, affecting our emotions and thoughts. This dynamic interaction forms the basis of our responses to stress and trauma.
When we experience trauma or chronic stress, the highway traffic can go into overdrive, with signals often stuck in a "fight or flight" loop. Like a car alarm that won't turn off, our body remains in a state of high alert — leading to chronic stress and health issues.
When this alarm system is repeatedly activated due to ongoing trauma or severe experiences, it can lead to long-term changes in our brain’s structure and function. For instance, research has shown that prolonged exposure to stress hormones can shrink the hippocampus (an area responsible for memory and learning), leading to difficulty in processing memory.
Mindfulness and controlled breathing exercises can guide us like a GPS. They help to slow down the traffic, giving us a chance to exit the stressful "fight or flight" loop and enter a calmer state — known as "rest and digest.”
Meditation can significantly reduce stress and improve mental health. Deep, controlled breathing can lower blood pressure and promote feelings of calm.
Practicing mindfulness helps recalibrate our brain's response to stress, creating harmony between brain and body. Gradually, this can help us cut back on unhealthy coping mechanisms — like excessive drinking — paving the way for lasting change.
Unhealed trauma can also affect our prefrontal cortex, the part of our brain responsible for executive functions like decision-making and impulse control, making it harder for us to manage our emotions.
When dealing with trauma, it's essential to remember we don't have to face it alone. Professional help from therapists or counselors specialized in trauma therapy can be a game-changer on our healing journeys.
Therapists trained in trauma work understand the intricate ways trauma alters our brains and bodies. They use evidence-based therapeutic approaches designed specifically to help individuals process traumatic experiences and foster resilience.
Cognitive Behavioral Therapy (CBT), for instance, helps us identify and change the thought patterns that lead to harmful behaviors or emotions. By reframing negative thoughts, CBT can help reduce symptoms of post-traumatic stress disorder (PTSD) and other trauma-related disorders.
Another powerful tool is Eye Movement Desensitization and Reprocessing (EMDR). This therapy uses guided eye movements to help us process traumatic memories and reduce their long-term effects. This reprocesses traumatic memories, integrating them into our overall life narrative rather than letting them linger as disruptive fragments.
Remember, there's no one-size-fits-all when it comes to therapy; what works for one person might not work for another. Take some time to research the resources available to you that might resonate with you personally.
Triggers are hidden tripwires in our minds. When we encounter one, our brain swiftly recalls past experiences. If it finds a link to a traumatic event, it initiates the stress response, preparing us to "fight or flee."
They are the brain's way of alerting us to potential danger based on past experiences. However, triggers can cause us distress and lead us to unhealthy coping mechanisms. They are unique to each of us.
Understanding our triggers is critical for healing. Recognizing these tripwires and replacing our response to them with healthier alternatives — like deep breathing or taking a brisk walk — can help rewire the brain's reward system, making lasting changes more feasible. But in order to do so, we need to know and track those triggers.

Self-care is not just about bubble baths and spa days; it's about taking intentional actions to care for your physical, mental, and emotional health. It means movement, good food, and enough sleep.
Movement helps promote relaxation. Eating well is also important — just as our body needs nutritious food, so does our brain. Certain nutrients can bolster our brain health, enhance mood, and mitigate stress. A balanced diet rich in omega-3 fatty acids, antioxidants, and vitamins is crucial for optimal brain function.
Sleep is more than recharging. It's the time when our brain processes the day's events, solidifying memories and learning. Improving sleep hygiene gives the brain ample time to process trauma and accelerate healing.
Taking care of our body is taking care of our mind.
Having a strong support system is crucial to healing.
Reach out to trusted friends or family members who can provide emotional support.
Consider joining support groups and connect with others who share similar experiences. It can be incredibly healing — and make you feel less alone.
Expressive therapies — like art therapy or dance/movement therapy — offer creative outlets for expressing and processing emotions related to trauma.
They allow you to communicate feelings that might be too difficult to put into words.
But expressing yourself can take many forms: write down your thoughts in a journal, knit a scarf, take up painting or cooking, or clip together a fun collage from old magazines. Or get back to an old hobby you once loved!
Healing from trauma requires deep kindness towards ourselves.
Practicing self-compassion involves acknowledging your pain without judgment, understanding that suffering is part of the human experience, and being mindful of negative self-talk.
It helps to remember that healing isn’t linear.
Physical activities like walking or dancing are great ways to release tension. Regular exercise improves our physical health and promotes emotional well-being. It does so by releasing endorphins — our body's natural mood boosters.
Plus, it can be a great way to reconnect with your body and regain a sense of control that trauma might have taken away.
Here are some excellent ways to get moving:
The goal here isn't necessarily about losing weight or building muscle; it's about taking care of yourself holistically during this healing journey.
Remember to start slowly, gradually increasing intensity as your fitness level improves over time — there's no rush!
Healing requires patience, courage, and self-compassion. The eight strategies discussed in this article can serve as a guide.
Remember that everyone's healing journey is unique; what works for one person may not work for another. It's okay to try different strategies until you find what works best for you. In the meantime, consider the following:
You're not alone on this journey; reach out when you need help, and remember — it's okay not to be okay.
Imagine walking through a beautiful forest: the sun is shining, birds are singing, and it seems that all is well. Suddenly, a bear appears directly in front of you. Your heart races, adrenaline surges through your veins, and your body prepares for fight or flight. This is trauma: an intense response to a deeply distressing event that overwhelms our ability to cope.
Now imagine if that bear followed you home and lurked in every corner of your life. That's how living with unresolved trauma can feel. It can manifest in various ways and affect each of us uniquely — from anxiety and depression to substance abuse to physical illness.
Spotting and understanding our own "invisible bear" is the first step towards healing.
In this article, we'll explore eight potent strategies for taming the beast of trauma and reclaiming control over our lives.
Trauma refers to a deeply distressing or disturbing experience that has profound impacts on our mental, physical, and emotional well-being. This can include events such as abuse, neglect, loss of a loved one, accidents, or exposure to violence or disaster.
When we encounter an event or situation that we perceive as physically or emotionally threatening, and it overwhelms our ability to cope, it can result in trauma. This can lead to long-term consequences: post-traumatic stress disorder (PTSD), anxiety, depression, and challenges with self-regulation — and changes in our brains.
It's essential to remember that trauma is highly subjective — what may be traumatic for one of us may not be for another. Our perception of the event, our personal resilience, and our available support systems can significantly influence the impact of the traumatic event.
The connection between the brain and body is a profound one. Picture it as a bustling two-way highway with constant traffic — our thoughts, feelings, and physiological responses— flowing in both directions.
Our brain, the command center, sends out signals based on our thoughts and emotions. These signals manifest physically as changes in heart rate, blood pressure, and muscle tension. Simultaneously, our body sends feedback to the brain, affecting our emotions and thoughts. This dynamic interaction forms the basis of our responses to stress and trauma.
When we experience trauma or chronic stress, the highway traffic can go into overdrive, with signals often stuck in a "fight or flight" loop. Like a car alarm that won't turn off, our body remains in a state of high alert — leading to chronic stress and health issues.
When this alarm system is repeatedly activated due to ongoing trauma or severe experiences, it can lead to long-term changes in our brain’s structure and function. For instance, research has shown that prolonged exposure to stress hormones can shrink the hippocampus (an area responsible for memory and learning), leading to difficulty in processing memory.
Mindfulness and controlled breathing exercises can guide us like a GPS. They help to slow down the traffic, giving us a chance to exit the stressful "fight or flight" loop and enter a calmer state — known as "rest and digest.”
Meditation can significantly reduce stress and improve mental health. Deep, controlled breathing can lower blood pressure and promote feelings of calm.
Practicing mindfulness helps recalibrate our brain's response to stress, creating harmony between brain and body. Gradually, this can help us cut back on unhealthy coping mechanisms — like excessive drinking — paving the way for lasting change.
Unhealed trauma can also affect our prefrontal cortex, the part of our brain responsible for executive functions like decision-making and impulse control, making it harder for us to manage our emotions.
When dealing with trauma, it's essential to remember we don't have to face it alone. Professional help from therapists or counselors specialized in trauma therapy can be a game-changer on our healing journeys.
Therapists trained in trauma work understand the intricate ways trauma alters our brains and bodies. They use evidence-based therapeutic approaches designed specifically to help individuals process traumatic experiences and foster resilience.
Cognitive Behavioral Therapy (CBT), for instance, helps us identify and change the thought patterns that lead to harmful behaviors or emotions. By reframing negative thoughts, CBT can help reduce symptoms of post-traumatic stress disorder (PTSD) and other trauma-related disorders.
Another powerful tool is Eye Movement Desensitization and Reprocessing (EMDR). This therapy uses guided eye movements to help us process traumatic memories and reduce their long-term effects. This reprocesses traumatic memories, integrating them into our overall life narrative rather than letting them linger as disruptive fragments.
Remember, there's no one-size-fits-all when it comes to therapy; what works for one person might not work for another. Take some time to research the resources available to you that might resonate with you personally.
Triggers are hidden tripwires in our minds. When we encounter one, our brain swiftly recalls past experiences. If it finds a link to a traumatic event, it initiates the stress response, preparing us to "fight or flee."
They are the brain's way of alerting us to potential danger based on past experiences. However, triggers can cause us distress and lead us to unhealthy coping mechanisms. They are unique to each of us.
Understanding our triggers is critical for healing. Recognizing these tripwires and replacing our response to them with healthier alternatives — like deep breathing or taking a brisk walk — can help rewire the brain's reward system, making lasting changes more feasible. But in order to do so, we need to know and track those triggers.

Self-care is not just about bubble baths and spa days; it's about taking intentional actions to care for your physical, mental, and emotional health. It means movement, good food, and enough sleep.
Movement helps promote relaxation. Eating well is also important — just as our body needs nutritious food, so does our brain. Certain nutrients can bolster our brain health, enhance mood, and mitigate stress. A balanced diet rich in omega-3 fatty acids, antioxidants, and vitamins is crucial for optimal brain function.
Sleep is more than recharging. It's the time when our brain processes the day's events, solidifying memories and learning. Improving sleep hygiene gives the brain ample time to process trauma and accelerate healing.
Taking care of our body is taking care of our mind.
Having a strong support system is crucial to healing.
Reach out to trusted friends or family members who can provide emotional support.
Consider joining support groups and connect with others who share similar experiences. It can be incredibly healing — and make you feel less alone.
Expressive therapies — like art therapy or dance/movement therapy — offer creative outlets for expressing and processing emotions related to trauma.
They allow you to communicate feelings that might be too difficult to put into words.
But expressing yourself can take many forms: write down your thoughts in a journal, knit a scarf, take up painting or cooking, or clip together a fun collage from old magazines. Or get back to an old hobby you once loved!
Healing from trauma requires deep kindness towards ourselves.
Practicing self-compassion involves acknowledging your pain without judgment, understanding that suffering is part of the human experience, and being mindful of negative self-talk.
It helps to remember that healing isn’t linear.
Physical activities like walking or dancing are great ways to release tension. Regular exercise improves our physical health and promotes emotional well-being. It does so by releasing endorphins — our body's natural mood boosters.
Plus, it can be a great way to reconnect with your body and regain a sense of control that trauma might have taken away.
Here are some excellent ways to get moving:
The goal here isn't necessarily about losing weight or building muscle; it's about taking care of yourself holistically during this healing journey.
Remember to start slowly, gradually increasing intensity as your fitness level improves over time — there's no rush!
Healing requires patience, courage, and self-compassion. The eight strategies discussed in this article can serve as a guide.
Remember that everyone's healing journey is unique; what works for one person may not work for another. It's okay to try different strategies until you find what works best for you. In the meantime, consider the following:
You're not alone on this journey; reach out when you need help, and remember — it's okay not to be okay.

Here’s our comprehensive guide to making and maintaining friendships as an adult. We cover strategies such as being open and approachable, engaging in social activities, being a good listener, and fostering authenticity.
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually, with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet millions of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
As we navigate the unending list of challenges of adulthood, our social circles often seem to shrink faster than our favorite jeans after a tumble in the dryer. As we juggling careers, family life, and personal pursuits, it can feel like there's barely time to breathe, let alone forge new friendships or nurture existing ones. But fear not! Just as those jeans can be stretched back into shape, so too can your social life. If you’re wondering how to get people to like you, how to meet friends as an adult, and ways to to make friends at any point in life, we’ve got you covered. Here are nine simple steps you can take to improve your relationships now — your ultimate guide to making friends as an adult.

The first step on your journey to find friends is to become a beacon of openness and approachability. Think of yourself as a human welcome sign, inviting others to step into your world. A warm smile, direct eye contact, and genuine interest in others can be as inviting as a freshly baked batch of cookies. Remember, it's not about showing off your latest accomplishments or your shiny new car, but about connecting heart-to-heart.
Next, step out of your comfort zone and dive headfirst into social activities that suit your interests. Whether it's a book club, a Zumba class, a cooking group, or a volunteer organization, these environments are ripe for friendship formation. Joining a hiking group, for example, not only gets you out in the fresh air but also offers countless opportunities to bond with fellow nature-lovers.
When it comes to finding ways to make friends, waiting for others to make the first move can often leave you stranded. So, be the trailblazer! If you meet someone who sparks your interest, seize the opportunity and suggest a coffee date, a leisurely walk, or a casual get-together. Think of it as inviting them to join you on a mini-adventure — and who could resist that?

If you’re wondering how to make friends, keep in mind that listening is a superpower in the realm of friendships. When someone shares their thoughts, feelings, or experiences, show them you're genuinely interested. Resist the urge to interrupt or steer the conversation back to yourself. People who feel heard and validated are more likely to trust us and want to open up to us.
Reliability is the sturdy foundation upon which friendships are built. If you make plans, stick to them unless there’s an emergency and you can’t follow-through. If you promise to do something, honor your commitments. Being consistent and showing up will make it more likely that others will want to spend time with us and get to know us better.
You might be wondering, “Why can’t I make friends and actually keep them?” Remember that keeping the friendship flame alive requires regular contact. This doesn't mean you need to chat every day or meet up every week. But a simple text message, email, or phone call can be like a spark that keeps the friendship fire burning brightly. Showing you care can go a long way!
Another important aspect of how to make friends as an adult? Keep in mind that friendships need time to mature. So, practice the art of patience. Don't rush the process or try to force intimacy. It's like planting a seed and waiting for it to grow, knowing that with time and care, it will blossom into something beautiful.
Authenticity is the secret ingredient that makes friendships truly satisfying. Pretending to be someone else is like wearing a mask — it's uncomfortable and people can see right through it. By being yourself, you attract people who appreciate the real you, leading to more fulfilling friendships.
Finally, in a society where socializing often revolves around alcohol, it's important to remember that meaningful connections can be made without it. If you’re wondering where to make friends as an adult, opt for activities that don't involve alcohol, like coffee dates, outdoor adventures, or hobby clubs. These environments allow for genuine connections based on shared interests, not just shared drinks.
Making and keeping friends as an adult might require a bit more effort and intentionality than in our carefree younger years. But the rewards — a robust social network, a shoulder to lean on, a partner in crime for life's adventures — are worth their weight in gold.
Now that you know how to meet friends as an adult, step out of your comfort zone, seize the initiative, and start cultivating those friendships today. Remember, it's never too late to make a new friend. After all, every friend was once a stranger. So, get out there and start turning those strangers into friends!
As we navigate the unending list of challenges of adulthood, our social circles often seem to shrink faster than our favorite jeans after a tumble in the dryer. As we juggling careers, family life, and personal pursuits, it can feel like there's barely time to breathe, let alone forge new friendships or nurture existing ones. But fear not! Just as those jeans can be stretched back into shape, so too can your social life. If you’re wondering how to get people to like you, how to meet friends as an adult, and ways to to make friends at any point in life, we’ve got you covered. Here are nine simple steps you can take to improve your relationships now — your ultimate guide to making friends as an adult.

The first step on your journey to find friends is to become a beacon of openness and approachability. Think of yourself as a human welcome sign, inviting others to step into your world. A warm smile, direct eye contact, and genuine interest in others can be as inviting as a freshly baked batch of cookies. Remember, it's not about showing off your latest accomplishments or your shiny new car, but about connecting heart-to-heart.
Next, step out of your comfort zone and dive headfirst into social activities that suit your interests. Whether it's a book club, a Zumba class, a cooking group, or a volunteer organization, these environments are ripe for friendship formation. Joining a hiking group, for example, not only gets you out in the fresh air but also offers countless opportunities to bond with fellow nature-lovers.
When it comes to finding ways to make friends, waiting for others to make the first move can often leave you stranded. So, be the trailblazer! If you meet someone who sparks your interest, seize the opportunity and suggest a coffee date, a leisurely walk, or a casual get-together. Think of it as inviting them to join you on a mini-adventure — and who could resist that?

If you’re wondering how to make friends, keep in mind that listening is a superpower in the realm of friendships. When someone shares their thoughts, feelings, or experiences, show them you're genuinely interested. Resist the urge to interrupt or steer the conversation back to yourself. People who feel heard and validated are more likely to trust us and want to open up to us.
Reliability is the sturdy foundation upon which friendships are built. If you make plans, stick to them unless there’s an emergency and you can’t follow-through. If you promise to do something, honor your commitments. Being consistent and showing up will make it more likely that others will want to spend time with us and get to know us better.
You might be wondering, “Why can’t I make friends and actually keep them?” Remember that keeping the friendship flame alive requires regular contact. This doesn't mean you need to chat every day or meet up every week. But a simple text message, email, or phone call can be like a spark that keeps the friendship fire burning brightly. Showing you care can go a long way!
Another important aspect of how to make friends as an adult? Keep in mind that friendships need time to mature. So, practice the art of patience. Don't rush the process or try to force intimacy. It's like planting a seed and waiting for it to grow, knowing that with time and care, it will blossom into something beautiful.
Authenticity is the secret ingredient that makes friendships truly satisfying. Pretending to be someone else is like wearing a mask — it's uncomfortable and people can see right through it. By being yourself, you attract people who appreciate the real you, leading to more fulfilling friendships.
Finally, in a society where socializing often revolves around alcohol, it's important to remember that meaningful connections can be made without it. If you’re wondering where to make friends as an adult, opt for activities that don't involve alcohol, like coffee dates, outdoor adventures, or hobby clubs. These environments allow for genuine connections based on shared interests, not just shared drinks.
Making and keeping friends as an adult might require a bit more effort and intentionality than in our carefree younger years. But the rewards — a robust social network, a shoulder to lean on, a partner in crime for life's adventures — are worth their weight in gold.
Now that you know how to meet friends as an adult, step out of your comfort zone, seize the initiative, and start cultivating those friendships today. Remember, it's never too late to make a new friend. After all, every friend was once a stranger. So, get out there and start turning those strangers into friends!

Whenever we’re stressed, our body releases adrenaline and cortisol, which triggers the production of cholesterol. A constant state of stress can lead to high cholesterol and put us at a greater risk for developing heart disease.
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually, with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet millions of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
When we think of high cholesterol, we probably tend to think of avoiding certain foods: fast food, fried foods, sugar, and processed meat are harmful for a variety of reasons, one of which is that they can significantly raise our cholesterol levels.
But, did you know that stress can actually lead to high cholesterol as well? In fact, recurrent or daily stress can not only affect cholesterol levels in the short term, but it can eventually lead to heart disease. Let’s take a closer look.
When we experience stress, our body automatically starts preparing our muscles, heart, and other organs and functions for a fight-or-flight response. Our hypothalamus, a gland located near our brain stem, triggers the release of two hormones — adrenaline and cortisol — that speed up our heart, stimulate the release of energy, and increase blood flow to the brain.
From an evolutionary perspective, this was our body’s way of protecting itself against danger. For example, it’s what allowed us to escape the threat of wild animals. Today, however, this same chemical reaction occurs even if we’re not in immediate physical harm. For instance, our body might go into fight-or-flight mode if we’re facing the potential loss of income.
Both adrenaline and cortisol trigger the production of cholesterol, which is a waxy, fatty substance located in our body’s cells. Our body uses cholesterol to perform many bodily functions, such as making vitamin D and hormones. However, too much cholesterol can be dangerous because it can clog the arteries, eventually leading to a heart attack or stroke.
The amount of adrenaline and cortisol in our body usually remains high until we resolve the stress. Today, however, many of us are living in a constant state of stress. This can lead to high cholesterol levels both in the short-term and long-term, putting us at greater risk for health complications, especially heart disease.
Stress also triggers inflammation that lowers our high-density lipoproteins (HDL), or “good” cholesterol. HDL is vital for helping clear out extra low-density lipoproteins (LDL), the artery-clogging “bad” cholesterol.

More and more research points to the detrimental effects of stress on cholesterol levels. A 2017 study found that psychological stress led to higher levels of triglycerides and LDL (which we want to be low). It also decreased levels of HDL (which we want to be high).
Similarly, another study found a positive correlation between those who experienced job stress and unhealthy cholesterol levels. People with high work stress were also more likely to take cholesterol medicine.
Part of the link between stress and cholesterol is in the way we handle our stress. For instance, many of us might cope with stress by eating unhealthy foods, or turning to sugary or high-carbohydrate “comfort” foods, which appear to reduce feelings of stress. But overconsumption of these foods can cause weight gain and obesity, which raise our risk of high cholesterol.
Similarly, some of us might turn to unhealthy coping mechanisms — such as drinking too much alcohol or smoking — as a way of managing stress. These habits can also raise our cholesterol levels. Furthermore, if we’re not getting enough physical activity, our cholesterol levels will likely rise.
If we already have high cholesterol, stress can make it worse. One study found that people with higher levels of stress had elevated cholesterol compared with those who had lower stress over a three year period.
But even if we’re healthy, our cholesterol levels can rise during stressful times. A study of college students showed higher levels of cortisol, adrenaline, and cholesterol — including total and LDL cholesterol — around the time of their exams.
Interestingly, researchers have found that some of our cardiovascular systems react more than others in response to stress. For example, some people’s blood pressure rises more than others at stressful times.
Our personality type (classified by the letters A, B, C, D, and E) can help predict our response to stress. For instance, research indicates types A and D tend to be high-stress personalities and are especially sensitive to stress hormones. Their heart rates increase, arteries restrict, and sugars are released into the bloodstream at higher rates than those with more relaxed personality types.
Accordingly, research suggests that those with “high stress” personality types can reduce their risk for high cholesterol by spending time engaged in frivolous thought, such as daydreaming. They can also reduce stress by limiting workplace conflicts, organizing their home and workspace, and realistically planning each day with enough time allocated for tasks.
Given the detrimental effects of stress on cholesterol levels in both the short- and long-term, it’s important to do everything we can to manage our stress levels. Here are some tips:
Finally, if you find yourself turning to alcohol as a way to manage stress, consider joining Reframe. We can help you cut back on your drinking and develop healthier lifestyle habits that boost your physical, mental, and emotional well-being.
When we think of high cholesterol, we probably tend to think of avoiding certain foods: fast food, fried foods, sugar, and processed meat are harmful for a variety of reasons, one of which is that they can significantly raise our cholesterol levels.
But, did you know that stress can actually lead to high cholesterol as well? In fact, recurrent or daily stress can not only affect cholesterol levels in the short term, but it can eventually lead to heart disease. Let’s take a closer look.
When we experience stress, our body automatically starts preparing our muscles, heart, and other organs and functions for a fight-or-flight response. Our hypothalamus, a gland located near our brain stem, triggers the release of two hormones — adrenaline and cortisol — that speed up our heart, stimulate the release of energy, and increase blood flow to the brain.
From an evolutionary perspective, this was our body’s way of protecting itself against danger. For example, it’s what allowed us to escape the threat of wild animals. Today, however, this same chemical reaction occurs even if we’re not in immediate physical harm. For instance, our body might go into fight-or-flight mode if we’re facing the potential loss of income.
Both adrenaline and cortisol trigger the production of cholesterol, which is a waxy, fatty substance located in our body’s cells. Our body uses cholesterol to perform many bodily functions, such as making vitamin D and hormones. However, too much cholesterol can be dangerous because it can clog the arteries, eventually leading to a heart attack or stroke.
The amount of adrenaline and cortisol in our body usually remains high until we resolve the stress. Today, however, many of us are living in a constant state of stress. This can lead to high cholesterol levels both in the short-term and long-term, putting us at greater risk for health complications, especially heart disease.
Stress also triggers inflammation that lowers our high-density lipoproteins (HDL), or “good” cholesterol. HDL is vital for helping clear out extra low-density lipoproteins (LDL), the artery-clogging “bad” cholesterol.

More and more research points to the detrimental effects of stress on cholesterol levels. A 2017 study found that psychological stress led to higher levels of triglycerides and LDL (which we want to be low). It also decreased levels of HDL (which we want to be high).
Similarly, another study found a positive correlation between those who experienced job stress and unhealthy cholesterol levels. People with high work stress were also more likely to take cholesterol medicine.
Part of the link between stress and cholesterol is in the way we handle our stress. For instance, many of us might cope with stress by eating unhealthy foods, or turning to sugary or high-carbohydrate “comfort” foods, which appear to reduce feelings of stress. But overconsumption of these foods can cause weight gain and obesity, which raise our risk of high cholesterol.
Similarly, some of us might turn to unhealthy coping mechanisms — such as drinking too much alcohol or smoking — as a way of managing stress. These habits can also raise our cholesterol levels. Furthermore, if we’re not getting enough physical activity, our cholesterol levels will likely rise.
If we already have high cholesterol, stress can make it worse. One study found that people with higher levels of stress had elevated cholesterol compared with those who had lower stress over a three year period.
But even if we’re healthy, our cholesterol levels can rise during stressful times. A study of college students showed higher levels of cortisol, adrenaline, and cholesterol — including total and LDL cholesterol — around the time of their exams.
Interestingly, researchers have found that some of our cardiovascular systems react more than others in response to stress. For example, some people’s blood pressure rises more than others at stressful times.
Our personality type (classified by the letters A, B, C, D, and E) can help predict our response to stress. For instance, research indicates types A and D tend to be high-stress personalities and are especially sensitive to stress hormones. Their heart rates increase, arteries restrict, and sugars are released into the bloodstream at higher rates than those with more relaxed personality types.
Accordingly, research suggests that those with “high stress” personality types can reduce their risk for high cholesterol by spending time engaged in frivolous thought, such as daydreaming. They can also reduce stress by limiting workplace conflicts, organizing their home and workspace, and realistically planning each day with enough time allocated for tasks.
Given the detrimental effects of stress on cholesterol levels in both the short- and long-term, it’s important to do everything we can to manage our stress levels. Here are some tips:
Finally, if you find yourself turning to alcohol as a way to manage stress, consider joining Reframe. We can help you cut back on your drinking and develop healthier lifestyle habits that boost your physical, mental, and emotional well-being.