

Understand how emotions influence recovery and learn practical strategies to manage them effectively for a healthier, more fulfilling journey.
Recovery is more than just changing your drinking habits; it's about transforming your relationship with yourself. It's about understanding the emotions that drive your choices and developing healthier ways to cope. This post explores the concept of emotional goals in recovery, offering a roadmap for lasting change. We'll discuss how to identify your ideal emotional state, create achievable milestones, and build emotional strength through self-awareness and mindfulness. We'll also delve into the importance of self-compassion, positive self-talk, and building a strong support system. Plus, we'll explore how technology, including apps like Reframe, can provide valuable support and resources on your journey to emotional well-being.
Recovery journeys are deeply personal, but they often share a common thread: the importance of emotional well-being. While managing drinking is a significant aspect, true recovery delves into the underlying emotions and thought patterns that influence our relationship with alcohol. This is where emotional goals come into play. They're not about eliminating negative emotions altogether—that's unrealistic. Instead, they're about learning to understand, process, and manage those emotions effectively without turning to alcohol as a coping mechanism. Think of it as developing a new toolkit for navigating life's ups and downs.
Emotional goals involve recognizing your emotional triggers—those situations or feelings that make you want to drink. Perhaps it's stress from work, loneliness, or even celebrations where alcohol is prevalent. By identifying these triggers, you can start to anticipate challenges and develop healthier responses. Why do you react the way you do? What thoughts and feelings arise? This self-awareness is fundamental to changing your behavior. Greater Boston Addiction Centers highlights the importance of understanding these emotional responses.
Building emotional resilience is another key component of emotional goals. It's about developing the ability to bounce back from difficult experiences without resorting to old habits. This involves learning coping strategies, such as mindfulness techniques, deep breathing exercises, or engaging in activities you enjoy. Perennial Recovery discusses building this resilience as part of redefining your relationship with alcohol. Tracking your emotions throughout the day can provide valuable insights into your emotional landscape, helping you pinpoint areas where you need to focus your efforts, as suggested by Lumina Recovery. Finally, effective communication plays a crucial role in achieving emotional goals. Expressing your needs and feelings clearly and honestly is essential for building a strong support network, a point emphasized by Samba Recovery.
Traditional recovery often emphasizes abstinence as the primary goal. While this is important, solely focusing on not drinking can sometimes overshadow the underlying emotional issues that contribute to alcohol use. Feeling-based recovery, on the other hand, recognizes that lasting change comes from understanding and addressing these deeper emotional needs. It shifts the focus from simply controlling behavior to cultivating genuine well-being. This approach empowers you to build a healthier relationship with alcohol by addressing the root causes of your drinking habits, rather than just the symptoms.
Think of it this way: if you're constantly restricting yourself without understanding why you drink, you might end up feeling deprived and resentful. This can create a cycle of restriction and relapse. As Annie Grace discusses in her work on rethinking drinking, traditional recovery programs often prioritize abstinence above all else, sometimes neglecting the emotional well-being of individuals in recovery. Feeling-based recovery acknowledges that our worth isn't tied to our behavior. By focusing on how we want to feel—calm, content, joyful—we set ourselves up for sustainable change. When our goals are rooted in positive emotions, we're more likely to stick with them and avoid the shame and guilt that can derail our progress. This approach allows you to explore the emotions that drive your drinking habits and develop healthier coping mechanisms.
Prioritizing emotional well-being has numerous benefits. It equips you with the tools to manage stress, anxiety, and other challenging emotions without turning to alcohol. As the team at Perennial Recovery points out, implementing self-care practices and stress management techniques can significantly reduce your reliance on alcohol as a coping mechanism. Building emotional resilience, as highlighted by the Greater Boston Addiction Centers, is crucial for navigating the ups and downs of life without resorting to substance use. When you develop a strong emotional foundation, you're better prepared to handle triggers and cravings. Furthermore, research demonstrates that finding purpose in life can improve emotional recovery from negative events. This sense of purpose can motivate you to reframe stressful situations and deal with them more productively, further supporting your recovery journey. By focusing on your emotional health, you create a positive feedback loop: as you feel better, you're more motivated to make healthy choices, which in turn strengthens your emotional well-being. This holistic approach sets the stage for long-term success and a more fulfilling life.
Setting emotional goals provides a roadmap for your recovery journey. It's about understanding how you want to feel and taking steps to get there. This section offers practical guidance on setting meaningful emotional goals that support lasting change.
Think about how you ideally want to feel. Do you crave more peace and less anxiety? More confidence and less self-doubt? Perhaps you want to experience more joy and connection in your life. Exploring these desired emotional states is the first step. Often, people use alcohol to cope with stress, anxiety, or other challenging emotions, so identifying your ideal state helps you visualize a different path. Instead of reaching for a drink, what positive feelings could you cultivate instead? This process helps redefine your relationship with alcohol and create a vision for a healthier, more fulfilling life. Consider writing down these ideal emotional states to create a clear picture of what you're working toward. This can be a powerful motivator throughout your recovery.
Once you've identified your ideal emotional state, break it down into smaller, achievable milestones. Setting small, realistic goals makes success feel more attainable and keeps you motivated. For example, if your goal is to feel less anxious, start with small steps like practicing deep breathing exercises for five minutes each day or incorporating mindfulness into your routine. If you want to feel more connected, set a goal to have one meaningful conversation with a loved one each week. As you achieve these smaller milestones, you'll build confidence and momentum toward your larger emotional goals. Remember, your emotional goals should align with your overall recovery journey. For example, focusing on social interactions can help you build a supportive network, which is crucial for long-term recovery. Start small, celebrate your wins, and gradually work your way toward the emotional state you envision for yourself.
Building emotional strength and self-awareness is key to changing your drinking habits. It's about understanding your emotions, how they influence your choices, and developing healthier ways to cope with them. This understanding helps you identify your triggers, manage cravings, and make choices that align with your goals.
Mindfulness is a powerful tool for developing self-awareness, especially regarding your emotions. It involves paying attention to your present-moment experiences—your thoughts, feelings, and bodily sensations—without judgment. Think of it as tuning into your inner world. Regular mindfulness practice, like meditation, helps you become more aware of your emotional responses. You start to notice patterns: how your emotions change throughout the day, what triggers them, and how they influence your behavior. This awareness is crucial for making conscious choices about your drinking. For example, if you notice that stress often leads to a desire to drink, you can start exploring alternative coping mechanisms, like deep breathing or going for a walk.
Changing habits is rarely a smooth, linear process. There will be times when you face challenges or experience setbacks. During these times, self-compassion is essential. It's about treating yourself with the same kindness and understanding you would offer a friend. Self-compassion helps you avoid negative self-talk and over-identification with difficult emotions. Instead of criticizing yourself for slip-ups, you can acknowledge them as part of the learning process and focus on getting back on track. Positive self-talk also plays a vital role. The words you use when talking to yourself have a powerful impact on your mindset and motivation. Replacing negative self-talk with positive affirmations can boost your confidence and resilience, making you better equipped to handle challenges and stay committed to your goals. Sharing your feelings and needs with trusted individuals can provide valuable support and strengthen your commitment to change. Remember, recovery is a journey, not a destination. Be patient with yourself, celebrate your progress, and focus on building a healthier, happier relationship with yourself and alcohol.
Tracking your emotional progress is key to understanding yourself and your recovery journey. It's like keeping a fitness log—you need to see where you started to appreciate how far you've come. This section offers practical ways to monitor your emotional state and celebrate your wins.
Journaling is a powerful tool for self-discovery. It's a safe space to explore your emotions without judgment. Start by noting your feelings throughout the day, including their intensity and any triggers that might have caused them. For example, did a stressful meeting make you feel anxious? Did a social gathering tempt you to drink? Over time, these entries will reveal patterns and provide valuable insights into your emotional fluctuations. Recognizing these patterns, as Luminarecovery explains in their guide to identifying emotions, is crucial for understanding the underlying causes and developing effective coping strategies. Don't worry about perfect grammar or elegant prose; just focus on honest expression.
In addition to journaling, technology can be a valuable ally in your recovery. Mood tracking apps and wearables offer convenient ways to monitor your emotional state and access relaxation techniques. Many apps provide guided meditations, breathing exercises, and other tools to help you manage stress and stay grounded. These tools, as Forbes notes in their article on technology for addiction recovery, can be crucial components of a successful recovery plan. They can also help you identify potential triggers and develop coping mechanisms. The National Institutes of Health published research on user experience with mental health apps, emphasizing the importance of engagement and user-friendliness. Experiment with different apps to find one that resonates with you and integrates seamlessly into your routine. Reframe itself offers personalized drink tracking and evidence-based programs to support your journey.
Recovering from alcohol dependence isn't a solo journey. Building a strong support system is crucial for navigating the emotional ups and downs of changing your drinking habits. Connecting with others who understand your struggles and seeking professional guidance can make all the difference.
Start by talking to friends and family members who are empathetic and willing to support your goals. Openly communicate your needs and explain how they can help you stay on track. Sometimes, loved ones unintentionally enable unhealthy habits, so clearly explaining your boundaries is important. For example, let them know if you'd prefer they not drink around you or offer you alcohol. Having these conversations can strengthen your relationships and create a more supportive environment. Remember, setting boundaries is a form of self-care, and it’s okay to prioritize your well-being. Reframe's mindful drinking program offers resources and support for setting healthy boundaries. Consider exploring resources like Mountain Valley Recovery for additional guidance on building a strong support network.
Professional guidance can provide you with personalized strategies and coping mechanisms. Therapists specializing in addiction can help you understand the root causes of your drinking habits and develop healthier ways to manage emotions. They can also offer evidence-based techniques like cognitive behavioral therapy (CBT) to address negative thought patterns and behaviors. In addition to individual therapy, consider joining a support group. Connecting with others facing similar challenges creates a sense of community and shared understanding. Support groups like Alcoholics Anonymous or SMART Recovery offer safe spaces to share experiences, learn from others, and build a network of support. Combining professional guidance with community support can significantly enhance your recovery journey. Check out Reframe's FAQ for more information on finding support resources. You can also find helpful communication tips for recovery at Samba Recovery.
This section dives into practical strategies for reshaping how you think about and interact with alcohol. It's a crucial part of lasting recovery.
Redefining your relationship with alcohol starts with getting clear on your goals. What do you want to achieve? Everyone's journey is unique—there's no one-size-fits-all answer. Do you want to cut back on how much you drink, or stop altogether? Think about what a healthier relationship with alcohol looks like for you, and what you hope to gain on this journey. As Red Willow Counseling points out, "Not every relationship with alcohol will look the same, so individuals will need to determine what they want to get out of this experience." This personal reflection is the foundation for making positive changes. Reframe’s Mindful Drinking resources can provide valuable support and guidance as you explore these new approaches.
It's also important to recognize the role alcohol plays in your life. Do you use it to celebrate, to unwind, or to cope with stress? Many people turn to alcohol as a quick fix for difficult emotions, as highlighted by Perennial Recovery in their discussion of redefining your relationship with alcohol. By understanding your drinking patterns, you can start to identify healthier ways to manage stress and celebrate life's moments.
If you often use alcohol to deal with stress, anxiety, or other tough emotions, it's time to explore alternative coping mechanisms. Elev8 Centers emphasizes the importance of this step in their guide on how to redefine your relationship with alcohol. Think about activities you enjoy or find relaxing—spending time in nature, listening to music, practicing yoga, or connecting with loved ones. These activities can become your new go-to strategies for managing challenging situations. Reframe offers a variety of tools and resources, including a Sober Days Counting and Cost Savings Calculator, to support you in building these new habits and tracking your progress.
Building a toolkit of healthy coping mechanisms is essential for long-term success. As you discover new ways to manage stress and regulate your emotions, you'll gradually reduce your reliance on alcohol. This process, as described by Elev8 Centers, allows you to "gradually reduce reliance on alcohol as a means of escape or relaxation." Remember, building new habits takes time and effort, so be patient with yourself and celebrate each step forward.
Recovery isn't always a straight line; there will be bumps in the road, and that's perfectly normal. This section offers practical strategies to manage setbacks, stay motivated, and integrate emotional and behavioral approaches for long-term success.
Setbacks are a natural part of any change process. Don't view them as failures, but rather as opportunities for learning and growth. When you experience a setback, acknowledge your feelings without judgment. Try to understand what triggered the setback and what you can do differently next time. A strong sense of purpose can fuel your motivation during challenging times. Reconnect with your reasons for wanting to change your drinking habits. Perhaps you want to improve your physical health, strengthen your relationships, or simply feel more present in your life. Remembering your "why" can help you regain your footing and move forward. Research even suggests that having a purpose can help you reframe stressful situations and recover more effectively. This sense of purpose can be a powerful motivator when things get tough. Check out Reframe's Mindful Drinking resources for additional support.
True recovery involves addressing both emotions and behaviors. Learning to regulate your emotions is key. This might involve developing coping mechanisms for difficult emotions like stress, anxiety, or sadness. Instead of turning to alcohol, explore healthier alternatives such as exercise, mindfulness practices, or spending time in nature. As you explore these new coping mechanisms, you'll begin to redefine your relationship with alcohol. Open communication is also essential. Talking to trusted friends, family members, or a therapist can provide valuable support and help you process your emotions. Connecting with others who understand what you're going through can make a significant difference. Consider joining Reframe's supportive community by downloading the app to connect with others on a similar journey. Leveraging technology can also be beneficial. Apps like Reframe can provide personalized support, track your progress, and offer tools for managing emotions and behaviors. The combination of emotional and behavioral strategies, along with a strong support system, can empower you to achieve lasting change.
Recovery isn't one-size-fits-all. It's a deeply personal experience, and what works for one person might not work for another. That's why personalizing your approach is key to lasting change. This involves understanding your unique emotional landscape, identifying your specific triggers, and tailoring your strategies to meet your individual needs. A personalized recovery journey acknowledges that your experiences, challenges, and strengths are unique, empowering you to take control of your path.
Think of building a toolbox for your recovery. Traditional methods, like support groups and therapy, offer valuable structure and human connection. These approaches provide a safe space to share experiences and learn from others who understand the challenges of recovery. Combining these with innovative tools, like mindfulness apps and online resources, can amplify your efforts. For example, Reframe’s mindful drinking program offers evidence-based exercises and personalized support to help you understand and manage your drinking habits. Exploring alternative coping mechanisms, such as exercise, creative expression, or spending time in nature, can further enhance your journey.
Pay attention to your emotions. They hold valuable clues about your needs and triggers. If stress drives you to drink, incorporating stress management techniques into your recovery plan is crucial. This might involve practicing mindfulness, deep breathing exercises, or engaging in activities you enjoy. If you struggle with loneliness, building a strong support system can make a world of difference. Honest communication with loved ones, joining a support group, or connecting with a therapist can provide the understanding and encouragement you need. Remember, addressing your emotional needs is not a sign of weakness; it's a powerful step towards building resilience and creating a fulfilling life free from the grip of alcohol dependence. Tools like Reframe’s Sober Days Calculator and Alcohol Spend Calculator can also help you track your progress and stay motivated.
Technology can play a supportive role in your emotional recovery journey. Think of apps as tools that complement, not replace, traditional methods like therapy and support groups. They can be particularly helpful for tracking progress, practicing mindfulness, and accessing resources on the go. When choosing an app, look for features aligned with your needs and preferences. Consider exploring Reframe's Mindful Drinking program as part of your toolkit.
Apps designed with user feedback in mind tend to be more effective. For example, if an app incorporates input from people in recovery, it's more likely to address real-world challenges and offer practical solutions. This user-centered design approach often leads to higher engagement and better outcomes, as highlighted in research on app uptake and engagement. Look for apps that prioritize user experience and actively solicit feedback. Reframe, for instance, values user input and continually refines its features based on community suggestions. You can learn more about Reframe and its features on their FAQ page.
Effective recovery apps often incorporate evidence-based features that promote emotional well-being. These might include tools for tracking moods, practicing mindfulness exercises, or learning coping skills. Some apps also offer personalized programs based on your specific needs and goals. The Reframe app, for example, provides structured programs and resources grounded in neuroscience to help you understand and manage your drinking habits. Prioritize apps that offer features backed by research and tailored to your individual recovery path. For more insights on how apps can support recovery, check out resources on the relationship between user experience and engagement with mental health apps.
What are emotional goals in recovery, and why are they important? Emotional goals in recovery are about learning to understand and manage your emotions without using alcohol as a crutch. They involve identifying your emotional triggers, building resilience, and developing healthier coping mechanisms. These goals are crucial because they address the root causes of unhealthy drinking habits, leading to more sustainable change. It's about creating a life where you feel equipped to handle challenges without relying on alcohol.
How is feeling-based recovery different from traditional approaches? Traditional recovery often emphasizes abstinence, while feeling-based recovery focuses on understanding and addressing the underlying emotional needs that contribute to alcohol use. It's not just about not drinking; it's about cultivating overall well-being and building a healthier relationship with yourself and your emotions. This approach empowers you to make lasting changes by addressing the root causes of your drinking habits, rather than just the symptoms.
How can I set meaningful emotional goals for myself? Start by envisioning your ideal emotional state. How do you want to feel? Then, break down that vision into smaller, achievable milestones. If you want to feel less anxious, start with short mindfulness exercises. If you want to feel more connected, prioritize meaningful conversations with loved ones. These small steps build momentum and confidence.
What are some practical ways to build emotional strength and self-awareness? Mindfulness practices, like meditation, can help you become more aware of your emotional responses and identify your triggers. Self-compassion and positive self-talk are also essential. Treat yourself with kindness, especially during setbacks, and focus on building a healthier relationship with yourself. Remember, change takes time, and setbacks are a normal part of the process.
How can I build a support system for my emotional recovery? Openly communicate your needs with trusted friends and family members. Seek professional guidance from a therapist specializing in addiction. Consider joining a support group to connect with others who understand your challenges. Building a strong support network can provide encouragement, accountability, and a sense of community during your recovery journey.
Recovery is more than just changing your drinking habits; it's about transforming your relationship with yourself. It's about understanding the emotions that drive your choices and developing healthier ways to cope. This post explores the concept of emotional goals in recovery, offering a roadmap for lasting change. We'll discuss how to identify your ideal emotional state, create achievable milestones, and build emotional strength through self-awareness and mindfulness. We'll also delve into the importance of self-compassion, positive self-talk, and building a strong support system. Plus, we'll explore how technology, including apps like Reframe, can provide valuable support and resources on your journey to emotional well-being.
Recovery journeys are deeply personal, but they often share a common thread: the importance of emotional well-being. While managing drinking is a significant aspect, true recovery delves into the underlying emotions and thought patterns that influence our relationship with alcohol. This is where emotional goals come into play. They're not about eliminating negative emotions altogether—that's unrealistic. Instead, they're about learning to understand, process, and manage those emotions effectively without turning to alcohol as a coping mechanism. Think of it as developing a new toolkit for navigating life's ups and downs.
Emotional goals involve recognizing your emotional triggers—those situations or feelings that make you want to drink. Perhaps it's stress from work, loneliness, or even celebrations where alcohol is prevalent. By identifying these triggers, you can start to anticipate challenges and develop healthier responses. Why do you react the way you do? What thoughts and feelings arise? This self-awareness is fundamental to changing your behavior. Greater Boston Addiction Centers highlights the importance of understanding these emotional responses.
Building emotional resilience is another key component of emotional goals. It's about developing the ability to bounce back from difficult experiences without resorting to old habits. This involves learning coping strategies, such as mindfulness techniques, deep breathing exercises, or engaging in activities you enjoy. Perennial Recovery discusses building this resilience as part of redefining your relationship with alcohol. Tracking your emotions throughout the day can provide valuable insights into your emotional landscape, helping you pinpoint areas where you need to focus your efforts, as suggested by Lumina Recovery. Finally, effective communication plays a crucial role in achieving emotional goals. Expressing your needs and feelings clearly and honestly is essential for building a strong support network, a point emphasized by Samba Recovery.
Traditional recovery often emphasizes abstinence as the primary goal. While this is important, solely focusing on not drinking can sometimes overshadow the underlying emotional issues that contribute to alcohol use. Feeling-based recovery, on the other hand, recognizes that lasting change comes from understanding and addressing these deeper emotional needs. It shifts the focus from simply controlling behavior to cultivating genuine well-being. This approach empowers you to build a healthier relationship with alcohol by addressing the root causes of your drinking habits, rather than just the symptoms.
Think of it this way: if you're constantly restricting yourself without understanding why you drink, you might end up feeling deprived and resentful. This can create a cycle of restriction and relapse. As Annie Grace discusses in her work on rethinking drinking, traditional recovery programs often prioritize abstinence above all else, sometimes neglecting the emotional well-being of individuals in recovery. Feeling-based recovery acknowledges that our worth isn't tied to our behavior. By focusing on how we want to feel—calm, content, joyful—we set ourselves up for sustainable change. When our goals are rooted in positive emotions, we're more likely to stick with them and avoid the shame and guilt that can derail our progress. This approach allows you to explore the emotions that drive your drinking habits and develop healthier coping mechanisms.
Prioritizing emotional well-being has numerous benefits. It equips you with the tools to manage stress, anxiety, and other challenging emotions without turning to alcohol. As the team at Perennial Recovery points out, implementing self-care practices and stress management techniques can significantly reduce your reliance on alcohol as a coping mechanism. Building emotional resilience, as highlighted by the Greater Boston Addiction Centers, is crucial for navigating the ups and downs of life without resorting to substance use. When you develop a strong emotional foundation, you're better prepared to handle triggers and cravings. Furthermore, research demonstrates that finding purpose in life can improve emotional recovery from negative events. This sense of purpose can motivate you to reframe stressful situations and deal with them more productively, further supporting your recovery journey. By focusing on your emotional health, you create a positive feedback loop: as you feel better, you're more motivated to make healthy choices, which in turn strengthens your emotional well-being. This holistic approach sets the stage for long-term success and a more fulfilling life.
Setting emotional goals provides a roadmap for your recovery journey. It's about understanding how you want to feel and taking steps to get there. This section offers practical guidance on setting meaningful emotional goals that support lasting change.
Think about how you ideally want to feel. Do you crave more peace and less anxiety? More confidence and less self-doubt? Perhaps you want to experience more joy and connection in your life. Exploring these desired emotional states is the first step. Often, people use alcohol to cope with stress, anxiety, or other challenging emotions, so identifying your ideal state helps you visualize a different path. Instead of reaching for a drink, what positive feelings could you cultivate instead? This process helps redefine your relationship with alcohol and create a vision for a healthier, more fulfilling life. Consider writing down these ideal emotional states to create a clear picture of what you're working toward. This can be a powerful motivator throughout your recovery.
Once you've identified your ideal emotional state, break it down into smaller, achievable milestones. Setting small, realistic goals makes success feel more attainable and keeps you motivated. For example, if your goal is to feel less anxious, start with small steps like practicing deep breathing exercises for five minutes each day or incorporating mindfulness into your routine. If you want to feel more connected, set a goal to have one meaningful conversation with a loved one each week. As you achieve these smaller milestones, you'll build confidence and momentum toward your larger emotional goals. Remember, your emotional goals should align with your overall recovery journey. For example, focusing on social interactions can help you build a supportive network, which is crucial for long-term recovery. Start small, celebrate your wins, and gradually work your way toward the emotional state you envision for yourself.
Building emotional strength and self-awareness is key to changing your drinking habits. It's about understanding your emotions, how they influence your choices, and developing healthier ways to cope with them. This understanding helps you identify your triggers, manage cravings, and make choices that align with your goals.
Mindfulness is a powerful tool for developing self-awareness, especially regarding your emotions. It involves paying attention to your present-moment experiences—your thoughts, feelings, and bodily sensations—without judgment. Think of it as tuning into your inner world. Regular mindfulness practice, like meditation, helps you become more aware of your emotional responses. You start to notice patterns: how your emotions change throughout the day, what triggers them, and how they influence your behavior. This awareness is crucial for making conscious choices about your drinking. For example, if you notice that stress often leads to a desire to drink, you can start exploring alternative coping mechanisms, like deep breathing or going for a walk.
Changing habits is rarely a smooth, linear process. There will be times when you face challenges or experience setbacks. During these times, self-compassion is essential. It's about treating yourself with the same kindness and understanding you would offer a friend. Self-compassion helps you avoid negative self-talk and over-identification with difficult emotions. Instead of criticizing yourself for slip-ups, you can acknowledge them as part of the learning process and focus on getting back on track. Positive self-talk also plays a vital role. The words you use when talking to yourself have a powerful impact on your mindset and motivation. Replacing negative self-talk with positive affirmations can boost your confidence and resilience, making you better equipped to handle challenges and stay committed to your goals. Sharing your feelings and needs with trusted individuals can provide valuable support and strengthen your commitment to change. Remember, recovery is a journey, not a destination. Be patient with yourself, celebrate your progress, and focus on building a healthier, happier relationship with yourself and alcohol.
Tracking your emotional progress is key to understanding yourself and your recovery journey. It's like keeping a fitness log—you need to see where you started to appreciate how far you've come. This section offers practical ways to monitor your emotional state and celebrate your wins.
Journaling is a powerful tool for self-discovery. It's a safe space to explore your emotions without judgment. Start by noting your feelings throughout the day, including their intensity and any triggers that might have caused them. For example, did a stressful meeting make you feel anxious? Did a social gathering tempt you to drink? Over time, these entries will reveal patterns and provide valuable insights into your emotional fluctuations. Recognizing these patterns, as Luminarecovery explains in their guide to identifying emotions, is crucial for understanding the underlying causes and developing effective coping strategies. Don't worry about perfect grammar or elegant prose; just focus on honest expression.
In addition to journaling, technology can be a valuable ally in your recovery. Mood tracking apps and wearables offer convenient ways to monitor your emotional state and access relaxation techniques. Many apps provide guided meditations, breathing exercises, and other tools to help you manage stress and stay grounded. These tools, as Forbes notes in their article on technology for addiction recovery, can be crucial components of a successful recovery plan. They can also help you identify potential triggers and develop coping mechanisms. The National Institutes of Health published research on user experience with mental health apps, emphasizing the importance of engagement and user-friendliness. Experiment with different apps to find one that resonates with you and integrates seamlessly into your routine. Reframe itself offers personalized drink tracking and evidence-based programs to support your journey.
Recovering from alcohol dependence isn't a solo journey. Building a strong support system is crucial for navigating the emotional ups and downs of changing your drinking habits. Connecting with others who understand your struggles and seeking professional guidance can make all the difference.
Start by talking to friends and family members who are empathetic and willing to support your goals. Openly communicate your needs and explain how they can help you stay on track. Sometimes, loved ones unintentionally enable unhealthy habits, so clearly explaining your boundaries is important. For example, let them know if you'd prefer they not drink around you or offer you alcohol. Having these conversations can strengthen your relationships and create a more supportive environment. Remember, setting boundaries is a form of self-care, and it’s okay to prioritize your well-being. Reframe's mindful drinking program offers resources and support for setting healthy boundaries. Consider exploring resources like Mountain Valley Recovery for additional guidance on building a strong support network.
Professional guidance can provide you with personalized strategies and coping mechanisms. Therapists specializing in addiction can help you understand the root causes of your drinking habits and develop healthier ways to manage emotions. They can also offer evidence-based techniques like cognitive behavioral therapy (CBT) to address negative thought patterns and behaviors. In addition to individual therapy, consider joining a support group. Connecting with others facing similar challenges creates a sense of community and shared understanding. Support groups like Alcoholics Anonymous or SMART Recovery offer safe spaces to share experiences, learn from others, and build a network of support. Combining professional guidance with community support can significantly enhance your recovery journey. Check out Reframe's FAQ for more information on finding support resources. You can also find helpful communication tips for recovery at Samba Recovery.
This section dives into practical strategies for reshaping how you think about and interact with alcohol. It's a crucial part of lasting recovery.
Redefining your relationship with alcohol starts with getting clear on your goals. What do you want to achieve? Everyone's journey is unique—there's no one-size-fits-all answer. Do you want to cut back on how much you drink, or stop altogether? Think about what a healthier relationship with alcohol looks like for you, and what you hope to gain on this journey. As Red Willow Counseling points out, "Not every relationship with alcohol will look the same, so individuals will need to determine what they want to get out of this experience." This personal reflection is the foundation for making positive changes. Reframe’s Mindful Drinking resources can provide valuable support and guidance as you explore these new approaches.
It's also important to recognize the role alcohol plays in your life. Do you use it to celebrate, to unwind, or to cope with stress? Many people turn to alcohol as a quick fix for difficult emotions, as highlighted by Perennial Recovery in their discussion of redefining your relationship with alcohol. By understanding your drinking patterns, you can start to identify healthier ways to manage stress and celebrate life's moments.
If you often use alcohol to deal with stress, anxiety, or other tough emotions, it's time to explore alternative coping mechanisms. Elev8 Centers emphasizes the importance of this step in their guide on how to redefine your relationship with alcohol. Think about activities you enjoy or find relaxing—spending time in nature, listening to music, practicing yoga, or connecting with loved ones. These activities can become your new go-to strategies for managing challenging situations. Reframe offers a variety of tools and resources, including a Sober Days Counting and Cost Savings Calculator, to support you in building these new habits and tracking your progress.
Building a toolkit of healthy coping mechanisms is essential for long-term success. As you discover new ways to manage stress and regulate your emotions, you'll gradually reduce your reliance on alcohol. This process, as described by Elev8 Centers, allows you to "gradually reduce reliance on alcohol as a means of escape or relaxation." Remember, building new habits takes time and effort, so be patient with yourself and celebrate each step forward.
Recovery isn't always a straight line; there will be bumps in the road, and that's perfectly normal. This section offers practical strategies to manage setbacks, stay motivated, and integrate emotional and behavioral approaches for long-term success.
Setbacks are a natural part of any change process. Don't view them as failures, but rather as opportunities for learning and growth. When you experience a setback, acknowledge your feelings without judgment. Try to understand what triggered the setback and what you can do differently next time. A strong sense of purpose can fuel your motivation during challenging times. Reconnect with your reasons for wanting to change your drinking habits. Perhaps you want to improve your physical health, strengthen your relationships, or simply feel more present in your life. Remembering your "why" can help you regain your footing and move forward. Research even suggests that having a purpose can help you reframe stressful situations and recover more effectively. This sense of purpose can be a powerful motivator when things get tough. Check out Reframe's Mindful Drinking resources for additional support.
True recovery involves addressing both emotions and behaviors. Learning to regulate your emotions is key. This might involve developing coping mechanisms for difficult emotions like stress, anxiety, or sadness. Instead of turning to alcohol, explore healthier alternatives such as exercise, mindfulness practices, or spending time in nature. As you explore these new coping mechanisms, you'll begin to redefine your relationship with alcohol. Open communication is also essential. Talking to trusted friends, family members, or a therapist can provide valuable support and help you process your emotions. Connecting with others who understand what you're going through can make a significant difference. Consider joining Reframe's supportive community by downloading the app to connect with others on a similar journey. Leveraging technology can also be beneficial. Apps like Reframe can provide personalized support, track your progress, and offer tools for managing emotions and behaviors. The combination of emotional and behavioral strategies, along with a strong support system, can empower you to achieve lasting change.
Recovery isn't one-size-fits-all. It's a deeply personal experience, and what works for one person might not work for another. That's why personalizing your approach is key to lasting change. This involves understanding your unique emotional landscape, identifying your specific triggers, and tailoring your strategies to meet your individual needs. A personalized recovery journey acknowledges that your experiences, challenges, and strengths are unique, empowering you to take control of your path.
Think of building a toolbox for your recovery. Traditional methods, like support groups and therapy, offer valuable structure and human connection. These approaches provide a safe space to share experiences and learn from others who understand the challenges of recovery. Combining these with innovative tools, like mindfulness apps and online resources, can amplify your efforts. For example, Reframe’s mindful drinking program offers evidence-based exercises and personalized support to help you understand and manage your drinking habits. Exploring alternative coping mechanisms, such as exercise, creative expression, or spending time in nature, can further enhance your journey.
Pay attention to your emotions. They hold valuable clues about your needs and triggers. If stress drives you to drink, incorporating stress management techniques into your recovery plan is crucial. This might involve practicing mindfulness, deep breathing exercises, or engaging in activities you enjoy. If you struggle with loneliness, building a strong support system can make a world of difference. Honest communication with loved ones, joining a support group, or connecting with a therapist can provide the understanding and encouragement you need. Remember, addressing your emotional needs is not a sign of weakness; it's a powerful step towards building resilience and creating a fulfilling life free from the grip of alcohol dependence. Tools like Reframe’s Sober Days Calculator and Alcohol Spend Calculator can also help you track your progress and stay motivated.
Technology can play a supportive role in your emotional recovery journey. Think of apps as tools that complement, not replace, traditional methods like therapy and support groups. They can be particularly helpful for tracking progress, practicing mindfulness, and accessing resources on the go. When choosing an app, look for features aligned with your needs and preferences. Consider exploring Reframe's Mindful Drinking program as part of your toolkit.
Apps designed with user feedback in mind tend to be more effective. For example, if an app incorporates input from people in recovery, it's more likely to address real-world challenges and offer practical solutions. This user-centered design approach often leads to higher engagement and better outcomes, as highlighted in research on app uptake and engagement. Look for apps that prioritize user experience and actively solicit feedback. Reframe, for instance, values user input and continually refines its features based on community suggestions. You can learn more about Reframe and its features on their FAQ page.
Effective recovery apps often incorporate evidence-based features that promote emotional well-being. These might include tools for tracking moods, practicing mindfulness exercises, or learning coping skills. Some apps also offer personalized programs based on your specific needs and goals. The Reframe app, for example, provides structured programs and resources grounded in neuroscience to help you understand and manage your drinking habits. Prioritize apps that offer features backed by research and tailored to your individual recovery path. For more insights on how apps can support recovery, check out resources on the relationship between user experience and engagement with mental health apps.
What are emotional goals in recovery, and why are they important? Emotional goals in recovery are about learning to understand and manage your emotions without using alcohol as a crutch. They involve identifying your emotional triggers, building resilience, and developing healthier coping mechanisms. These goals are crucial because they address the root causes of unhealthy drinking habits, leading to more sustainable change. It's about creating a life where you feel equipped to handle challenges without relying on alcohol.
How is feeling-based recovery different from traditional approaches? Traditional recovery often emphasizes abstinence, while feeling-based recovery focuses on understanding and addressing the underlying emotional needs that contribute to alcohol use. It's not just about not drinking; it's about cultivating overall well-being and building a healthier relationship with yourself and your emotions. This approach empowers you to make lasting changes by addressing the root causes of your drinking habits, rather than just the symptoms.
How can I set meaningful emotional goals for myself? Start by envisioning your ideal emotional state. How do you want to feel? Then, break down that vision into smaller, achievable milestones. If you want to feel less anxious, start with short mindfulness exercises. If you want to feel more connected, prioritize meaningful conversations with loved ones. These small steps build momentum and confidence.
What are some practical ways to build emotional strength and self-awareness? Mindfulness practices, like meditation, can help you become more aware of your emotional responses and identify your triggers. Self-compassion and positive self-talk are also essential. Treat yourself with kindness, especially during setbacks, and focus on building a healthier relationship with yourself. Remember, change takes time, and setbacks are a normal part of the process.
How can I build a support system for my emotional recovery? Openly communicate your needs with trusted friends and family members. Seek professional guidance from a therapist specializing in addiction. Consider joining a support group to connect with others who understand your challenges. Building a strong support network can provide encouragement, accountability, and a sense of community during your recovery journey.

Drinking alcohol before a colonoscopy influences the safety and success of the screening. Learn more about the effects of drinking before a colonoscopy in our latest blog.
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet millions of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
Colonoscopies are no glamorous procedure. To add to its unpleasantness, the procedure involves a comprehensive preparation regimen that boosts its accuracy. One of the many instructions in the prep booklet for a colonoscopy is to avoid alcohol. While testing our luck is fun and games when buying a lottery ticket, this “no drinking” guideline is one we’ll want to follow.
Understanding the risks of drinking before a colonoscopy will help us follow protocols and have a safe procedure. Let’s take a good look (no pun intended) at if and when it’s okay to drink before a colonoscopy.

A colonoscopy is a screening procedure that is used to check the large intestine for abnormalities like swelling, polyps, irritated tissue, and diseases. To do this, they insert a colonoscope — a flexible tube with a tiny camera on the end — through the rectum to view the inside of our colon and surrounding areas.
Although it’s relatively quick (typically under an hour), a colonoscopy is considered an invasive procedure that requires anesthesia and a lengthy pre-procedure regimen that ensures the physician gets a clear view of our colon. Standard colonoscopy preparation includes limiting certain substances. Let’s take a closer look at what these are.
Preparation for a colonoscopy typically starts three to four days before the scheduled procedure. However, it’s always important to check with our treatment team for specific instructions.
To ensure that the gastroenterologist has an unobstructed view of our colon, we have to flush out our intestine. To do this, we are instructed to avoid certain foods and substances in the days leading up to the procedure:
Avoiding these four things will give us the best chance of a successful procedure. But let’s dive into how alcohol, specifically, could complicate our colonoscopy.
Most clear liquids are permitted up to two to four hours before the procedure. While most alcoholic beverages are clear liquids, they are still not allowed.
Why? There are several reasons. Alcohol dehydrates us, impacts anesthesia (the stuff that keeps us safe and asleep), and thins our blood. All of these can complicate what would normally be a standard procedure.
But what about just one beer? Can one sip of wine hurt?
When it comes to preparing for a colonoscopy (or any procedure for that matter), all alcohol is created equal.
Spirits, indeed, contain higher alcohol by volume, but any amount of alcohol can impact a colonoscopy. Lower-alcohol beverages such as wine or beer may produce less of an impact, but any amount of alcohol can have serious adverse effects.
People get colonoscopies for one reason: to detect abnormalities. If the doctor cannot get a clear picture, the whole procedure is pointless. When we drink before the procedure, we complicate the screening in multiple ways:
Drinking before a colonoscopy opens the door to complications that can be fatal. It is imperative that we tell our medical team if we have had anything to drink in the days leading up to our procedure. We might be hesitant to say anything for fear they will reschedule the procedure, but rescheduling is a small price to pay to avoid complications.

We should clear our calendars of all happy hours, weddings, or other festivities two to three days before a colonoscopy. A liquid diet and bowel emptying preparation typically start two days before colonoscopy procedures are scheduled. While avoiding alcohol for a longer period before a colonoscopy is beneficial, ensuring our last drink is at least 48 hours before is crucial for our safety.
Chronic drinking is also shown to impact anesthesia, regardless of following proper protocols. Be sure to communicate clearly with the operating physician and request individual direction if needed. Colonoscopy prep seems like it involves a lot of “no’s.” Let’s get into some “yes’s” and alternatives to alcohol.
Colonoscopy prep can be unpleasant, but it doesn’t have to be miserable. As long as the beverage is non-alcoholic and meets the clear liquid criteria, we can still enjoy it. There are plenty of alternatives that won’t impact our colonoscopy:
Including variety in our clear liquid diet helps make the days leading up to our procedure less miserable. Water can get a bit old after two days of just that (even if it is the liquid of life). These alternatives can help us avoid alcohol the days before a colonoscopy, but what do we do if we slip up?
If we do accidentally have a drink within 48 hours of our colonoscopy, the first thing to do is note the time of our last drink. We can then inform our treatment team to receive further guidance on how to proceed. If necessary, the colonoscopy can be postponed to a later date.
We’ve warned against drinking before the procedure, but what about after?
Drinking right after a colonoscopy may not pose an immediate risk to our health, but it may lead to adverse symptoms and produce complications during recovery.
It may take hours or days to fully metabolize anesthesia. If we drink while anesthesia is still in our system, our liver may not be able to keep up. This can lead to increased side effects from anesthesia drugs and hangover symptoms from alcohol.
Furthermore, if any abnormalities are discovered and removed during the procedure, we might be prescribed medications. Drinking after the operation can interact with prescribed medications and also impact recovery.
When dealing with invasive procedures, the fewer complications the better. We’ve determined that alcohol is one of these complications that negatively influences the safety and outcome of colonoscopy procedures. To set us up for success, we can make intentional choices during colonoscopy preparation.
Implementing safe practices leading up to any medical procedure helps things go more smoothly. Here are four tips we can keep in our toolbox for colonoscopies and other medical procedures:
A colonoscopy and the prep leading up to it can be a pain in the butt (pun intended), but a successful procedure can help catch issues before they get more serious. The procedure is short but open to a host of complications when pre-procedure guidelines aren’t followed. One of these procedures is avoiding alcohol. We may think that a sip of wine can’t hurt, but any amount of alcohol before a colonoscopy can have detrimental effects on our safety and the conclusiveness of the test. Thankfully, there are plenty of alternatives to alcohol that we can still enjoy during colonoscopy prep. Avoid alcohol and follow protocol!
Colonoscopies are no glamorous procedure. To add to its unpleasantness, the procedure involves a comprehensive preparation regimen that boosts its accuracy. One of the many instructions in the prep booklet for a colonoscopy is to avoid alcohol. While testing our luck is fun and games when buying a lottery ticket, this “no drinking” guideline is one we’ll want to follow.
Understanding the risks of drinking before a colonoscopy will help us follow protocols and have a safe procedure. Let’s take a good look (no pun intended) at if and when it’s okay to drink before a colonoscopy.

A colonoscopy is a screening procedure that is used to check the large intestine for abnormalities like swelling, polyps, irritated tissue, and diseases. To do this, they insert a colonoscope — a flexible tube with a tiny camera on the end — through the rectum to view the inside of our colon and surrounding areas.
Although it’s relatively quick (typically under an hour), a colonoscopy is considered an invasive procedure that requires anesthesia and a lengthy pre-procedure regimen that ensures the physician gets a clear view of our colon. Standard colonoscopy preparation includes limiting certain substances. Let’s take a closer look at what these are.
Preparation for a colonoscopy typically starts three to four days before the scheduled procedure. However, it’s always important to check with our treatment team for specific instructions.
To ensure that the gastroenterologist has an unobstructed view of our colon, we have to flush out our intestine. To do this, we are instructed to avoid certain foods and substances in the days leading up to the procedure:
Avoiding these four things will give us the best chance of a successful procedure. But let’s dive into how alcohol, specifically, could complicate our colonoscopy.
Most clear liquids are permitted up to two to four hours before the procedure. While most alcoholic beverages are clear liquids, they are still not allowed.
Why? There are several reasons. Alcohol dehydrates us, impacts anesthesia (the stuff that keeps us safe and asleep), and thins our blood. All of these can complicate what would normally be a standard procedure.
But what about just one beer? Can one sip of wine hurt?
When it comes to preparing for a colonoscopy (or any procedure for that matter), all alcohol is created equal.
Spirits, indeed, contain higher alcohol by volume, but any amount of alcohol can impact a colonoscopy. Lower-alcohol beverages such as wine or beer may produce less of an impact, but any amount of alcohol can have serious adverse effects.
People get colonoscopies for one reason: to detect abnormalities. If the doctor cannot get a clear picture, the whole procedure is pointless. When we drink before the procedure, we complicate the screening in multiple ways:
Drinking before a colonoscopy opens the door to complications that can be fatal. It is imperative that we tell our medical team if we have had anything to drink in the days leading up to our procedure. We might be hesitant to say anything for fear they will reschedule the procedure, but rescheduling is a small price to pay to avoid complications.

We should clear our calendars of all happy hours, weddings, or other festivities two to three days before a colonoscopy. A liquid diet and bowel emptying preparation typically start two days before colonoscopy procedures are scheduled. While avoiding alcohol for a longer period before a colonoscopy is beneficial, ensuring our last drink is at least 48 hours before is crucial for our safety.
Chronic drinking is also shown to impact anesthesia, regardless of following proper protocols. Be sure to communicate clearly with the operating physician and request individual direction if needed. Colonoscopy prep seems like it involves a lot of “no’s.” Let’s get into some “yes’s” and alternatives to alcohol.
Colonoscopy prep can be unpleasant, but it doesn’t have to be miserable. As long as the beverage is non-alcoholic and meets the clear liquid criteria, we can still enjoy it. There are plenty of alternatives that won’t impact our colonoscopy:
Including variety in our clear liquid diet helps make the days leading up to our procedure less miserable. Water can get a bit old after two days of just that (even if it is the liquid of life). These alternatives can help us avoid alcohol the days before a colonoscopy, but what do we do if we slip up?
If we do accidentally have a drink within 48 hours of our colonoscopy, the first thing to do is note the time of our last drink. We can then inform our treatment team to receive further guidance on how to proceed. If necessary, the colonoscopy can be postponed to a later date.
We’ve warned against drinking before the procedure, but what about after?
Drinking right after a colonoscopy may not pose an immediate risk to our health, but it may lead to adverse symptoms and produce complications during recovery.
It may take hours or days to fully metabolize anesthesia. If we drink while anesthesia is still in our system, our liver may not be able to keep up. This can lead to increased side effects from anesthesia drugs and hangover symptoms from alcohol.
Furthermore, if any abnormalities are discovered and removed during the procedure, we might be prescribed medications. Drinking after the operation can interact with prescribed medications and also impact recovery.
When dealing with invasive procedures, the fewer complications the better. We’ve determined that alcohol is one of these complications that negatively influences the safety and outcome of colonoscopy procedures. To set us up for success, we can make intentional choices during colonoscopy preparation.
Implementing safe practices leading up to any medical procedure helps things go more smoothly. Here are four tips we can keep in our toolbox for colonoscopies and other medical procedures:
A colonoscopy and the prep leading up to it can be a pain in the butt (pun intended), but a successful procedure can help catch issues before they get more serious. The procedure is short but open to a host of complications when pre-procedure guidelines aren’t followed. One of these procedures is avoiding alcohol. We may think that a sip of wine can’t hurt, but any amount of alcohol before a colonoscopy can have detrimental effects on our safety and the conclusiveness of the test. Thankfully, there are plenty of alternatives to alcohol that we can still enjoy during colonoscopy prep. Avoid alcohol and follow protocol!

Organic cane alcohol can sound like a better choice than conventional grain alcohol. But that’s not the case. Check out our latest blog for more info on the adverse effects of cane alcohol.
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet millions of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
Organic, natural, and non-GMO, among many other labels, are supposedly “better” alternatives to a normal generic product. But what about organic cane alcohol? We know that there are harmful effects of drinking alcoholic beverages and may be looking for a better option.
On the surface, cane alcohol can seem like a viable alternative to other alcoholic beverages we may be more familiar with. However, a deeper dive into its adverse effects may suggest otherwise. Let’s further examine what it is and evaluate if it's a healthier option so we can make more well-informed alcohol choices.

Cane alcohol is alcohol that is made from the sugar cane plant. The two main types of cane alcohol are pure cane alcohol and alcohol made from molasses — which we know as rum.
Pure cane alcohol is made from organic sugar cane. The plant is cut and milled with water to produce raw sugar cane juice, which is then heated to remove the impurities. The sugar cane juice is fermented and distilled multiple times to reach a high level of purity, which organic cane alcohol is known for. Rum, on the other hand, is made from fermentation of molasses, a byproduct of the sugar-making process. It falls under the general category of cane alcohol but is distinct from pure cane alcohol.
Pure organic cane alcohol is known for its neutral taste and purity, making it adaptable to many different uses.
Organic cane alcohol is used in a variety of different industries aside from alcoholic beverage companies. Some of its other uses include the following:
Cane alcohol is versatile, not just in its applications within different industries but also in the types of alcoholic beverages it can create.
Pure cane alcohol, which is pure alcohol at 98% alcohol by volume, is used to make distilled alcoholic beverages such as liqueurs, vodkas, and bitters. Legality varies widely by country and region. When purchasing or consuming cane alcohol, it’s important to check regional regulations.
Cane alcoholic drinks are extremely popular in Brazil. Three of the most notable include cachaça, aguardente de cana, and simple alcoholic sugar cane distillate — all made from sugar cane juice. Each varies in ABV and has its own minimum and maximum ABV regulations in Brazil.
While cane alcoholic beverages are popular in Brazil, rum is the most popular cane alcohol approved for consumption in the U.S. According to the Alcohol and Tobacco Tax and Trade Bureau (TTB), rum may not exceed 95% alcohol by volume but can vary in regulations depending on the area.
So is cane alcohol really so bad, given its popularity and various uses?
Organic sugar cane alcohol in the context of cosmetics preservation and pharmaceuticals can be a great alternative to synthetically produced chemicals. However, in the context of alcoholic beverages, being derived from an organic plant doesn’t negate the toxicity of alcohol.
Just the way a basket of french fries or a carton of apple juice doesn't count as our serving of fruits and vegetables for the day, alcohol made from a plant doesn’t exactly make it a green juice. Organic cane alcohol has the same harmful effects as other alcoholic beverages that are made from other plants. It goes through the same fermentation process that creates alcohol by turning sugar into ethanol. When we consume ethanol, it’s broken down into a toxic compound known as acetaldehyde — the culprit of many of alcohol’s detrimental effects.
A particular study focused on sugar cane spirits found that their consumption produced anxiolytic-like effects in mice, reducing their inhibitions and causing them to behave out of the ordinary, while also causing them liver injury. While the alcohol content in organic cane alcohol can vary depending on the type of alcoholic beverage, it still contains toxic compounds that harm our health.
So, we’ve learned that cane alcohol has the same harmful effects as grain alcohol, but let’s dive into the difference a little more.
Grain and cane alcohol are similar in that they have various uses, and they’re both derived from plants: cane alcohol is from sugar cane and grain alcohol is from other grains such as corn, wheat, or barley. But grain and cane alcohol are distinct due to three main differences:
While sugar cane alcohol has some benefits over grain alcohol, consuming cane alcohol is still associated with many risks.
Sugar cane alcohol is just like any other alcohol in that it is a toxic compound that opens the door to many different complications and consequences. Some of the issues that drinking alcohol leads to include the following:
Due to the way sugar cane alcohol is presented, it also comes with its own risk factors.
Let’s clear up some of the confusion surrounding organic cane alcohol so we can make well-informed decisions about drinking.
Cane alcohol, specifically organic cane alcohol, is associated with many common misconceptions, such as:
After we understand exactly what cane alcohol is we are able to consume more mindfully and safely.

As we’ve learned, consuming cane alcohol comes with many risks. If we choose to drink cane alcohol, we can limit its negative consequences through mindful drinking practices:
Mindfully approaching cane alcohol and alcohol in general can help minimize its adverse effects. However, at the end of the day, alcohol is still alcohol, no matter if it’s organic or derived from a sugar cane plant.
We may have all been duped at some point in our lives by product labeling. Free-range, all-natural, and organic may not always be what we think. Debunking common myths about organic cane alcohol helps us see it for what it is. Pure cane alcohol is a useful, eco-friendly substance when used in the cosmetics, pharmaceutical, and food industries. However, as an alcoholic beverage, organic cane alcohol has the same toxic effects as grain alcohol, which we may be more familiar with. The lack of clarity and regulations surrounding cane alcohol makes it even more dangerous than other alcoholic beverages. Gain a better relationship with alcohol by cutting back, whether it be from grain or cane!
Organic, natural, and non-GMO, among many other labels, are supposedly “better” alternatives to a normal generic product. But what about organic cane alcohol? We know that there are harmful effects of drinking alcoholic beverages and may be looking for a better option.
On the surface, cane alcohol can seem like a viable alternative to other alcoholic beverages we may be more familiar with. However, a deeper dive into its adverse effects may suggest otherwise. Let’s further examine what it is and evaluate if it's a healthier option so we can make more well-informed alcohol choices.

Cane alcohol is alcohol that is made from the sugar cane plant. The two main types of cane alcohol are pure cane alcohol and alcohol made from molasses — which we know as rum.
Pure cane alcohol is made from organic sugar cane. The plant is cut and milled with water to produce raw sugar cane juice, which is then heated to remove the impurities. The sugar cane juice is fermented and distilled multiple times to reach a high level of purity, which organic cane alcohol is known for. Rum, on the other hand, is made from fermentation of molasses, a byproduct of the sugar-making process. It falls under the general category of cane alcohol but is distinct from pure cane alcohol.
Pure organic cane alcohol is known for its neutral taste and purity, making it adaptable to many different uses.
Organic cane alcohol is used in a variety of different industries aside from alcoholic beverage companies. Some of its other uses include the following:
Cane alcohol is versatile, not just in its applications within different industries but also in the types of alcoholic beverages it can create.
Pure cane alcohol, which is pure alcohol at 98% alcohol by volume, is used to make distilled alcoholic beverages such as liqueurs, vodkas, and bitters. Legality varies widely by country and region. When purchasing or consuming cane alcohol, it’s important to check regional regulations.
Cane alcoholic drinks are extremely popular in Brazil. Three of the most notable include cachaça, aguardente de cana, and simple alcoholic sugar cane distillate — all made from sugar cane juice. Each varies in ABV and has its own minimum and maximum ABV regulations in Brazil.
While cane alcoholic beverages are popular in Brazil, rum is the most popular cane alcohol approved for consumption in the U.S. According to the Alcohol and Tobacco Tax and Trade Bureau (TTB), rum may not exceed 95% alcohol by volume but can vary in regulations depending on the area.
So is cane alcohol really so bad, given its popularity and various uses?
Organic sugar cane alcohol in the context of cosmetics preservation and pharmaceuticals can be a great alternative to synthetically produced chemicals. However, in the context of alcoholic beverages, being derived from an organic plant doesn’t negate the toxicity of alcohol.
Just the way a basket of french fries or a carton of apple juice doesn't count as our serving of fruits and vegetables for the day, alcohol made from a plant doesn’t exactly make it a green juice. Organic cane alcohol has the same harmful effects as other alcoholic beverages that are made from other plants. It goes through the same fermentation process that creates alcohol by turning sugar into ethanol. When we consume ethanol, it’s broken down into a toxic compound known as acetaldehyde — the culprit of many of alcohol’s detrimental effects.
A particular study focused on sugar cane spirits found that their consumption produced anxiolytic-like effects in mice, reducing their inhibitions and causing them to behave out of the ordinary, while also causing them liver injury. While the alcohol content in organic cane alcohol can vary depending on the type of alcoholic beverage, it still contains toxic compounds that harm our health.
So, we’ve learned that cane alcohol has the same harmful effects as grain alcohol, but let’s dive into the difference a little more.
Grain and cane alcohol are similar in that they have various uses, and they’re both derived from plants: cane alcohol is from sugar cane and grain alcohol is from other grains such as corn, wheat, or barley. But grain and cane alcohol are distinct due to three main differences:
While sugar cane alcohol has some benefits over grain alcohol, consuming cane alcohol is still associated with many risks.
Sugar cane alcohol is just like any other alcohol in that it is a toxic compound that opens the door to many different complications and consequences. Some of the issues that drinking alcohol leads to include the following:
Due to the way sugar cane alcohol is presented, it also comes with its own risk factors.
Let’s clear up some of the confusion surrounding organic cane alcohol so we can make well-informed decisions about drinking.
Cane alcohol, specifically organic cane alcohol, is associated with many common misconceptions, such as:
After we understand exactly what cane alcohol is we are able to consume more mindfully and safely.

As we’ve learned, consuming cane alcohol comes with many risks. If we choose to drink cane alcohol, we can limit its negative consequences through mindful drinking practices:
Mindfully approaching cane alcohol and alcohol in general can help minimize its adverse effects. However, at the end of the day, alcohol is still alcohol, no matter if it’s organic or derived from a sugar cane plant.
We may have all been duped at some point in our lives by product labeling. Free-range, all-natural, and organic may not always be what we think. Debunking common myths about organic cane alcohol helps us see it for what it is. Pure cane alcohol is a useful, eco-friendly substance when used in the cosmetics, pharmaceutical, and food industries. However, as an alcoholic beverage, organic cane alcohol has the same toxic effects as grain alcohol, which we may be more familiar with. The lack of clarity and regulations surrounding cane alcohol makes it even more dangerous than other alcoholic beverages. Gain a better relationship with alcohol by cutting back, whether it be from grain or cane!

Wondering can I drink alcohol after having a stent fitted? Learn the facts, risks, and safe steps for heart health after your stent procedure.
You’ve come to the right place! Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet millions of fellow Reframers in our 24/7 forum and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
We’ve all heard the myth that a glass of red wine is good for the heart. But after a major medical event like a stent placement, that old advice gets complicated. You might be asking yourself, “Can I drink alcohol after having a stent fitted?” The answer isn’t as simple as you might think, and it’s crucial to understand the risks during this fragile recovery period. We'll look at the science-backed facts, helping you understand why moderation or abstinence is so important for protecting your newly repaired arteries and overall cardiovascular health.
If you’ve ever had a stent fitted or know someone who has, you may be wondering if you’ll ever be able to get back to your old self. “Do I have to give up Chick-fil-A for good?” “Will I be able to get back to long-distance running?” “Can I drink alcohol after having a stent fitted?”
Only your doctor can definitively answer questions about your prognosis, but we can touch on the alcohol-related side of things. Let’s explore and find out: Can you drink alcohol with stents in your heart? And how soon after a heart attack can you drink alcohol?
A stent is a small tube that a doctor installs inside one of our arteries to open it up after it’s been blocked by either cholesterol or fat buildup that was limiting — or, in the case of a heart attack, completely stopping — blood from flowing through our heart and to the rest of our body.
Once a doctor removes the buildup that was causing the blockage in the artery, a stent is then placed to prevent further stress to that area. Think of your coronary arteries as mining tunnels — a stent acts as a support structure to keep the tunnel from collapsing.
Simply put, our coronary arteries are a big deal! A completely blocked coronary artery will cause a heart attack. The classic signs and symptoms of a heart attack include crushing chest pain or pressure, shoulder or arm pain, shortness of breath, and sweating. Women are more likely to have atypical symptoms, such as neck or jaw pain, nausea, or unusual fatigue.
If you are experiencing any of these symptoms, call 911 immediately, especially if you’ve already had a heart attack or have a stent in place.
Stents are typically used for those of us who have experienced heart problems such as a heart attack. They’re also used when we have advanced atherosclerosis, a condition that involves plaque collecting inside an artery. However, stents can be used for other conditions that aren’t related to the heart but are related to circulation and blood flow.
Here are some additional conditions that may require a stent:
Just like stents help increase blood flow when our hearts are blocked, they also help increase blood flow through our bodies when we have another blockage, such as deep vein thrombosis (a blood clot in your leg, arm, or pelvis) or an aneurysm. They can also help with blockages in airways for someone experiencing a blockage in their lungs, for example. However, stents are most commonly used to prevent further damage after a heart attack.
As we mentioned, stents are often used after heart attacks to shore up the structure of the blood vessel that was blocked during the attack. Unfortunately, alcohol has many detrimental effects on the heart. But can alcohol cause cardiac arrest?
It's no secret that alcohol can contribute to weight gain, but the reasons why are often overlooked. Alcoholic drinks are packed with what are often called “empty calories” because they offer little nutritional value. A single glass of wine or a pint of beer can have a surprising number of calories, and since our bodies prioritize processing alcohol over burning fat, this can lead to weight gain over time. This extra weight puts additional strain on our cardiovascular system, increasing the risk of high blood pressure and other heart issues. If you're curious about the impact of your own habits, you can calculate not just the financial cost but also the hidden calorie cost of drinking. Understanding this connection is a key step in protecting our heart health, especially for those of us who have or are at risk for heart conditions.
Drinking alcohol is linked to a number of poor health outcomes, including heart conditions. Excessive alcohol intake can lead to high blood pressure, heart failure, or stroke — but can alcohol give you a heart attack?
Excessive drinking can also contribute to cardiomyopathy, a disorder that affects the heart muscle, and can contribute to conditions associated with heart attacks, such as diabetes, obesity, clotting, high blood pressure, and atrial fibrillation.
In general, it’s best to avoid alcohol if you’re concerned about heart health. And if you’ve already had a heart attack, it’s even more important.
We don’t recommend drinking alcohol after a heart attack or stent placement, but for those of us who do choose to consume alcohol, it’s important to exercise caution. Speak to a healthcare provider about your individual case and medical history. For some of us, it may be safe to drink a glass of wine after a week or so; whereas, for others, it may be best to wait up to a month or more or to cut out alcohol completely.
The takeaway is this: If we choose to drink alcohol, it’s important to practice moderation. Remember, there is no “safe” level of alcohol, only best practices for reducing the risk of harm.
Now, back to stents!
The clinical term for a heart stent procedure is percutaneous coronary intervention (PCI) or angioplasty. The procedure is usually done using a local anesthetic, though we’ll likely be given medication to help us relax.
An inflatable catheter (called a “balloon”) is inserted into a blood vessel, typically through our wrist. Once the doctor determines the target location, the stent is placed using special X-ray equipment. The balloon is inflated, and the stent is expanded around it. Then the balloon is deflated, leaving the stent in place.
After the procedure, we will likely be required to take blood thinners or other medications to ensure our arteries remain open and the blood continues to flow freely, as it should.
It’s completely normal to wonder about the road ahead after any heart procedure. You want to know when you can get back to your routine, your hobbies, and just feeling like yourself again. The recovery timeline can vary quite a bit from person to person, depending on your overall health and the specifics of your situation. The most important thing you can do is to follow the advice of your healthcare team. They will give you a personalized plan with specific instructions on activity levels, medications, and follow-up appointments. Understanding the general timeline, however, can help you set realistic expectations. A key factor in that timeline is the type of procedure you had, as the recovery from a stent is very different from that of more invasive surgeries.
A stent procedure is much less invasive than open-heart surgery, and that difference is clearly reflected in the recovery time. Many people who receive a stent are able to return to their normal activities within a week or two, though full recovery can sometimes take longer. Light activity is often encouraged to help with healing. In contrast, open-heart surgery is a major operation that requires a much longer and more intensive recovery, often lasting several weeks to months. Activity is usually very limited in the beginning. While both procedures often require medications like blood thinners to prevent complications, the overall path back to full strength is significantly shorter and less demanding after a stent placement.
The recovery process after getting a stent fitted depends on the seriousness of the preceding event. It’s always important to speak with our healthcare provider and ask detailed questions. To protect our well-being, it’s important to be honest and open with our doctor.
But generally, here are a few things to avoid at least for a few days after a stent procedure:
All of this sounds like a drag — but hey, it’s better than the alternative! After your recovery period, you’ll be able to get back to your normal self. However, you will likely have to adjust to a different lifestyle with healthier choices. Say goodbye to your regular fried chicken sandwich for lunch!
But wait, can you drink alcohol with stents in your heart? Let’s find out!
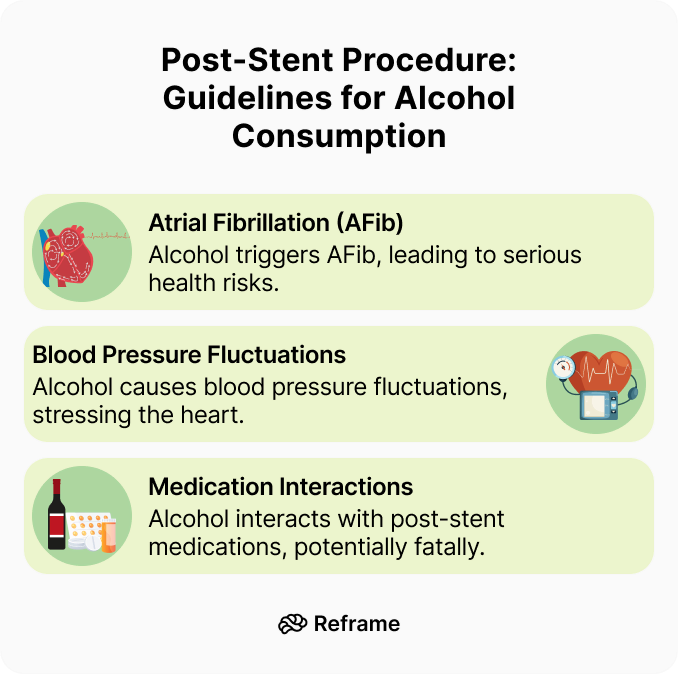
We’ve established that moderation is key, especially after a heart procedure. But what about binge drinking? This isn't just about having a few too many on a Saturday night; it’s about consuming a large amount of alcohol in a short time, which puts immense stress on your body — particularly your heart. For someone with a stent, this is especially risky. A sudden influx of alcohol can quickly raise your blood pressure and even trigger irregular heartbeats. This puts a dangerous strain on your newly repaired arteries, potentially counteracting the very benefits the stent was placed to provide. It also reminds us that any amount of alcohol carries some risk, and binge drinking significantly magnifies those dangers, especially when it comes to interacting with essential medications like blood thinners.
As we’ve reiterated throughout the article, we recommend speaking with your doctor about this before you go for a drink. Everyone’s recovery process is different, and we all react differently to medical procedures. Depending on overall health, a few drinks might not kill us, but drinking alcohol at this stage poses a lot of risks. Here are the big ones:
Let’s face it, if we’ve just had a stent placed, we probably have more than the average health considerations to take into account! We’re healing not only from the procedure, but we’re in the process of recovering from whatever condition led to the placement of the stent. To optimize heart and blood health and give our body the best chance at healing, it’s best to take it easy and avoid stressing our body out with alcohol.
The conversation around alcohol and heart health can feel confusing, with some studies suggesting benefits while others highlight major risks. It’s especially complicated after a procedure like a stent placement. Let's break down what some of the research indicates, but remember, these are general findings. Your personal health situation is unique, and your doctor's advice is always the most important guide for your recovery and long-term well-being. This is a time to be extra mindful about what you put into your body, and understanding the full picture can help you make the best choices for your healing process.
Interestingly, some research has explored the effects of alcohol on arteries after stenting. One study found that men who drank moderately had a lower chance of their arteries re-narrowing compared to those who drank very little. In that study, only 23% of moderate drinkers needed a repeat procedure, while 43% of very light drinkers did. The researchers suggested that moderate alcohol consumption might help prevent arteries from narrowing again after angioplasty. However, it's crucial to see this as a single data point and not a prescription to drink for your health. The risks associated with alcohol, especially during a fragile recovery period, can easily cancel out any potential, and still debated, benefits.
You may have also heard that alcohol can be good for your cholesterol. Some studies, particularly those looking at red wine, suggest that light to moderate drinking might help your heart by raising HDL, or "good" cholesterol. It’s thought that this could also help with inflammation in the body. While this is a common talking point, the potential benefits are often small and can be easily outweighed by the negative effects of alcohol, especially after a major heart event. You can get similar or better cholesterol-managing benefits from diet and exercise, without the added risks that come with drinking alcohol.
While the potential benefits we just discussed are debated, the risks are much more clear-cut. For many people, especially those with specific health factors, drinking alcohol after a stent isn't just a bad idea—it's dangerous. These aren't suggestions but firm guidelines for protecting your health and ensuring your recovery is successful. If any of the following situations apply to you, abstaining from alcohol is the safest and smartest choice you can make for your heart. This is where being honest with yourself and your medical team is absolutely essential for your long-term health and peace of mind.
Your overall health picture is the most important factor. You should not drink alcohol at all if you have conditions like liver problems or uncontrolled high blood pressure. Most importantly, you need to consider your medications. If you are taking blood thinners or other heart medications, alcohol can cause dangerous interactions, increasing bleeding risks or causing unpredictable changes in blood pressure. In fact, alcohol can interfere with all the drugs typically used after a stent placement. At high amounts, this interaction can be fatal. Always talk to your doctor about whether it's safe for you to drink. Your life could depend on it.
Seek medical attention or dial 911 if you experience any of these symptoms after a stent procedure:
Although the angioplasty and stent will help the blood circulate better, that doesn’t mean we’re completely off the hook! We still need to do our part to live a healthy lifestyle. That means eating healthy foods, exercising, avoiding tobacco products, and limiting alcohol.
Moderation is key to overall health and a healthy relationship with alcohol. We may have heard the term “moderation” thrown around a lot, but what does it actually mean?
Moderation means consuming alcoholic beverages in reasonable limits that mitigate risks to health. Moderation implies a balanced and controlled approach to drinking. It’s typically defined as less than one drink per day for women and fewer than two drinks per day for men.
Moderation entails making intentional and informed decisions about the quantity and frequency of our alcohol intake. Mindful drinking prioritizes our health goals and allows us to avoid negative consequences such as impaired judgment or dependency. To learn more about how mindful drinking benefits overall well-being, check out our article about health benefits of cutting back on drinking.
Luckily, life offers many options for enjoying ourselves without drinking alcohol. Let’s take a look at how we can protect our heart health with sobriety!
It’s easy to hear “one drink a day” and lose track of what that actually means. Is a pint of high-alcohol craft beer one drink? What about that generous pour of wine at dinner? In the US, a “standard” drink contains about 14 grams of pure alcohol. This typically looks like 12 ounces of regular beer (at 5% ABV), 5 ounces of wine (at 12% ABV), or 1.5 ounces of distilled spirits like vodka or whiskey (at 40% ABV). Understanding these measurements is the first step toward accurately tracking your intake and making sure your version of “one drink” aligns with medical guidelines. Knowing exactly how much you’re consuming can help you better understand its effect on your blood alcohol content and your heart.
If you choose to drink after a stent procedure, doing so with intention is crucial for protecting your heart. This is the core of mindful drinking — it’s about being present and making conscious choices rather than drinking out of habit. Before you pour a drink, ask yourself why you want it. Is it to relax, to celebrate, or just because it’s there? Consider opting for drinks that are lower in alcohol and sugar, as sugary cocktails and high-calorie beers can put additional stress on your body. The goal is to shift your relationship with alcohol from a reactive one to a proactive one, where your long-term health is always the priority.
One of the most effective strategies for safer drinking is to manage your pace and stay hydrated. A simple but powerful rule is to alternate every alcoholic beverage with a full glass of water. This practice does two important things: it prevents dehydration, which can strain your system, and it naturally slows down your rate of consumption. Giving your body more time to process the alcohol helps prevent sudden spikes in blood pressure, which is especially important when you’re protecting your heart. This simple habit makes it easier to stay within moderation and reinforces the benefits you gain on the days you choose not to drink at all.
Many of us have heard that a glass of red wine is good for heart health. So is that an invitation to drink our daily glass (and then some) if we’re on a path of healing our heart?
Think again! We wish it were that simple. Most of those studies have been debunked, or it was proven that we get all the benefits of drinking red wine by just drinking non-alcoholic grape juice (without the negative effects of alcohol).
Luckily, there are heart-healthy ways to enjoy a “drink” without alcohol. In fact, this time of healing can stand as the beginning of a greater journey toward sobriety or mindfully reduced drinking. Let’s look at some healthy alternatives to drinking alcohol after getting a stent placed.
Whether we’re recovering from heart surgery or taking a break from drinking for other health reasons, there are many benefits to an alcohol-free lifestyle worth exploring.
Although it’s not technically a “no-no” to drink alcohol after having a stent fitted, the best idea is to exercise caution with anything that could potentially put us at risk or cause any complications — especially when we’re dealing with matters of the heart! Our hearts are really the heartbeat of our entire well-being. As always, Reframe is here to help us all make positive changes that benefit our health.
A stent is a fantastic piece of medical technology, but it's important to remember that it doesn't cure the underlying coronary artery disease. It's a fix for a specific blockage, not a full-body reset. This means the risk of future heart problems, including another heart attack, is still there if lifestyle factors aren't addressed. This is especially true when it comes to alcohol. If you're focused on your heart health, it's generally best to limit or avoid alcohol, and this becomes even more critical after you've had a heart attack. Making conscious choices now is your best defense for the future.
You're probably eager to get back to your routine, and you will! The key is to follow your doctor's timeline. They will give you specific instructions on when you can drive, return to work, and tackle your usual chores. This isn't a time for guesswork or pushing yourself too hard. To protect your well-being, it’s essential to be completely honest and open with your doctor about how you're feeling and what you're capable of. They are your best resource for navigating this recovery phase safely. Your body has been through a lot, so give it the time it needs to heal properly.
Once you get the green light from your doctor, easing back into physical activity is a huge step toward long-term heart health. Start with gentle activities like walking. The goal isn't to run a marathon next week, but to slowly build back your strength and stamina. After your initial recovery, you'll be able to get back to being your normal self, but it will likely involve adjusting to a new lifestyle with healthier choices. Think of it as creating a new, stronger foundation for your health, where regular, enjoyable movement is a non-negotiable part of your day.
This is a common question that many people feel shy about asking, but it's a perfectly normal part of life and recovery. Most doctors advise that you can resume sexual activity when you feel ready—often when you can handle mild to moderate exercise, like climbing two flights of stairs, without getting breathless or having chest pain. Ultimately, we still need to do our part to live a healthy lifestyle. That means focusing on heart-healthy foods, getting regular exercise, avoiding tobacco, and limiting alcohol, all of which contribute to your overall stamina and well-being.
Planning a trip? Flying involves changes in air pressure and can be physically demanding (hello, lugging suitcases!), so it's wise to check with your doctor before booking a flight. They'll consider your specific situation, the length of the flight, and how your recovery is progressing. There's no one-size-fits-all answer, so it's crucial to speak to a healthcare provider about your individual case and medical history. They can give you the personalized advice you need to travel safely and with peace of mind.
Your doctor might recommend a cardiac rehabilitation program, and if they do, it's a fantastic opportunity. These programs are medically supervised and designed to help you recover safely while improving your overall cardiovascular health. They typically include structured exercise, education on heart-healthy living (like nutrition and stress management), and counseling to help you adjust. Think of it as having a dedicated team of experts guiding you through the process of building a stronger, healthier life after your stent procedure. It’s a proactive step that can make a huge difference in your long-term outcome.
This is non-negotiable. Your doctor will likely prescribe medications like blood thinners or cholesterol-lowering drugs to prevent new clots and keep your arteries open. It is absolutely critical to take these exactly as prescribed. This is also where alcohol can be particularly dangerous. Alcohol interacts with all the drugs typically used after a stent placement, which can lead to serious complications. Mixing them can alter how the medications work and put unnecessary strain on your body. Sticking to your medication plan is one of the most important things you can do for your heart.
A stent procedure is the beginning of a new chapter in your health journey, not the end of the story. Regular follow-up appointments with your doctor are essential to monitor your progress, check your blood pressure and cholesterol, and make any necessary adjustments to your treatment plan. These checkups are your chance to ask questions and stay on track. If you do choose to drink alcohol, these appointments are the time to discuss it with your doctor. The key takeaway is that if we choose to drink, it’s vital to practice moderation and ensure it aligns with your overall health plan.
What we eat has a direct impact on our heart. Adopting a heart-healthy diet, like the Mediterranean diet, is one of the best changes you can make. This means filling your plate with fruits, vegetables, whole grains, lean proteins (like fish and chicken), and healthy fats (like olive oil and avocados). It also means cutting back on processed foods, saturated fats, trans fats, and excess sodium. This isn't about deprivation; it's about nourishing your body with the fuel it needs to heal and thrive for years to come.
Emotional stress can take a physical toll on your heart by raising blood pressure and heart rate. Finding healthy ways to manage stress is a crucial part of your recovery. This could be through practices like meditation, deep breathing exercises, yoga, or simply spending time in nature. To give our body the best chance at healing, it’s best to take it easy and avoid stressing it out with things like alcohol, which can add both physical and emotional strain. Prioritizing relaxation isn't an indulgence—it's a core component of your heart care plan.
You don't have to go through this alone. Leaning on your support system is incredibly important for both your emotional and physical recovery. It’s important to have a support system in place, whether it’s family, friends, or your healthcare team. Talking about your experiences, fears, and successes can make a world of difference. For many, connecting with others who are on a similar journey to improve their health and change their relationship with alcohol can be empowering. The Reframe app, for example, offers a supportive community to help you build these healthy habits.
How soon after my stent procedure can I have a drink? There isn't a single, universal timeline for when it's safe to drink alcohol again. Your personal recovery depends on your overall health, the specifics of your procedure, and the medications you're taking. The first few weeks are a fragile healing period where your body needs to recover without the added stress of processing alcohol. The only person who can give you a definite answer is your doctor, who understands your complete medical picture.
What is the single biggest danger of drinking alcohol with a stent? The most critical risk is how alcohol interacts with your new medication regimen. After a stent, you'll likely be on essential drugs like blood thinners and cholesterol medication. Alcohol can interfere with how these drugs work, potentially increasing your risk of bleeding or causing unpredictable changes in your blood pressure. This interaction isn't just a minor issue; it can have very serious consequences for your heart health.
I've always heard red wine is good for the heart. Does that still apply after a stent? That old piece of advice gets complicated after a major heart event. While some studies have pointed to potential benefits from compounds in red wine, the risks associated with alcohol itself generally outweigh them, especially during recovery. You can get much more reliable heart-healthy benefits from things like a balanced diet and gentle exercise, without adding the strain that alcohol puts on your cardiovascular system.
My procedure was a while ago and I feel fine. Is it still risky to drink? It's great that you're feeling well, but it's important to remember that a stent treats a specific blockage, not the underlying condition of coronary artery disease. Alcohol can still contribute to risk factors like high blood pressure, weight gain, and irregular heart rhythms, which can lead to future problems. Thinking about your long-term heart health is just as important as getting through the initial recovery.
If my doctor and I agree that occasional drinking is okay, what's the safest way to do it? If you choose to drink, the key is to be mindful and intentional. This means knowing what a standard drink size is for your beverage of choice and sticking to strict moderation. A great strategy is to pace yourself by having a full glass of water between each alcoholic drink. This keeps you hydrated and naturally slows you down. The goal is to make a conscious choice that supports your health, not to fall back into old habits.
We’ve all heard the myth that a glass of red wine is good for the heart. But after a major medical event like a stent placement, that old advice gets complicated. You might be asking yourself, “Can I drink alcohol after having a stent fitted?” The answer isn’t as simple as you might think, and it’s crucial to understand the risks during this fragile recovery period. We'll look at the science-backed facts, helping you understand why moderation or abstinence is so important for protecting your newly repaired arteries and overall cardiovascular health.
If you’ve ever had a stent fitted or know someone who has, you may be wondering if you’ll ever be able to get back to your old self. “Do I have to give up Chick-fil-A for good?” “Will I be able to get back to long-distance running?” “Can I drink alcohol after having a stent fitted?”
Only your doctor can definitively answer questions about your prognosis, but we can touch on the alcohol-related side of things. Let’s explore and find out: Can you drink alcohol with stents in your heart? And how soon after a heart attack can you drink alcohol?
A stent is a small tube that a doctor installs inside one of our arteries to open it up after it’s been blocked by either cholesterol or fat buildup that was limiting — or, in the case of a heart attack, completely stopping — blood from flowing through our heart and to the rest of our body.
Once a doctor removes the buildup that was causing the blockage in the artery, a stent is then placed to prevent further stress to that area. Think of your coronary arteries as mining tunnels — a stent acts as a support structure to keep the tunnel from collapsing.
Simply put, our coronary arteries are a big deal! A completely blocked coronary artery will cause a heart attack. The classic signs and symptoms of a heart attack include crushing chest pain or pressure, shoulder or arm pain, shortness of breath, and sweating. Women are more likely to have atypical symptoms, such as neck or jaw pain, nausea, or unusual fatigue.
If you are experiencing any of these symptoms, call 911 immediately, especially if you’ve already had a heart attack or have a stent in place.
Stents are typically used for those of us who have experienced heart problems such as a heart attack. They’re also used when we have advanced atherosclerosis, a condition that involves plaque collecting inside an artery. However, stents can be used for other conditions that aren’t related to the heart but are related to circulation and blood flow.
Here are some additional conditions that may require a stent:
Just like stents help increase blood flow when our hearts are blocked, they also help increase blood flow through our bodies when we have another blockage, such as deep vein thrombosis (a blood clot in your leg, arm, or pelvis) or an aneurysm. They can also help with blockages in airways for someone experiencing a blockage in their lungs, for example. However, stents are most commonly used to prevent further damage after a heart attack.
As we mentioned, stents are often used after heart attacks to shore up the structure of the blood vessel that was blocked during the attack. Unfortunately, alcohol has many detrimental effects on the heart. But can alcohol cause cardiac arrest?
It's no secret that alcohol can contribute to weight gain, but the reasons why are often overlooked. Alcoholic drinks are packed with what are often called “empty calories” because they offer little nutritional value. A single glass of wine or a pint of beer can have a surprising number of calories, and since our bodies prioritize processing alcohol over burning fat, this can lead to weight gain over time. This extra weight puts additional strain on our cardiovascular system, increasing the risk of high blood pressure and other heart issues. If you're curious about the impact of your own habits, you can calculate not just the financial cost but also the hidden calorie cost of drinking. Understanding this connection is a key step in protecting our heart health, especially for those of us who have or are at risk for heart conditions.
Drinking alcohol is linked to a number of poor health outcomes, including heart conditions. Excessive alcohol intake can lead to high blood pressure, heart failure, or stroke — but can alcohol give you a heart attack?
Excessive drinking can also contribute to cardiomyopathy, a disorder that affects the heart muscle, and can contribute to conditions associated with heart attacks, such as diabetes, obesity, clotting, high blood pressure, and atrial fibrillation.
In general, it’s best to avoid alcohol if you’re concerned about heart health. And if you’ve already had a heart attack, it’s even more important.
We don’t recommend drinking alcohol after a heart attack or stent placement, but for those of us who do choose to consume alcohol, it’s important to exercise caution. Speak to a healthcare provider about your individual case and medical history. For some of us, it may be safe to drink a glass of wine after a week or so; whereas, for others, it may be best to wait up to a month or more or to cut out alcohol completely.
The takeaway is this: If we choose to drink alcohol, it’s important to practice moderation. Remember, there is no “safe” level of alcohol, only best practices for reducing the risk of harm.
Now, back to stents!
The clinical term for a heart stent procedure is percutaneous coronary intervention (PCI) or angioplasty. The procedure is usually done using a local anesthetic, though we’ll likely be given medication to help us relax.
An inflatable catheter (called a “balloon”) is inserted into a blood vessel, typically through our wrist. Once the doctor determines the target location, the stent is placed using special X-ray equipment. The balloon is inflated, and the stent is expanded around it. Then the balloon is deflated, leaving the stent in place.
After the procedure, we will likely be required to take blood thinners or other medications to ensure our arteries remain open and the blood continues to flow freely, as it should.
It’s completely normal to wonder about the road ahead after any heart procedure. You want to know when you can get back to your routine, your hobbies, and just feeling like yourself again. The recovery timeline can vary quite a bit from person to person, depending on your overall health and the specifics of your situation. The most important thing you can do is to follow the advice of your healthcare team. They will give you a personalized plan with specific instructions on activity levels, medications, and follow-up appointments. Understanding the general timeline, however, can help you set realistic expectations. A key factor in that timeline is the type of procedure you had, as the recovery from a stent is very different from that of more invasive surgeries.
A stent procedure is much less invasive than open-heart surgery, and that difference is clearly reflected in the recovery time. Many people who receive a stent are able to return to their normal activities within a week or two, though full recovery can sometimes take longer. Light activity is often encouraged to help with healing. In contrast, open-heart surgery is a major operation that requires a much longer and more intensive recovery, often lasting several weeks to months. Activity is usually very limited in the beginning. While both procedures often require medications like blood thinners to prevent complications, the overall path back to full strength is significantly shorter and less demanding after a stent placement.
The recovery process after getting a stent fitted depends on the seriousness of the preceding event. It’s always important to speak with our healthcare provider and ask detailed questions. To protect our well-being, it’s important to be honest and open with our doctor.
But generally, here are a few things to avoid at least for a few days after a stent procedure:
All of this sounds like a drag — but hey, it’s better than the alternative! After your recovery period, you’ll be able to get back to your normal self. However, you will likely have to adjust to a different lifestyle with healthier choices. Say goodbye to your regular fried chicken sandwich for lunch!
But wait, can you drink alcohol with stents in your heart? Let’s find out!
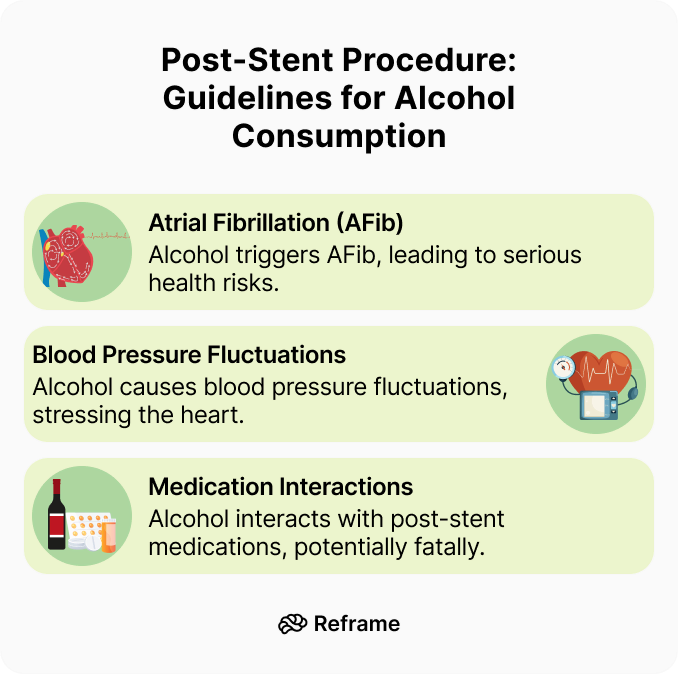
We’ve established that moderation is key, especially after a heart procedure. But what about binge drinking? This isn't just about having a few too many on a Saturday night; it’s about consuming a large amount of alcohol in a short time, which puts immense stress on your body — particularly your heart. For someone with a stent, this is especially risky. A sudden influx of alcohol can quickly raise your blood pressure and even trigger irregular heartbeats. This puts a dangerous strain on your newly repaired arteries, potentially counteracting the very benefits the stent was placed to provide. It also reminds us that any amount of alcohol carries some risk, and binge drinking significantly magnifies those dangers, especially when it comes to interacting with essential medications like blood thinners.
As we’ve reiterated throughout the article, we recommend speaking with your doctor about this before you go for a drink. Everyone’s recovery process is different, and we all react differently to medical procedures. Depending on overall health, a few drinks might not kill us, but drinking alcohol at this stage poses a lot of risks. Here are the big ones:
Let’s face it, if we’ve just had a stent placed, we probably have more than the average health considerations to take into account! We’re healing not only from the procedure, but we’re in the process of recovering from whatever condition led to the placement of the stent. To optimize heart and blood health and give our body the best chance at healing, it’s best to take it easy and avoid stressing our body out with alcohol.
The conversation around alcohol and heart health can feel confusing, with some studies suggesting benefits while others highlight major risks. It’s especially complicated after a procedure like a stent placement. Let's break down what some of the research indicates, but remember, these are general findings. Your personal health situation is unique, and your doctor's advice is always the most important guide for your recovery and long-term well-being. This is a time to be extra mindful about what you put into your body, and understanding the full picture can help you make the best choices for your healing process.
Interestingly, some research has explored the effects of alcohol on arteries after stenting. One study found that men who drank moderately had a lower chance of their arteries re-narrowing compared to those who drank very little. In that study, only 23% of moderate drinkers needed a repeat procedure, while 43% of very light drinkers did. The researchers suggested that moderate alcohol consumption might help prevent arteries from narrowing again after angioplasty. However, it's crucial to see this as a single data point and not a prescription to drink for your health. The risks associated with alcohol, especially during a fragile recovery period, can easily cancel out any potential, and still debated, benefits.
You may have also heard that alcohol can be good for your cholesterol. Some studies, particularly those looking at red wine, suggest that light to moderate drinking might help your heart by raising HDL, or "good" cholesterol. It’s thought that this could also help with inflammation in the body. While this is a common talking point, the potential benefits are often small and can be easily outweighed by the negative effects of alcohol, especially after a major heart event. You can get similar or better cholesterol-managing benefits from diet and exercise, without the added risks that come with drinking alcohol.
While the potential benefits we just discussed are debated, the risks are much more clear-cut. For many people, especially those with specific health factors, drinking alcohol after a stent isn't just a bad idea—it's dangerous. These aren't suggestions but firm guidelines for protecting your health and ensuring your recovery is successful. If any of the following situations apply to you, abstaining from alcohol is the safest and smartest choice you can make for your heart. This is where being honest with yourself and your medical team is absolutely essential for your long-term health and peace of mind.
Your overall health picture is the most important factor. You should not drink alcohol at all if you have conditions like liver problems or uncontrolled high blood pressure. Most importantly, you need to consider your medications. If you are taking blood thinners or other heart medications, alcohol can cause dangerous interactions, increasing bleeding risks or causing unpredictable changes in blood pressure. In fact, alcohol can interfere with all the drugs typically used after a stent placement. At high amounts, this interaction can be fatal. Always talk to your doctor about whether it's safe for you to drink. Your life could depend on it.
Seek medical attention or dial 911 if you experience any of these symptoms after a stent procedure:
Although the angioplasty and stent will help the blood circulate better, that doesn’t mean we’re completely off the hook! We still need to do our part to live a healthy lifestyle. That means eating healthy foods, exercising, avoiding tobacco products, and limiting alcohol.
Moderation is key to overall health and a healthy relationship with alcohol. We may have heard the term “moderation” thrown around a lot, but what does it actually mean?
Moderation means consuming alcoholic beverages in reasonable limits that mitigate risks to health. Moderation implies a balanced and controlled approach to drinking. It’s typically defined as less than one drink per day for women and fewer than two drinks per day for men.
Moderation entails making intentional and informed decisions about the quantity and frequency of our alcohol intake. Mindful drinking prioritizes our health goals and allows us to avoid negative consequences such as impaired judgment or dependency. To learn more about how mindful drinking benefits overall well-being, check out our article about health benefits of cutting back on drinking.
Luckily, life offers many options for enjoying ourselves without drinking alcohol. Let’s take a look at how we can protect our heart health with sobriety!
It’s easy to hear “one drink a day” and lose track of what that actually means. Is a pint of high-alcohol craft beer one drink? What about that generous pour of wine at dinner? In the US, a “standard” drink contains about 14 grams of pure alcohol. This typically looks like 12 ounces of regular beer (at 5% ABV), 5 ounces of wine (at 12% ABV), or 1.5 ounces of distilled spirits like vodka or whiskey (at 40% ABV). Understanding these measurements is the first step toward accurately tracking your intake and making sure your version of “one drink” aligns with medical guidelines. Knowing exactly how much you’re consuming can help you better understand its effect on your blood alcohol content and your heart.
If you choose to drink after a stent procedure, doing so with intention is crucial for protecting your heart. This is the core of mindful drinking — it’s about being present and making conscious choices rather than drinking out of habit. Before you pour a drink, ask yourself why you want it. Is it to relax, to celebrate, or just because it’s there? Consider opting for drinks that are lower in alcohol and sugar, as sugary cocktails and high-calorie beers can put additional stress on your body. The goal is to shift your relationship with alcohol from a reactive one to a proactive one, where your long-term health is always the priority.
One of the most effective strategies for safer drinking is to manage your pace and stay hydrated. A simple but powerful rule is to alternate every alcoholic beverage with a full glass of water. This practice does two important things: it prevents dehydration, which can strain your system, and it naturally slows down your rate of consumption. Giving your body more time to process the alcohol helps prevent sudden spikes in blood pressure, which is especially important when you’re protecting your heart. This simple habit makes it easier to stay within moderation and reinforces the benefits you gain on the days you choose not to drink at all.
Many of us have heard that a glass of red wine is good for heart health. So is that an invitation to drink our daily glass (and then some) if we’re on a path of healing our heart?
Think again! We wish it were that simple. Most of those studies have been debunked, or it was proven that we get all the benefits of drinking red wine by just drinking non-alcoholic grape juice (without the negative effects of alcohol).
Luckily, there are heart-healthy ways to enjoy a “drink” without alcohol. In fact, this time of healing can stand as the beginning of a greater journey toward sobriety or mindfully reduced drinking. Let’s look at some healthy alternatives to drinking alcohol after getting a stent placed.
Whether we’re recovering from heart surgery or taking a break from drinking for other health reasons, there are many benefits to an alcohol-free lifestyle worth exploring.
Although it’s not technically a “no-no” to drink alcohol after having a stent fitted, the best idea is to exercise caution with anything that could potentially put us at risk or cause any complications — especially when we’re dealing with matters of the heart! Our hearts are really the heartbeat of our entire well-being. As always, Reframe is here to help us all make positive changes that benefit our health.
A stent is a fantastic piece of medical technology, but it's important to remember that it doesn't cure the underlying coronary artery disease. It's a fix for a specific blockage, not a full-body reset. This means the risk of future heart problems, including another heart attack, is still there if lifestyle factors aren't addressed. This is especially true when it comes to alcohol. If you're focused on your heart health, it's generally best to limit or avoid alcohol, and this becomes even more critical after you've had a heart attack. Making conscious choices now is your best defense for the future.
You're probably eager to get back to your routine, and you will! The key is to follow your doctor's timeline. They will give you specific instructions on when you can drive, return to work, and tackle your usual chores. This isn't a time for guesswork or pushing yourself too hard. To protect your well-being, it’s essential to be completely honest and open with your doctor about how you're feeling and what you're capable of. They are your best resource for navigating this recovery phase safely. Your body has been through a lot, so give it the time it needs to heal properly.
Once you get the green light from your doctor, easing back into physical activity is a huge step toward long-term heart health. Start with gentle activities like walking. The goal isn't to run a marathon next week, but to slowly build back your strength and stamina. After your initial recovery, you'll be able to get back to being your normal self, but it will likely involve adjusting to a new lifestyle with healthier choices. Think of it as creating a new, stronger foundation for your health, where regular, enjoyable movement is a non-negotiable part of your day.
This is a common question that many people feel shy about asking, but it's a perfectly normal part of life and recovery. Most doctors advise that you can resume sexual activity when you feel ready—often when you can handle mild to moderate exercise, like climbing two flights of stairs, without getting breathless or having chest pain. Ultimately, we still need to do our part to live a healthy lifestyle. That means focusing on heart-healthy foods, getting regular exercise, avoiding tobacco, and limiting alcohol, all of which contribute to your overall stamina and well-being.
Planning a trip? Flying involves changes in air pressure and can be physically demanding (hello, lugging suitcases!), so it's wise to check with your doctor before booking a flight. They'll consider your specific situation, the length of the flight, and how your recovery is progressing. There's no one-size-fits-all answer, so it's crucial to speak to a healthcare provider about your individual case and medical history. They can give you the personalized advice you need to travel safely and with peace of mind.
Your doctor might recommend a cardiac rehabilitation program, and if they do, it's a fantastic opportunity. These programs are medically supervised and designed to help you recover safely while improving your overall cardiovascular health. They typically include structured exercise, education on heart-healthy living (like nutrition and stress management), and counseling to help you adjust. Think of it as having a dedicated team of experts guiding you through the process of building a stronger, healthier life after your stent procedure. It’s a proactive step that can make a huge difference in your long-term outcome.
This is non-negotiable. Your doctor will likely prescribe medications like blood thinners or cholesterol-lowering drugs to prevent new clots and keep your arteries open. It is absolutely critical to take these exactly as prescribed. This is also where alcohol can be particularly dangerous. Alcohol interacts with all the drugs typically used after a stent placement, which can lead to serious complications. Mixing them can alter how the medications work and put unnecessary strain on your body. Sticking to your medication plan is one of the most important things you can do for your heart.
A stent procedure is the beginning of a new chapter in your health journey, not the end of the story. Regular follow-up appointments with your doctor are essential to monitor your progress, check your blood pressure and cholesterol, and make any necessary adjustments to your treatment plan. These checkups are your chance to ask questions and stay on track. If you do choose to drink alcohol, these appointments are the time to discuss it with your doctor. The key takeaway is that if we choose to drink, it’s vital to practice moderation and ensure it aligns with your overall health plan.
What we eat has a direct impact on our heart. Adopting a heart-healthy diet, like the Mediterranean diet, is one of the best changes you can make. This means filling your plate with fruits, vegetables, whole grains, lean proteins (like fish and chicken), and healthy fats (like olive oil and avocados). It also means cutting back on processed foods, saturated fats, trans fats, and excess sodium. This isn't about deprivation; it's about nourishing your body with the fuel it needs to heal and thrive for years to come.
Emotional stress can take a physical toll on your heart by raising blood pressure and heart rate. Finding healthy ways to manage stress is a crucial part of your recovery. This could be through practices like meditation, deep breathing exercises, yoga, or simply spending time in nature. To give our body the best chance at healing, it’s best to take it easy and avoid stressing it out with things like alcohol, which can add both physical and emotional strain. Prioritizing relaxation isn't an indulgence—it's a core component of your heart care plan.
You don't have to go through this alone. Leaning on your support system is incredibly important for both your emotional and physical recovery. It’s important to have a support system in place, whether it’s family, friends, or your healthcare team. Talking about your experiences, fears, and successes can make a world of difference. For many, connecting with others who are on a similar journey to improve their health and change their relationship with alcohol can be empowering. The Reframe app, for example, offers a supportive community to help you build these healthy habits.
How soon after my stent procedure can I have a drink? There isn't a single, universal timeline for when it's safe to drink alcohol again. Your personal recovery depends on your overall health, the specifics of your procedure, and the medications you're taking. The first few weeks are a fragile healing period where your body needs to recover without the added stress of processing alcohol. The only person who can give you a definite answer is your doctor, who understands your complete medical picture.
What is the single biggest danger of drinking alcohol with a stent? The most critical risk is how alcohol interacts with your new medication regimen. After a stent, you'll likely be on essential drugs like blood thinners and cholesterol medication. Alcohol can interfere with how these drugs work, potentially increasing your risk of bleeding or causing unpredictable changes in your blood pressure. This interaction isn't just a minor issue; it can have very serious consequences for your heart health.
I've always heard red wine is good for the heart. Does that still apply after a stent? That old piece of advice gets complicated after a major heart event. While some studies have pointed to potential benefits from compounds in red wine, the risks associated with alcohol itself generally outweigh them, especially during recovery. You can get much more reliable heart-healthy benefits from things like a balanced diet and gentle exercise, without adding the strain that alcohol puts on your cardiovascular system.
My procedure was a while ago and I feel fine. Is it still risky to drink? It's great that you're feeling well, but it's important to remember that a stent treats a specific blockage, not the underlying condition of coronary artery disease. Alcohol can still contribute to risk factors like high blood pressure, weight gain, and irregular heart rhythms, which can lead to future problems. Thinking about your long-term heart health is just as important as getting through the initial recovery.
If my doctor and I agree that occasional drinking is okay, what's the safest way to do it? If you choose to drink, the key is to be mindful and intentional. This means knowing what a standard drink size is for your beverage of choice and sticking to strict moderation. A great strategy is to pace yourself by having a full glass of water between each alcoholic drink. This keeps you hydrated and naturally slows you down. The goal is to make a conscious choice that supports your health, not to fall back into old habits.

Learn how to detox your body from alcohol with these 7 tasty liver detox drinks, and find out how to optimize your liver health!
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually, with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet millions of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
Last night was wild, and now you’re feeling crummy. Maybe it’s a hangover, or flashes from embarrassing moments. At times like these, we often have some clarity about our self-care. We may decide to counteract our overindulgence with a healthy boost to the system — a trip to the gym, a green smoothie for breakfast, or a commitment to take it a little easier next time.

One great way to get a health boost after heavy drinking is to give our liver a break. Indulging in a healthy liver detox drink is like giving a spa day to the hardworking organ that cleans up the alcohol from our system and gets us back to our sober selves.
If you’re wondering what to drink to detox your body, looking for liver flush recipes, or searching for homemade detox drink ideas, you’ve come to the right place. What is a good detox drink to flush your system? And what are the best detox drinks for alcohol recovery? Read on for tips and recipes!
Now that you have some ideas of how to experiment with your own recipes, let’s look at a few to get you started and inspire you. Here are seven tasty recipes to set you on the road to recovery.
1 cup of water
½ inch piece of ginger, grated or sliced
Juice from half a lemon
1 tsp of honey (or to taste)
Optional: cinnamon stick, fresh mint leaves, or turmeric
Boil the water and add all ingredients. Steep for 5-10 minutes, then strain. This drink is soothing when hot, and refreshing when served over ice.
Psychotherapy is beneficial for AUD treatment because it addresses our mental health. Our mental health and AUD are connected in three main ways:
Blend all the ingredients together well and serve while still warm.

1 bananas (fresh or frozen without the skin)
1 cup of milk of your choice
¼ cup peanut butter
Optional: 1 tablespoons honey, or to taste
1 cup of ice cubes
Blend everything together very well and enjoy. It’s that simple!
1 cup leafy greens (spinach, kale, and chard are great!)
½ - 1 banana
½ avocado
½ cup orange juice, plus more to taste
½ teaspoon chia seeds and/or hemp hearts
1 cup almond milk, plus more as needed to blend
Handful of ice
Toss everything into a blender and enjoy! You might also consider adding ingredients like spirulina, flaxseed meal, and frozen fruits (try pineapple or mango!).
⅓ cup peeled + chopped raw beet (or ¼ cup beet juice)
1 ⅓ cup frozen strawberries
½ frozen banana
⅔ cup apple juice or cider
A handful of ice (more if using fresh fruit)
Blend everything together. Want to get experimental? Try adding a tablespoon of almond or sunflower seed butter for some extra creaminess, or a carrot for an extra nutritional boost.
If you have access to fresh dandelion root — amazing! It can be hard to find, so here are some suggestions for spicing up your plain store-bought dandelion tea. Experiment and find what works for you! Don’t go too crazy: try one or two of these things at a time to get an idea of what you do or don’t like.
Milk or cream of your choice
1 cinnamon stick
½ teaspoon of dried ginger
1 teaspoon fresh minced ginger
⅛ tsp vanilla extract (or to taste)
1 tsp honey or maple syrup (or to taste)
⅛ tsp pumpkin spice
⅛ tsp cloves
1 large orange, peeled
½ banana (fresh or frozen)
1 cup frozen mango chunks
½ cup milk of your choice
¼ cup vanilla extract
Blend everything together very well. Consider adding a carrot for an extra nutrient boost and a glowing orange color.
The liver is one of the largest organs in the human body, an essential player on the organ team that keeps our body running. Understanding what it does is a good place to start when thinking about how to take care of it.
A detox can help us keep our liver in tip-top shape.
Wondering what to drink to detox your body? The best detox cleanse drink for your liver is the one you’ll drink and enjoy! When you understand the ingredients that go into good detox drinks, you can start crafting one to your tastes.
When it comes to the mixology of liver detox drinks, there are two major categories to explore: teas and smoothies.
Teas allow us to take advantage of the many herbs and plants that boost liver health. You can make hot tea on a cold winter day or a cozy evening, or an iced tea to beat the heat in the dead of summer. Whichever you choose, there are a few key items to keep in your pantry.
Who doesn’t love a tasty smoothie? They’re an easy, refreshing way to blend up superfoods and pack a wellness punch. Let’s look at some great smoothie ingredients to inspire you:
Next time you’re enjoying your morning cup of joe, consider that it’s doing more for you than just giving you an energy boost. Coffee is known to help protect against liver cancer. Don’t think that’s a license to up your intake — the caffeine in coffee can interfere with sleep and cause gastrointestinal issues, and excessive coffee intake is associated with a higher risk of other types of cancer.
Hopefully these liver-detoxing ingredients have you excited and inspired. But before you run to the kitchen to concoct some cleansing drinks, let’s consider one more thing.
If you’re in a rush to detox, you may be out of luck. If you’re wondering how to get alcohol out of your system fast, a detox drink simply won’t do it. There’s no way to speed up the elimination of alcohol from your system. Your liver can only process alcohol so quickly, and it needs time and rest to do its job.
So what is the best drink to flush your liver. Water! Good old H2O is the antidote to alcohol’s dehydrating effects. To give your liver a chance to focus on its job, drink some water, get in a good veggie-filled meal, and have a restful day.
While these recipes are a great way to recover, the best way to protect your liver is to control your alcohol intake by quitting or cutting back on drinking. Let’s look at some tips to help you make a successful rebound on your liver recovery journey.
Last night was wild, and now you’re feeling crummy. Maybe it’s a hangover, or flashes from embarrassing moments. At times like these, we often have some clarity about our self-care. We may decide to counteract our overindulgence with a healthy boost to the system — a trip to the gym, a green smoothie for breakfast, or a commitment to take it a little easier next time.

One great way to get a health boost after heavy drinking is to give our liver a break. Indulging in a healthy liver detox drink is like giving a spa day to the hardworking organ that cleans up the alcohol from our system and gets us back to our sober selves.
If you’re wondering what to drink to detox your body, looking for liver flush recipes, or searching for homemade detox drink ideas, you’ve come to the right place. What is a good detox drink to flush your system? And what are the best detox drinks for alcohol recovery? Read on for tips and recipes!
Now that you have some ideas of how to experiment with your own recipes, let’s look at a few to get you started and inspire you. Here are seven tasty recipes to set you on the road to recovery.
1 cup of water
½ inch piece of ginger, grated or sliced
Juice from half a lemon
1 tsp of honey (or to taste)
Optional: cinnamon stick, fresh mint leaves, or turmeric
Boil the water and add all ingredients. Steep for 5-10 minutes, then strain. This drink is soothing when hot, and refreshing when served over ice.
Psychotherapy is beneficial for AUD treatment because it addresses our mental health. Our mental health and AUD are connected in three main ways:
Blend all the ingredients together well and serve while still warm.

1 bananas (fresh or frozen without the skin)
1 cup of milk of your choice
¼ cup peanut butter
Optional: 1 tablespoons honey, or to taste
1 cup of ice cubes
Blend everything together very well and enjoy. It’s that simple!
1 cup leafy greens (spinach, kale, and chard are great!)
½ - 1 banana
½ avocado
½ cup orange juice, plus more to taste
½ teaspoon chia seeds and/or hemp hearts
1 cup almond milk, plus more as needed to blend
Handful of ice
Toss everything into a blender and enjoy! You might also consider adding ingredients like spirulina, flaxseed meal, and frozen fruits (try pineapple or mango!).
⅓ cup peeled + chopped raw beet (or ¼ cup beet juice)
1 ⅓ cup frozen strawberries
½ frozen banana
⅔ cup apple juice or cider
A handful of ice (more if using fresh fruit)
Blend everything together. Want to get experimental? Try adding a tablespoon of almond or sunflower seed butter for some extra creaminess, or a carrot for an extra nutritional boost.
If you have access to fresh dandelion root — amazing! It can be hard to find, so here are some suggestions for spicing up your plain store-bought dandelion tea. Experiment and find what works for you! Don’t go too crazy: try one or two of these things at a time to get an idea of what you do or don’t like.
Milk or cream of your choice
1 cinnamon stick
½ teaspoon of dried ginger
1 teaspoon fresh minced ginger
⅛ tsp vanilla extract (or to taste)
1 tsp honey or maple syrup (or to taste)
⅛ tsp pumpkin spice
⅛ tsp cloves
1 large orange, peeled
½ banana (fresh or frozen)
1 cup frozen mango chunks
½ cup milk of your choice
¼ cup vanilla extract
Blend everything together very well. Consider adding a carrot for an extra nutrient boost and a glowing orange color.
The liver is one of the largest organs in the human body, an essential player on the organ team that keeps our body running. Understanding what it does is a good place to start when thinking about how to take care of it.
A detox can help us keep our liver in tip-top shape.
Wondering what to drink to detox your body? The best detox cleanse drink for your liver is the one you’ll drink and enjoy! When you understand the ingredients that go into good detox drinks, you can start crafting one to your tastes.
When it comes to the mixology of liver detox drinks, there are two major categories to explore: teas and smoothies.
Teas allow us to take advantage of the many herbs and plants that boost liver health. You can make hot tea on a cold winter day or a cozy evening, or an iced tea to beat the heat in the dead of summer. Whichever you choose, there are a few key items to keep in your pantry.
Who doesn’t love a tasty smoothie? They’re an easy, refreshing way to blend up superfoods and pack a wellness punch. Let’s look at some great smoothie ingredients to inspire you:
Next time you’re enjoying your morning cup of joe, consider that it’s doing more for you than just giving you an energy boost. Coffee is known to help protect against liver cancer. Don’t think that’s a license to up your intake — the caffeine in coffee can interfere with sleep and cause gastrointestinal issues, and excessive coffee intake is associated with a higher risk of other types of cancer.
Hopefully these liver-detoxing ingredients have you excited and inspired. But before you run to the kitchen to concoct some cleansing drinks, let’s consider one more thing.
If you’re in a rush to detox, you may be out of luck. If you’re wondering how to get alcohol out of your system fast, a detox drink simply won’t do it. There’s no way to speed up the elimination of alcohol from your system. Your liver can only process alcohol so quickly, and it needs time and rest to do its job.
So what is the best drink to flush your liver. Water! Good old H2O is the antidote to alcohol’s dehydrating effects. To give your liver a chance to focus on its job, drink some water, get in a good veggie-filled meal, and have a restful day.
While these recipes are a great way to recover, the best way to protect your liver is to control your alcohol intake by quitting or cutting back on drinking. Let’s look at some tips to help you make a successful rebound on your liver recovery journey.

Many alcoholic drinks are loaded with sugar, which is detrimental to our overall well-being. Learn which beverages contain the most sugar and discover low-sugar alternative options.
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually, with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet millions of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
You’ve been slowly making changes to your lifestyle, and you’re finally tackling one area in particular: your sugar intake. You’ve removed the Oreos from your pantry, traded your morning donut for a bowl of oatmeal, and swapped your afternoon chocolate bar for a handful of nuts. But there’s still one lingering issue — your alcohol intake.
You have a cocktail or a glass of wine several times throughout the week. But have you ever paused to consider what's inside these beverages beyond the alcohol? The sugar content in alcoholic drinks is often overlooked, yet it can impact our health.
First let’s start by discussing the basic chemistry of alcoholic beverages. Pure alcohol, chemically known as ethanol, does not contain any sugar. Ethanol is produced through the fermentation process, during which yeast consumes sugars found in fruits, grains, or vegetables and converts them into alcohol and carbon dioxide.
The key factor in determining alcoholic beverages’ sugar content lies in the specifics of this fermentation process and the liquid’s subsequent treatments. For example, in wine production, the natural sugars in grapes are partially or fully fermented into alcohol, depending on the desired sweetness of the wine. Dry wines undergo a longer fermentation process, resulting in lower residual sugar; sweeter wines retain more of the original sugars.
In the case of distilled spirits such as vodka and whiskey, the initial fermentation creates a mash that contains alcohol and sugars. The distillation process then heats this mixture, evaporating the alcohol (which has a lower boiling point) and leaving most other substances, including sugars, behind. Consequently, most straight distilled spirits contain negligible sugar.
However, post-distillation treatments and flavor additions can alter this natural state. Liqueurs, flavored spirits, and pre-mixed drinks often have sugars and other sweeteners added to enhance taste, contributing to their overall sugar content.
Thus, while pure alcohol itself is sugar-free, the final sugar content in alcoholic beverages varies significantly based on the type of drink, the fermentation process, and any additional flavorings or mixers. Understanding these factors is essential for those of us looking to manage our sugar intake while still enjoying alcoholic beverages.
Vodka, a popular distilled spirit, is known for its clarity and supposed purity. This perception stems from its production process, which involves the fermentation of grains like wheat, rye, or potatoes, followed by a thorough distillation. The distillation process effectively removes impurities and residual sugars from the fermented mixture, resulting in a beverage that’s almost exclusively composed of water and ethanol (alcohol). This is why traditional, unflavored vodka is often considered sugar-free.
The caloric content in unflavored vodka comes primarily from its alcohol content. Alcohol contains about 7 calories per gram, which is almost twice as caloric as carbohydrates (including sugars) but less caloric than fats. While vodka does not contribute sugar to our diet, it does contribute calories — an important consideration for those of us watching our overall caloric intake.
Flavored vodkas are a different story. These contain sugars and other sweetening agents to enhance their taste and appeal. The sugar content in flavored vodkas varies widely depending on the brand and the specific flavoring methods. Some flavored vodkas contain 2-11 grams of sugar per 1.5-ounce serving. This can quickly add up, especially when consumed quickly in the form of shots.
Gin, similar to vodka, is typically sugar-free post-distillation, as the sugars in the original mash are converted into alcohol. The distillation process renders gin’s sugar content negligible — the final product is primarily alcohol and water.
However, the classic gin and tonic cocktail introduces a great deal of sugar, not from the gin itself, but from the tonic water. Tonic water, often perceived as a simple mixer, actually contains a considerable amount of sugar to balance the bitterness of quinine, its key ingredient. A single serving of tonic water can add up to 18 grams of sugar to a drink.
Beer contains sugars due to its brewing process. Brewed from starch-rich ingredients such as barley, the sugars in these grains are essential for fermentation, during which yeast converts them into alcohol and carbon dioxide. However, not all the sugars are fermented; some remain in the final product, contributing to the beer's flavor and body.
The sugar content in beer varies, but a standard pint typically contains up to 3 grams of sugar. This amount can increase, particularly in darker beers. Darker beers often have a richer malt profile, which involves the use of more heavily roasted grains. These grains contribute not only to the beer's deeper color and robust flavor but also to a higher residual sugar content.
Therefore, the sugar content of beer greatly depends upon its type, with darker varieties generally having more sugar compared to lighter ones.
The sugar content in wine varies greatly depending on the type and style of wine. It ranges from almost zero in some dry wines to high levels in sweet dessert wines.
In dry wines, most of the natural sugars from grapes are fermented into alcohol, leaving less than 1 gram of sugar per glass. Medium-dry wines might contain 1 to 12 grams of sugar per serving. On the other hand, sweet wines, such as some rieslings or dessert wines like port, can have over 20 grams of sugar per serving.
The winemaking process plays a crucial role in this variation; winemakers can stop fermentation early to retain more natural sugar for a sweeter taste or allow it to continue longer for a drier wine. It’s essential for those of us monitoring our sugar intake to understand the distinction between dry, medium, and sweet wines, as is checking the label for residual sugar content where available.

Tequila, a distinctive spirit distilled from the agave plant, typically contains almost no sugar. The production process involves harvesting the agave, extracting the juice, and then fermenting it. During fermentation, the natural sugars in the agave are converted into alcohol. The subsequent distillation process further purifies the liquid, leaving behind most non-alcoholic components, including sugars.
As a result, pure tequila, particularly the clear varieties such as blanco or silver tequila, is generally considered sugar-free. However, aged tequilas, such as reposado or añejo, may have trace amounts of sugar due to the caramelization of natural sugars during the aging process in wooden barrels. It's also noteworthy that flavored or mixed tequilas can contain added sugars, significantly altering their sugar content compared to traditional, pure tequila.
While tequila may have little to no sugar, it still contains a significant amount of alcohol. Consumption should be monitored to avoid the adverse effects of intoxication.
Whiskey, a spirit distilled from fermented grain mash, including barley, corn, rye, and wheat, typically has no sugar after the distillation process. The sugars present in the grains are crucial for fermentation, a process through which they’re converted into alcohol. During distillation, the alcohol is separated from most other components, including sugars, resulting in a sugar-free final product.
This holds true for various types of whiskey, such as scotch, bourbon, and rye. However, it's important to distinguish between straight whiskey and whiskey-based liqueurs or flavored whiskeys. The latter often contain added sugars and other flavoring agents, which can significantly increase their sugar content.
Like tequila, it’s important to drink whiskey in moderation to avoid the downsides of its high alcohol content.
Cocktails are notorious for their high sugar content. The sugar content in these beverages can significantly vary based on their ingredients:
Sugar, unfortunately, is present in many of our foods and beverages today. Many of us far exceed the recommended 24 grams (for women) or 36 grams (for men) of added sugar per day.
Consuming excessive amounts of sugar poses several health risks:
As with alcohol, moderating our sugar intake is key. Understanding the sugar content in alcoholic beverages is crucial for maintaining good health and preventing these potential risks.
When we build healthier drinking habits, we can also lower our overall sugar intake. Here’s how we can simultaneously lower our sugar and alcohol consumption:
Sugar sneaks into many of our food and beverages, and alcohol is no exception. Awareness of the sugar content in alcoholic beverages is a crucial step in making informed health decisions. With this knowledge, we can enjoy our evenings responsibly, knowing we're taking care of our bodies in the process.
The changes we make today will have lasting effects on our well-being. And with better health, we can be more present for what truly matters in our lives.
You’ve been slowly making changes to your lifestyle, and you’re finally tackling one area in particular: your sugar intake. You’ve removed the Oreos from your pantry, traded your morning donut for a bowl of oatmeal, and swapped your afternoon chocolate bar for a handful of nuts. But there’s still one lingering issue — your alcohol intake.
You have a cocktail or a glass of wine several times throughout the week. But have you ever paused to consider what's inside these beverages beyond the alcohol? The sugar content in alcoholic drinks is often overlooked, yet it can impact our health.
First let’s start by discussing the basic chemistry of alcoholic beverages. Pure alcohol, chemically known as ethanol, does not contain any sugar. Ethanol is produced through the fermentation process, during which yeast consumes sugars found in fruits, grains, or vegetables and converts them into alcohol and carbon dioxide.
The key factor in determining alcoholic beverages’ sugar content lies in the specifics of this fermentation process and the liquid’s subsequent treatments. For example, in wine production, the natural sugars in grapes are partially or fully fermented into alcohol, depending on the desired sweetness of the wine. Dry wines undergo a longer fermentation process, resulting in lower residual sugar; sweeter wines retain more of the original sugars.
In the case of distilled spirits such as vodka and whiskey, the initial fermentation creates a mash that contains alcohol and sugars. The distillation process then heats this mixture, evaporating the alcohol (which has a lower boiling point) and leaving most other substances, including sugars, behind. Consequently, most straight distilled spirits contain negligible sugar.
However, post-distillation treatments and flavor additions can alter this natural state. Liqueurs, flavored spirits, and pre-mixed drinks often have sugars and other sweeteners added to enhance taste, contributing to their overall sugar content.
Thus, while pure alcohol itself is sugar-free, the final sugar content in alcoholic beverages varies significantly based on the type of drink, the fermentation process, and any additional flavorings or mixers. Understanding these factors is essential for those of us looking to manage our sugar intake while still enjoying alcoholic beverages.
Vodka, a popular distilled spirit, is known for its clarity and supposed purity. This perception stems from its production process, which involves the fermentation of grains like wheat, rye, or potatoes, followed by a thorough distillation. The distillation process effectively removes impurities and residual sugars from the fermented mixture, resulting in a beverage that’s almost exclusively composed of water and ethanol (alcohol). This is why traditional, unflavored vodka is often considered sugar-free.
The caloric content in unflavored vodka comes primarily from its alcohol content. Alcohol contains about 7 calories per gram, which is almost twice as caloric as carbohydrates (including sugars) but less caloric than fats. While vodka does not contribute sugar to our diet, it does contribute calories — an important consideration for those of us watching our overall caloric intake.
Flavored vodkas are a different story. These contain sugars and other sweetening agents to enhance their taste and appeal. The sugar content in flavored vodkas varies widely depending on the brand and the specific flavoring methods. Some flavored vodkas contain 2-11 grams of sugar per 1.5-ounce serving. This can quickly add up, especially when consumed quickly in the form of shots.
Gin, similar to vodka, is typically sugar-free post-distillation, as the sugars in the original mash are converted into alcohol. The distillation process renders gin’s sugar content negligible — the final product is primarily alcohol and water.
However, the classic gin and tonic cocktail introduces a great deal of sugar, not from the gin itself, but from the tonic water. Tonic water, often perceived as a simple mixer, actually contains a considerable amount of sugar to balance the bitterness of quinine, its key ingredient. A single serving of tonic water can add up to 18 grams of sugar to a drink.
Beer contains sugars due to its brewing process. Brewed from starch-rich ingredients such as barley, the sugars in these grains are essential for fermentation, during which yeast converts them into alcohol and carbon dioxide. However, not all the sugars are fermented; some remain in the final product, contributing to the beer's flavor and body.
The sugar content in beer varies, but a standard pint typically contains up to 3 grams of sugar. This amount can increase, particularly in darker beers. Darker beers often have a richer malt profile, which involves the use of more heavily roasted grains. These grains contribute not only to the beer's deeper color and robust flavor but also to a higher residual sugar content.
Therefore, the sugar content of beer greatly depends upon its type, with darker varieties generally having more sugar compared to lighter ones.
The sugar content in wine varies greatly depending on the type and style of wine. It ranges from almost zero in some dry wines to high levels in sweet dessert wines.
In dry wines, most of the natural sugars from grapes are fermented into alcohol, leaving less than 1 gram of sugar per glass. Medium-dry wines might contain 1 to 12 grams of sugar per serving. On the other hand, sweet wines, such as some rieslings or dessert wines like port, can have over 20 grams of sugar per serving.
The winemaking process plays a crucial role in this variation; winemakers can stop fermentation early to retain more natural sugar for a sweeter taste or allow it to continue longer for a drier wine. It’s essential for those of us monitoring our sugar intake to understand the distinction between dry, medium, and sweet wines, as is checking the label for residual sugar content where available.

Tequila, a distinctive spirit distilled from the agave plant, typically contains almost no sugar. The production process involves harvesting the agave, extracting the juice, and then fermenting it. During fermentation, the natural sugars in the agave are converted into alcohol. The subsequent distillation process further purifies the liquid, leaving behind most non-alcoholic components, including sugars.
As a result, pure tequila, particularly the clear varieties such as blanco or silver tequila, is generally considered sugar-free. However, aged tequilas, such as reposado or añejo, may have trace amounts of sugar due to the caramelization of natural sugars during the aging process in wooden barrels. It's also noteworthy that flavored or mixed tequilas can contain added sugars, significantly altering their sugar content compared to traditional, pure tequila.
While tequila may have little to no sugar, it still contains a significant amount of alcohol. Consumption should be monitored to avoid the adverse effects of intoxication.
Whiskey, a spirit distilled from fermented grain mash, including barley, corn, rye, and wheat, typically has no sugar after the distillation process. The sugars present in the grains are crucial for fermentation, a process through which they’re converted into alcohol. During distillation, the alcohol is separated from most other components, including sugars, resulting in a sugar-free final product.
This holds true for various types of whiskey, such as scotch, bourbon, and rye. However, it's important to distinguish between straight whiskey and whiskey-based liqueurs or flavored whiskeys. The latter often contain added sugars and other flavoring agents, which can significantly increase their sugar content.
Like tequila, it’s important to drink whiskey in moderation to avoid the downsides of its high alcohol content.
Cocktails are notorious for their high sugar content. The sugar content in these beverages can significantly vary based on their ingredients:
Sugar, unfortunately, is present in many of our foods and beverages today. Many of us far exceed the recommended 24 grams (for women) or 36 grams (for men) of added sugar per day.
Consuming excessive amounts of sugar poses several health risks:
As with alcohol, moderating our sugar intake is key. Understanding the sugar content in alcoholic beverages is crucial for maintaining good health and preventing these potential risks.
When we build healthier drinking habits, we can also lower our overall sugar intake. Here’s how we can simultaneously lower our sugar and alcohol consumption:
Sugar sneaks into many of our food and beverages, and alcohol is no exception. Awareness of the sugar content in alcoholic beverages is a crucial step in making informed health decisions. With this knowledge, we can enjoy our evenings responsibly, knowing we're taking care of our bodies in the process.
The changes we make today will have lasting effects on our well-being. And with better health, we can be more present for what truly matters in our lives.

Is there any truth to the adages that warn against mixing drinks, such as “Beer before liquor, you’ve never been sicker”? Learn about the real problem with mixing different types of alcohol.
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually, with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet millions of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
You’re meeting some friends for happy hour after work. You order a beer, gulp it down, and are ready for another drink. You’re thinking about ordering a vodka soda, but your friend urges you to reconsider, saying, “Beer before liquor, never sicker.” You shrug it off. This isn’t the first time you’ve heard a saying like this. You’ve also been told, “Liquor before beer, you’re in the clear” and “Beer before wine, and you’ll feel fine.”
But is the “beer before liquor” rule really true? Can you mix beer and wine? Or does mixing alcohol somehow make it stronger? And what about mixing liquors? In this post, we explore the dangers of mixing different types of alcohol and provide tips on how to better manage our alcohol consumption. Let’s dive in!

Many people assume that mixing drinks increases the risk of getting sick or makes our hangovers worse (hence all those rhyming warnings). But this actually isn’t true. Drinking a beer and then a gin and tonic will probably have the same effect on our body as sticking to one type of alcoholic beverage.
When it comes to drinking alcohol, experts agree that there are only two things that increase our likelihood of getting sick or experiencing a hangover. Let’s take a closer look:
So, why is mixing alcohol bad? The problem with mixing drinks comes down to the rate at which our body processes alcohol. When we take a sip of alcohol — whether beer, wine, or liquor — it’s quickly absorbed into our bloodstream through our stomach lining and small intestine.
Once in our blood, alcohol is rapidly transported throughout our entire body, which is why it affects so many different bodily systems. Depending on how quickly our body’s tissues absorb alcohol, we’ll typically feel its effect within 15 to 45 minutes.
Most alcohol that enters our body eventually ends up in the liver, which is responsible for metabolizing it, or breaking it down. Our liver can only efficiently process one standard-sized alcoholic drink per hour. In other words, it takes 1 hour for our body to metabolize just one beer, one glass of wine, or one shot.
The amount of alcohol in our blood rises more quickly after drinking liquor than beer, due to its higher concentration of alcohol. If we drink liquor before beer, we’re likely to feel the effects of alcohol sooner. This might encourage us not to consume as much, thereby decreasing our chance of getting sick. However, drinking beer before liquor may lead to us becoming ill since our lowered inhibitions and impaired decision making may motivate us to consume higher concentrations of alcohol by doing shots or mixing stronger drinks.
We can also think about it like this: if we drink beer and then liquor, we’ll most likely get more drunk than we would if we had started with liquor and felt the effects of alcohol earlier. If we end up getting sick, we may assume that the culprit was mixing the two types of alcohol in that order. In reality, the total amount of alcohol consumed in a short period of time caused us to become sick.
Furthermore, another problem with mixing drinks is that it makes it harder to track how much alcohol we’ve been consuming. For instance, it’s much easier to keep track of how many drinks we’ve consumed if we stick with one type of alcohol — such as beer or wine. If we’re bouncing around between cocktails, wine, beer, and shots, we’re likely to lose track pretty quickly. And when we’re not keeping track, we’re more likely to drink too much — which can cause us to get sick.
There aren’t necessarily any side effects specifically related to mixing alcohol. In fact, one study looked at whether drinking wine before beer was associated with hangover severity and found that the order of alcoholic beverages didn’t have a significant effect.
However, certain types of alcohol may be more likely to lead to a hangover than others. This is because different types of alcohol have different congeners — toxins that result from the fermentation process. Congeners put extra stress on our liver to break down these substances and restore normal body function.
Congeners also contribute to alcohol’s color and flavor. Darker alcohols (such as brandy, bourbon, whiskey, tequila, darker beer, and red wine) have more congeners than clear or lighter alcohols like vodka, gin, and lighter beers. Bourbon whisky, for example, contains 37 times the quantity of congeners as vodka!
If we mix different kinds of alcohol, we may unknowingly drink higher amounts of congeners, which may lead to a more intense hangover, nausea, or dizziness the next day. Experts agree that feeling sick while intoxicated or experiencing a hangover is due largely to the amount of alcohol consumed and the time period it’s consumed over.

Research suggests that hangovers are primarily caused by alcohol’s toxicity and dehydrating effects. Let’s take a closer look:
Furthermore, there’s evidence that alcohol disrupts our immune system, which could also contribute to the symptoms of a headache, nausea, and fatigue.
Several other factors play a role in how our body processes and tolerates alcohol. For instance, our sex might factor into hangover severity. One study found that women who had moderate to high estimated peak blood alcohol concentration (BAC) — 0.08 percent to more than 0.2 percent — reported hangovers with more severe nausea, tiredness, weakness and dizziness than men. This could be because women process alcohol differently from men: they tend to have less acetaldehyde dehydrogenase (ALDH), an important enzyme for metabolizing alcohol in the stomach.
Similarly, our age and weight also play a role. For instance, the older we are, the longer alcohol stays in our liver before it moves into our general bloodstream or is metabolized. Typically, older people have lower percentages of body water compared to those who are younger, which can also contribute to a higher blood alcohol content (BAC) and a slower processing time.
Many people don’t realize that mixing alcohol with medications can be much more dangerous than mixing different types of alcohol together. Alcohol is known to interact with a wide variety of prescription and over-the-counter medications such as the following:
Mixing alcohol with these substances can lead to a higher risk of liver damage, irregular heart rate, heart attacks, overdose, and enhanced side effects from the medication.
We won’t have to worry about getting sick from alcohol if we avoid it entirely or consume it in moderation. Mindful drinking can be particularly effective at helping us make more intentional choices. Here are some other tips for managing our alcohol consumption:
Mixing different types of alcoholic drinks doesn’t increase our risk of getting sick or having a hangover. It’s the quantity of alcohol consumed — not combined — and the rate at which we’re consuming it that influences intoxication and sickness. In other words, the problem with mixing beer and wine is that it usually leads to higher amounts of alcohol consumed more quickly in one sitting. This puts us in danger of intoxication and feeling hungover the next day.
If you’re struggling to manage your alcohol consumption, consider trying Reframe. We’re a science-backed app that has helped millions of people cut back on their alcohol consumption and enhance their physical, mental, and emotional well-being.
You’re meeting some friends for happy hour after work. You order a beer, gulp it down, and are ready for another drink. You’re thinking about ordering a vodka soda, but your friend urges you to reconsider, saying, “Beer before liquor, never sicker.” You shrug it off. This isn’t the first time you’ve heard a saying like this. You’ve also been told, “Liquor before beer, you’re in the clear” and “Beer before wine, and you’ll feel fine.”
But is the “beer before liquor” rule really true? Can you mix beer and wine? Or does mixing alcohol somehow make it stronger? And what about mixing liquors? In this post, we explore the dangers of mixing different types of alcohol and provide tips on how to better manage our alcohol consumption. Let’s dive in!

Many people assume that mixing drinks increases the risk of getting sick or makes our hangovers worse (hence all those rhyming warnings). But this actually isn’t true. Drinking a beer and then a gin and tonic will probably have the same effect on our body as sticking to one type of alcoholic beverage.
When it comes to drinking alcohol, experts agree that there are only two things that increase our likelihood of getting sick or experiencing a hangover. Let’s take a closer look:
So, why is mixing alcohol bad? The problem with mixing drinks comes down to the rate at which our body processes alcohol. When we take a sip of alcohol — whether beer, wine, or liquor — it’s quickly absorbed into our bloodstream through our stomach lining and small intestine.
Once in our blood, alcohol is rapidly transported throughout our entire body, which is why it affects so many different bodily systems. Depending on how quickly our body’s tissues absorb alcohol, we’ll typically feel its effect within 15 to 45 minutes.
Most alcohol that enters our body eventually ends up in the liver, which is responsible for metabolizing it, or breaking it down. Our liver can only efficiently process one standard-sized alcoholic drink per hour. In other words, it takes 1 hour for our body to metabolize just one beer, one glass of wine, or one shot.
The amount of alcohol in our blood rises more quickly after drinking liquor than beer, due to its higher concentration of alcohol. If we drink liquor before beer, we’re likely to feel the effects of alcohol sooner. This might encourage us not to consume as much, thereby decreasing our chance of getting sick. However, drinking beer before liquor may lead to us becoming ill since our lowered inhibitions and impaired decision making may motivate us to consume higher concentrations of alcohol by doing shots or mixing stronger drinks.
We can also think about it like this: if we drink beer and then liquor, we’ll most likely get more drunk than we would if we had started with liquor and felt the effects of alcohol earlier. If we end up getting sick, we may assume that the culprit was mixing the two types of alcohol in that order. In reality, the total amount of alcohol consumed in a short period of time caused us to become sick.
Furthermore, another problem with mixing drinks is that it makes it harder to track how much alcohol we’ve been consuming. For instance, it’s much easier to keep track of how many drinks we’ve consumed if we stick with one type of alcohol — such as beer or wine. If we’re bouncing around between cocktails, wine, beer, and shots, we’re likely to lose track pretty quickly. And when we’re not keeping track, we’re more likely to drink too much — which can cause us to get sick.
There aren’t necessarily any side effects specifically related to mixing alcohol. In fact, one study looked at whether drinking wine before beer was associated with hangover severity and found that the order of alcoholic beverages didn’t have a significant effect.
However, certain types of alcohol may be more likely to lead to a hangover than others. This is because different types of alcohol have different congeners — toxins that result from the fermentation process. Congeners put extra stress on our liver to break down these substances and restore normal body function.
Congeners also contribute to alcohol’s color and flavor. Darker alcohols (such as brandy, bourbon, whiskey, tequila, darker beer, and red wine) have more congeners than clear or lighter alcohols like vodka, gin, and lighter beers. Bourbon whisky, for example, contains 37 times the quantity of congeners as vodka!
If we mix different kinds of alcohol, we may unknowingly drink higher amounts of congeners, which may lead to a more intense hangover, nausea, or dizziness the next day. Experts agree that feeling sick while intoxicated or experiencing a hangover is due largely to the amount of alcohol consumed and the time period it’s consumed over.

Research suggests that hangovers are primarily caused by alcohol’s toxicity and dehydrating effects. Let’s take a closer look:
Furthermore, there’s evidence that alcohol disrupts our immune system, which could also contribute to the symptoms of a headache, nausea, and fatigue.
Several other factors play a role in how our body processes and tolerates alcohol. For instance, our sex might factor into hangover severity. One study found that women who had moderate to high estimated peak blood alcohol concentration (BAC) — 0.08 percent to more than 0.2 percent — reported hangovers with more severe nausea, tiredness, weakness and dizziness than men. This could be because women process alcohol differently from men: they tend to have less acetaldehyde dehydrogenase (ALDH), an important enzyme for metabolizing alcohol in the stomach.
Similarly, our age and weight also play a role. For instance, the older we are, the longer alcohol stays in our liver before it moves into our general bloodstream or is metabolized. Typically, older people have lower percentages of body water compared to those who are younger, which can also contribute to a higher blood alcohol content (BAC) and a slower processing time.
Many people don’t realize that mixing alcohol with medications can be much more dangerous than mixing different types of alcohol together. Alcohol is known to interact with a wide variety of prescription and over-the-counter medications such as the following:
Mixing alcohol with these substances can lead to a higher risk of liver damage, irregular heart rate, heart attacks, overdose, and enhanced side effects from the medication.
We won’t have to worry about getting sick from alcohol if we avoid it entirely or consume it in moderation. Mindful drinking can be particularly effective at helping us make more intentional choices. Here are some other tips for managing our alcohol consumption:
Mixing different types of alcoholic drinks doesn’t increase our risk of getting sick or having a hangover. It’s the quantity of alcohol consumed — not combined — and the rate at which we’re consuming it that influences intoxication and sickness. In other words, the problem with mixing beer and wine is that it usually leads to higher amounts of alcohol consumed more quickly in one sitting. This puts us in danger of intoxication and feeling hungover the next day.
If you’re struggling to manage your alcohol consumption, consider trying Reframe. We’re a science-backed app that has helped millions of people cut back on their alcohol consumption and enhance their physical, mental, and emotional well-being.

Learn the effects of daily tequila on your body—blood sugar, liver, immune system, mental health, hydration, and more. Expert insights from Reframe App.
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually, with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet millions of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
In the world of booze, tequila packs a unique punch. Here’s how author Laurie Perez describes it in Torpor: Though the Heart Is Warm: “We force a dull clash of cups and pour everything down at once. The hard tequila shudders that never happen in the movies. First your head feels light, then it starts receiving the distress signals from the throat, lungs, belly. Your shoulders jerk to shake off the snake that wrapped around you and squeezed. It burns. The good burn.”
It’s a party, and someone shouts "Tequila!" Suddenly, it’s shot glasses for everyone. But what exactly does that shot of tequila do to your body? Is tequila good for you? Or, rather, is tequila healthy compared to other types of booze?
Let’s just say it might not be the party pleaser it’s made out to be. After learning more about the components of tequila and the science behind it, we can understand how it affects our body at a deeper level.

Tequila, primarily produced in Mexico, is made from the blue agave plant. Native to Mexico's sun-drenched fields, the blue agave looks like an oversized aloe vera with long, spiky leaves, and it can take 7-10 years to reach maturity. The environment, soil composition, and cultivation techniques all play a role in giving tequila its unique profile.
There are the main types of tequila:
As for the chemical components of tequila, here’s the inside scoop:
When tequila enters the body, its effects include more than just a potential dance on the table. Here are 5 ways in which tequila affects the body:
Stage 1: The Absorption Phase
Tequila, like all alcoholic beverages, undergoes an absorption phase when consumed. This phase is critical in determining how quickly the effects of alcohol are felt in the body. Once ingested, the alcohol enters our bloodstream through the stomach and intestines. This is where the "buzz" starts, as our blood alcohol content (BAC) rises.
Tequila, given its alcohol content, is absorbed relatively quickly into the bloodstream. The rate of absorption can be influenced by various factors:
While the liver metabolizes most of the alcohol we consume, around 20% is directly absorbed through the stomach lining into the bloodstream. This is why the effects of alcohol, including tequila, can be felt shortly after drinking.
A rapid rise in BAC leads to intoxication, reduced inhibitions, and impaired judgment. Tequila's high alcohol content and its potential for rapid absorption, especially on an empty stomach, can lead to a swift increase in BAC.
During the absorption phase, as BAC rises, we might experience mood elevation, increased sociability, and a sense of relaxation. However, these effects are short-lived, and they quickly turn negative with overconsumption. The line between pleasure and risk is thin, especially with drinks as potent as tequila.
Stage 2: The Unique Agave Effect
The agavins (natural sugars) in tequila have a unique role in the absorption process. Agavins are derived from the blue agave plant, and no, they're not similar to the agave syrup you might drizzle over your pancakes. Unlike the more commonly known agave nectar or syrup found in stores, agavins are not sweet and cannot be used as sweeteners.
If you've ever noticed that tequila gives you a different "buzz" compared to other drinks, agavins’ unique composition might be the reason. Some studies suggest they act more like dietary fibers and are not easily broken down. Bypassing the usual digestive process means that agavins might not raise blood sugar levels in the same way other sugars might.
As a result, tequila offers a slightly different metabolic experience than other alcoholic drinks, possibly leading to a smoother, more gradual sensation of intoxication. Some tequila drinkers report a “cleaner” or “smoother” buzz, which might be attributed, in part, to agavins.
But is tequila “good” for you? Before you start considering tequila a health drink, pump the brakes. While there's some talk about agavins possibly aiding in weight loss or benefiting gut health, concrete evidence is still on the horizon. Tequila is still a potent beverage, and the overall negative impact of the alcohol in it remains the same.
Stage 3: Entering the Brain
Alcohol affects neurotransmitters in the brain, impacting coordination, judgment, and mood, and tequila is no exception. In fact, its rapid absorption might lead to faster perceived effects on mood and judgment.
Once tequila is in the bloodstream, it makes a beeline for the brain. There it interferes with several processes, and the effects can take effect quite quickly:

Stage 4: The Dehydration Twist
We've all been there — waking up the morning after a tequila night with a mouth that feels like the Sahara and a thirst that could drain a water cooler. Why can tequila leave us so parched?
Stage 5: Body Temperature Fluctuations
Tequila can cause a rapid spike in body temperature. That warmth that we may feel right after a shot? It's not just the burn of the drink — it’s our body reacting to the alcohol.
Tequila has a direct influence on our body's temperature dynamics:
As we can see, tequila can have a profound effect on the physical processes in our body, some of which might not be obvious at first glance.
While a hangover is a temporary discomfort, consistent drinking can lead to more severe health concerns:
Now that you have the inside scoop on what tequila does to your body, here's how you can take action:
Tequila may have a reputation as the life of the party, but the real story unfolds inside your body. By understanding the science behind the booze and taking actionable steps, you can make more informed decisions about your relationship with tequila and rewrite the story in a way that reflects the authentic you.
Remember, life's a party even without the tequila shots. Celebrate your health and well-being!
In the world of booze, tequila packs a unique punch. Here’s how author Laurie Perez describes it in Torpor: Though the Heart Is Warm: “We force a dull clash of cups and pour everything down at once. The hard tequila shudders that never happen in the movies. First your head feels light, then it starts receiving the distress signals from the throat, lungs, belly. Your shoulders jerk to shake off the snake that wrapped around you and squeezed. It burns. The good burn.”
It’s a party, and someone shouts "Tequila!" Suddenly, it’s shot glasses for everyone. But what exactly does that shot of tequila do to your body? Is tequila good for you? Or, rather, is tequila healthy compared to other types of booze?
Let’s just say it might not be the party pleaser it’s made out to be. After learning more about the components of tequila and the science behind it, we can understand how it affects our body at a deeper level.

Tequila, primarily produced in Mexico, is made from the blue agave plant. Native to Mexico's sun-drenched fields, the blue agave looks like an oversized aloe vera with long, spiky leaves, and it can take 7-10 years to reach maturity. The environment, soil composition, and cultivation techniques all play a role in giving tequila its unique profile.
There are the main types of tequila:
As for the chemical components of tequila, here’s the inside scoop:
When tequila enters the body, its effects include more than just a potential dance on the table. Here are 5 ways in which tequila affects the body:
Stage 1: The Absorption Phase
Tequila, like all alcoholic beverages, undergoes an absorption phase when consumed. This phase is critical in determining how quickly the effects of alcohol are felt in the body. Once ingested, the alcohol enters our bloodstream through the stomach and intestines. This is where the "buzz" starts, as our blood alcohol content (BAC) rises.
Tequila, given its alcohol content, is absorbed relatively quickly into the bloodstream. The rate of absorption can be influenced by various factors:
While the liver metabolizes most of the alcohol we consume, around 20% is directly absorbed through the stomach lining into the bloodstream. This is why the effects of alcohol, including tequila, can be felt shortly after drinking.
A rapid rise in BAC leads to intoxication, reduced inhibitions, and impaired judgment. Tequila's high alcohol content and its potential for rapid absorption, especially on an empty stomach, can lead to a swift increase in BAC.
During the absorption phase, as BAC rises, we might experience mood elevation, increased sociability, and a sense of relaxation. However, these effects are short-lived, and they quickly turn negative with overconsumption. The line between pleasure and risk is thin, especially with drinks as potent as tequila.
Stage 2: The Unique Agave Effect
The agavins (natural sugars) in tequila have a unique role in the absorption process. Agavins are derived from the blue agave plant, and no, they're not similar to the agave syrup you might drizzle over your pancakes. Unlike the more commonly known agave nectar or syrup found in stores, agavins are not sweet and cannot be used as sweeteners.
If you've ever noticed that tequila gives you a different "buzz" compared to other drinks, agavins’ unique composition might be the reason. Some studies suggest they act more like dietary fibers and are not easily broken down. Bypassing the usual digestive process means that agavins might not raise blood sugar levels in the same way other sugars might.
As a result, tequila offers a slightly different metabolic experience than other alcoholic drinks, possibly leading to a smoother, more gradual sensation of intoxication. Some tequila drinkers report a “cleaner” or “smoother” buzz, which might be attributed, in part, to agavins.
But is tequila “good” for you? Before you start considering tequila a health drink, pump the brakes. While there's some talk about agavins possibly aiding in weight loss or benefiting gut health, concrete evidence is still on the horizon. Tequila is still a potent beverage, and the overall negative impact of the alcohol in it remains the same.
Stage 3: Entering the Brain
Alcohol affects neurotransmitters in the brain, impacting coordination, judgment, and mood, and tequila is no exception. In fact, its rapid absorption might lead to faster perceived effects on mood and judgment.
Once tequila is in the bloodstream, it makes a beeline for the brain. There it interferes with several processes, and the effects can take effect quite quickly:

Stage 4: The Dehydration Twist
We've all been there — waking up the morning after a tequila night with a mouth that feels like the Sahara and a thirst that could drain a water cooler. Why can tequila leave us so parched?
Stage 5: Body Temperature Fluctuations
Tequila can cause a rapid spike in body temperature. That warmth that we may feel right after a shot? It's not just the burn of the drink — it’s our body reacting to the alcohol.
Tequila has a direct influence on our body's temperature dynamics:
As we can see, tequila can have a profound effect on the physical processes in our body, some of which might not be obvious at first glance.
While a hangover is a temporary discomfort, consistent drinking can lead to more severe health concerns:
Now that you have the inside scoop on what tequila does to your body, here's how you can take action:
Tequila may have a reputation as the life of the party, but the real story unfolds inside your body. By understanding the science behind the booze and taking actionable steps, you can make more informed decisions about your relationship with tequila and rewrite the story in a way that reflects the authentic you.
Remember, life's a party even without the tequila shots. Celebrate your health and well-being!

Find out which drinks to choose and avoid if you have heartburn, plus tips on the worst alcohol for acid reflux and how to enjoy a night out comfortably.
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually, with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet millions of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
We’ve all felt it: that sudden, uncomfortable burning sensation that starts in your chest and creeps up your throat. But have you ever noticed it’s worse after certain drinks? Maybe one glass of wine is fine, but a beer triggers it instantly. If you're tired of guessing, you're in the right place. We’ll help you pinpoint the worst alcohol for acid reflux and even find the best alcohol for acid reflux. Understanding the difference between drinks is key to enjoying a night out without the burn later.
Believe it or not, heartburn isn't a modern phenomenon resulting from our love for spicy tacos or greasy burgers. Our ancestors experienced it, too! Historical texts and records from ancient Greece and Egypt describe symptoms that closely resemble modern-day heartburn. They even had their own remedies: a mixture of herbs, roots, and sometimes, quirky rituals.
It’s also a known fact that alcohol can make the problem worse. Let’s explore the connection between heartburn, drinking alcohol, and what different types of alcohol mean for acid reflux.

Let’s start by clarifying: in spite of what the name suggests, heartburn has nothing to do with the heart. The term likely comes from the location of the pain. The burning sensation often felt in the center of the chest can mimic the discomfort one might feel with heart issues. However, heartburn is all about the digestive system.
When we eat, our food travels from the mouth to the stomach via the esophagus. At the bottom of the esophagus is a muscular valve called the lower esophageal sphincter (LES). Its main job is to act as a one-way gate, letting food in and keeping stomach acids from coming back up.
However, sometimes, the LES doesn't close properly or opens too often, allowing stomach acid to creep up into the esophagus. This acid, which is great for breaking down food in the stomach, irritates the esophagus lining, leading to that familiar burning sensation.
Certain factors can make acid reflux more likely:
Each case is a little different, and triggers can shift over time. For example, some people find that certain foods that used to cause heartburn no longer do, while new culprits might appear on the scene. It’s good to keep track of the factors that seem to aggravate heartburn — preventing it before it begins is always our best bet.
Track Your Drinking Habits! Start For Free!
Click to Know More!It's worth noting that occasional heartburn is common and is not a cause for alarm. However, frequent episodes can be a sign of a more serious condition called gastroesophageal reflux disease (GERD). This chronic condition can lead to complications if not addressed. The combination of alcohol and GERD can worsen symptoms such as heartburn. If heartburn symptoms persist, it's essential to see a healthcare professional. For people already diagnosed with GERD, researching the relationship between GERD and alcohol may be helpful for understanding and mitigating adverse symptoms.
If you've ever indulged in a glass of wine, a cold beer, or a cocktail and soon after felt the sting of heartburn, you're not alone. While alcohol might be responsible for many merry moments and relaxed evenings, it can be a prime culprit behind that unwelcome fiery feeling in your chest. Let's demystify why alcohol and heartburn often go hand in hand.
When you have heartburn, drinking alcohol is clearly a gamble. While it's undeniable that alcohol plays a part in inducing heartburn, not all drinks are made equal when it comes to acid reflux. For instance, carbonated alcoholic beverages (like certain beers) increase the risk of heartburn due to their bubbly nature. Meanwhile, high-proof spirits might irritate the esophagus more due to their higher alcohol content. Let’s explore this subject of heartburn from alcohol in more detail as we take a closer look at wine, beer, hard liquor, and mixed drinks, and learn what is the best alcoholic drink for acid reflux!
When it comes to heartburn, not all alcoholic drinks are created equal, and the Alcohol by Volume (ABV) plays a significant role. Think of ABV as the drink's potency — the higher the percentage, the more alcohol it contains. Drinks with a higher ABV, like spirits such as whiskey and Scotch, are often more likely to trigger acid reflux. This is because concentrated alcohol can be more irritating to the stomach lining and the esophagus. If you're someone who frequently experiences heartburn, opting for drinks with a lower ABV might be a gentler choice for your digestive system. This is a core principle of mindful drinking: paying attention to how different drinks affect your body and making choices that support your well-being.
We’ve already touched on the main ways alcohol can lead to heartburn, but it’s worth a quick recap of the science. Alcohol relaxes the lower esophageal sphincter (LES), prompts the stomach to produce more acid, slows down how quickly the stomach empties, and can directly irritate the lining of your esophagus. It’s a four-pronged attack on your digestive comfort. But the type of alcohol is only part of the story; what it’s mixed with matters just as much. High-acid mixers like citrus juices (think margaritas and screwdrivers) are common culprits. Other ingredients like peppermint, chocolate, or coffee can also spell trouble for heartburn sufferers. Everyone’s triggers are unique, so listening to your body is key to figuring out what works for you.
When deciding between red and white wine, you might be surprised to learn that the color does play a role in its potential to cause acid reflux. So if you're choosing between the two, red wine might be the lesser of two evils. But remember: it still has the potential to cause heartburn.
Moreover, wine is often enjoyed with a meal. The type of food you pair with your wine can either amplify or mitigate heartburn risks. A spicy or very fatty meal, combined with wine, can be a recipe for increased acid reflux. Pairing wine with milder foods might help balance things out.
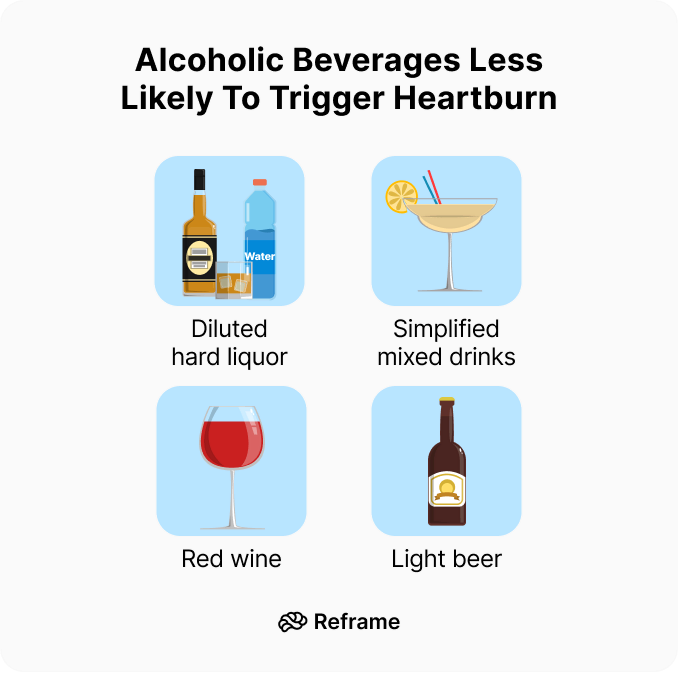
Beer, often referred to as “liquid bread,” has been a part of human life for thousands of years. However, for those prone to acid reflux, that comforting mug of beer might sometimes lead to uncomfortable consequences. Let's take a closer look at beer and its ties to acid reflux.
Beer is a fermented beverage made primarily from water, barley, hops, and yeast. The fermentation process results not just in alcohol — which enough to cause acid reflux by relaxing the LES — but also in certain compounds and gasses that can play a role in digestion:
The wide world of beer offers a diverse range of flavors and styles, from light lagers to rich stouts. The differences in ingredients and brewing processes can affect their potential to instigate reflux. While individual reactions may vary, it's always a good idea to be mindful and notice if a particular type of beer consistently triggers discomfort.
Spirits like whiskey, gin, and vodka might seem tempting, but they contain higher alcohol content, which can more readily relax the esophageal sphincter.
When it comes to beverages, hard liquor stands apart with its potent punch and distinct flavors. Whether it's a neat shot of whiskey, a gin on the rocks, or a simple vodka mixer, spirits are often the go-to choice for many. But how do these strong beverages fare when it comes to acid reflux? Let's sift through the facts.
The distinguishing feature of hard liquor over other alcoholic beverages is its higher alcohol content. Here's how that plays into acid reflux:
Often, spirits aren't consumed alone. They're mixed with a variety of beverages, from sodas to fruit juices. These mixers can be a double-edged sword:
You might wonder if reaching for a clear spirit like vodka or gin is a better choice than a dark one like whiskey or rum. The color difference isn't just for show; it comes from the aging process. Dark liquors spend time in barrels, picking up compounds that give them their distinct color and flavor. These compounds can be potential irritants for some people's stomachs. Clear spirits, on the other hand, are typically filtered to remove these extras, making them a purer form of alcohol. For this reason, some people find that clear liquors are a bit gentler on their digestive system.
However, it's important to remember the main issue with any hard liquor: its high alcohol content. Whether it's clear or dark, a concentrated spirit can relax the lower esophageal sphincter more effectively than beer or wine. So, while a clear spirit might have fewer potential irritants, the alcohol itself is still a primary trigger for acid reflux. Think of it as choosing the lesser of two evils — the fundamental risk remains the same because of the alcohol concentration.
Start Your Drink Less Journey Now!
Start For Free!Mixed drinks, with their variety and versatility, often steal the spotlight at gatherings and nights out. But how do these concoctions interact with acid reflux?
When we talk about mixed drinks, we're addressing a fusion of ingredients. Each component can play a role in influencing heartburn:
Some mixed drinks inherently pose a higher risk for reflux than others due to their ingredient list. A cocktail with multiple acidic components and carbonation might be more problematic than a simpler mix with non-acidic elements.
For those who have a soft spot for mixed drinks but are wary of acid reflux, a bit of cocktail creativity can go a long way:
The spirit in your glass is only half the story; the mixer you choose plays a huge role in whether you’ll feel that familiar burn later. Instead of reaching for highly acidic or bubbly options, think about gentler alternatives. Choose light juices like apple, pear, or cranberry, which are less likely to cause irritation than their citrusy counterparts like orange or grapefruit juice. If you prefer a simpler drink, try diluting your spirit with plain water or a soothing herbal infusion. This not only reduces the alcohol concentration but also avoids adding extra acid or carbonation. And if you just can’t resist a drink with a splash of citrus, make sure to have a glass of plain water on the side to help balance things out and keep your digestive system happy.
Some cocktails are practically designed to trigger heartburn. Drinks that rely heavily on citrus juice — think margaritas, daiquiris, and screwdrivers — are often the biggest offenders because of their high acid content. Carbonated mixers like soda and tonic water can also be problematic, as the fizz can increase pressure in your stomach and encourage acid to travel upward. Beyond the obvious, be mindful of other common triggers that can sneak into cocktails, such as peppermint, chocolate, and coffee. Being aware of these problematic ingredients can help you scan a menu and confidently choose a drink that’s less likely to cause discomfort later on.
So after diving deep into the world of wine, beer, hard liquor, and mixed drinks, what's the consensus on which are the best options for people dealing with acid reflux? Let's bring it all together.
If you’re struggling with acid reflux, avoid anything that will irritate your digestive tract further. In addition to alcohol, coffee and sometimes green tea can be an irritant, so opt for chamomile or rooibos instead. Smoothies, coconut water, and non-acidic juices are all great options as well. And if you’re set on having an alcoholic drink, choose one that has a lower alcohol content and low acidity, such as a light beer.
If you're a fan of spirits, you'll be glad to know some options are less likely to cause that fiery feeling. Generally, liquors with lower acidity are your best bet. According to the Tampa Bay Reflux Center, "Gin, tequila, and non-grain vodkas are generally the best choices because they have lower acidity." This means they are less likely to irritate your esophagus. Non-grain vodkas, which are made from things like potatoes or grapes instead of wheat or rye, can be particularly gentle. The distillation process for these spirits also removes many of the congeners and other compounds that can contribute to digestive upset, making them a cleaner choice if you’re trying to avoid heartburn.
Beyond the usual clear spirits, there are a few other interesting choices that some people find easier on the stomach. Good quality single malt scotch, for example, is often suggested as a gentler option. The key here is "good quality," as premium spirits tend to be more refined. You might also consider Japanese beverages like sake or shochu. Sake is a fermented rice beverage (often called rice wine), while shochu is a distilled spirit that can be made from barley, sweet potatoes, or rice. Both are known for their clean profiles, which can be less aggravating for a sensitive digestive system.
Have you ever heard of a digestif? It’s a drink traditionally served after a meal with the specific purpose of aiding digestion. While it might sound counterintuitive to have more alcohol, many of these drinks are made with herbs and botanicals that have been used for centuries to settle the stomach. Think of Italian Amaros like Averna or Montenegro, or other well-known options like Jägermeister and Limoncello. These drinks often have a bittersweet flavor profile that is thought to stimulate digestive enzymes. While they still contain alcohol, choosing a small serving of a digestif instead of a high-acid wine or a sugary cocktail could be a more comfortable way to end your evening.
Start Your Custom Plan With Reframe!
Join Now!Understanding the roots and mechanics of heartburn can provide not just relief but empowerment. It's always good to know what's happening inside our body and why.
Thankfully, with modern science and medical advancements, we have a clearer understanding of heartburn's causes and treatments, from over-the-counter antacids to lifestyle changes, making it easier for us to find relief. These are some common treatments:
If you have GERD or are prone to heartburn, the safest bet is to avoid alcohol altogether. However, if you do decide to have a drink, the key is to listen to your body and understand your personal limits. For many people, sticking to just one drink can make a world of difference. This practice of mindful drinking isn't about deprivation; it's about being present and aware of how alcohol affects you. By savoring a single, well-chosen beverage, you can reduce the likelihood of relaxing your LES too much and triggering that familiar burn, allowing you to enjoy a social occasion without the uncomfortable after-effects.
Timing is everything, especially when it comes to avoiding nighttime heartburn. When you lie down, you lose the help of gravity, which normally keeps your stomach contents where they belong. Drinking or eating anything within two to three hours of bedtime can set you up for a rough night of acid reflux and regurgitation. To give your digestive system a fighting chance, try to make your last sip of alcohol (and your last bite of food) happen at least three hours before you hit the pillow. This buffer period gives your stomach time to empty, significantly lowering the risk of acid creeping up your esophagus while you sleep.
Sometimes, it’s not just the alcohol itself but what’s mixed with it that causes problems. Many popular cocktails contain ingredients that are well-known acid reflux triggers on their own. Be particularly wary of drinks that include peppermint, chocolate, or coffee, as these can relax the LES and worsen heartburn. This means you might want to steer clear of creamy, dessert-like drinks such as a Grasshopper or a White Russian. Always consider the entire ingredient list of a cocktail before you order, as these hidden culprits can easily turn a pleasant evening into an uncomfortable one.
If you love a good margarita or a gin and tonic with a lime wedge, you don’t have to give them up entirely. While citrus is highly acidic and a common heartburn trigger, there’s a simple way to counteract its effects. If you’re having a drink with citrus, make a point to drink plenty of plain water alongside it. The water helps dilute the acid in your stomach, balancing its overall pH and reducing the chances of irritation. This easy trick allows you to enjoy the zesty flavors you love while being proactive about preventing the burn.
Keep these general tips in mind to avoid alcohol heartburn:
While cutting back or quitting alcohol is a commendable decision for numerous health reasons, understanding the nuanced relationship between heartburn and your drink choice is crucial. Always listen to your body, and when in doubt, consult with a healthcare professional. After all, a little knowledge (and maybe a splash of water in your drink) can go a long way in keeping that heartburn at bay. Here’s to smarter sipping — whether that means moderation or a refreshing glass of water!
Why does white wine seem to cause more heartburn than red wine? The main difference comes down to acidity. White wines are generally more acidic than red wines, and that crisp taste can directly irritate the lining of your esophagus. While red wine is often a gentler choice, it's not entirely risk-free. All alcohol, regardless of color, can relax the muscular valve at the bottom of your esophagus, which is the primary reason acid can creep back up.
Are clear spirits like vodka really better for acid reflux than dark ones like whiskey? While the high alcohol content in any spirit is the main trigger, the color can play a small role. Dark liquors get their color and flavor from compounds they absorb while aging in barrels, and these can sometimes be irritating. Clear spirits are typically filtered to be purer. For this reason, some people find that gin, tequila, or non-grain vodkas are a bit easier on their system. The most important factor, however, is diluting the spirit and drinking in moderation.
Besides the alcohol itself, what are the biggest heartburn triggers in cocktails? The mixers are often the biggest problem. Highly acidic ingredients like citrus juices (lemon, lime, orange, grapefruit) are common offenders. Carbonated mixers like soda and tonic water are also problematic because the bubbles can increase pressure in your stomach. You should also be mindful of other common triggers that can sneak into cocktails, such as peppermint, chocolate, or coffee.
Is there a "safest" time of day to have a drink to avoid heartburn? Yes, timing can make a huge difference. Try to have your last drink at least three hours before you plan to lie down. When you're upright, gravity is on your side, helping to keep stomach acid from traveling up your esophagus. Giving your body this buffer period allows your stomach to process the drink and begin to empty, significantly lowering your risk of uncomfortable nighttime reflux.
If I have to choose, what's the single best type of alcoholic drink to avoid acid reflux? While no alcohol is completely safe for heartburn sufferers, your best option is a drink with a lower alcohol content that is also low in acid and not carbonated. A diluted spirit, such as gin or a non-grain vodka mixed with a gentle, non-citrus juice like pear or apple, is often the most stomach-friendly choice. This approach minimizes the alcohol's direct impact and avoids adding extra irritants from mixers.
We’ve all felt it: that sudden, uncomfortable burning sensation that starts in your chest and creeps up your throat. But have you ever noticed it’s worse after certain drinks? Maybe one glass of wine is fine, but a beer triggers it instantly. If you're tired of guessing, you're in the right place. We’ll help you pinpoint the worst alcohol for acid reflux and even find the best alcohol for acid reflux. Understanding the difference between drinks is key to enjoying a night out without the burn later.
Believe it or not, heartburn isn't a modern phenomenon resulting from our love for spicy tacos or greasy burgers. Our ancestors experienced it, too! Historical texts and records from ancient Greece and Egypt describe symptoms that closely resemble modern-day heartburn. They even had their own remedies: a mixture of herbs, roots, and sometimes, quirky rituals.
It’s also a known fact that alcohol can make the problem worse. Let’s explore the connection between heartburn, drinking alcohol, and what different types of alcohol mean for acid reflux.

Let’s start by clarifying: in spite of what the name suggests, heartburn has nothing to do with the heart. The term likely comes from the location of the pain. The burning sensation often felt in the center of the chest can mimic the discomfort one might feel with heart issues. However, heartburn is all about the digestive system.
When we eat, our food travels from the mouth to the stomach via the esophagus. At the bottom of the esophagus is a muscular valve called the lower esophageal sphincter (LES). Its main job is to act as a one-way gate, letting food in and keeping stomach acids from coming back up.
However, sometimes, the LES doesn't close properly or opens too often, allowing stomach acid to creep up into the esophagus. This acid, which is great for breaking down food in the stomach, irritates the esophagus lining, leading to that familiar burning sensation.
Certain factors can make acid reflux more likely:
Each case is a little different, and triggers can shift over time. For example, some people find that certain foods that used to cause heartburn no longer do, while new culprits might appear on the scene. It’s good to keep track of the factors that seem to aggravate heartburn — preventing it before it begins is always our best bet.
Track Your Drinking Habits! Start For Free!
Click to Know More!It's worth noting that occasional heartburn is common and is not a cause for alarm. However, frequent episodes can be a sign of a more serious condition called gastroesophageal reflux disease (GERD). This chronic condition can lead to complications if not addressed. The combination of alcohol and GERD can worsen symptoms such as heartburn. If heartburn symptoms persist, it's essential to see a healthcare professional. For people already diagnosed with GERD, researching the relationship between GERD and alcohol may be helpful for understanding and mitigating adverse symptoms.
If you've ever indulged in a glass of wine, a cold beer, or a cocktail and soon after felt the sting of heartburn, you're not alone. While alcohol might be responsible for many merry moments and relaxed evenings, it can be a prime culprit behind that unwelcome fiery feeling in your chest. Let's demystify why alcohol and heartburn often go hand in hand.
When you have heartburn, drinking alcohol is clearly a gamble. While it's undeniable that alcohol plays a part in inducing heartburn, not all drinks are made equal when it comes to acid reflux. For instance, carbonated alcoholic beverages (like certain beers) increase the risk of heartburn due to their bubbly nature. Meanwhile, high-proof spirits might irritate the esophagus more due to their higher alcohol content. Let’s explore this subject of heartburn from alcohol in more detail as we take a closer look at wine, beer, hard liquor, and mixed drinks, and learn what is the best alcoholic drink for acid reflux!
When it comes to heartburn, not all alcoholic drinks are created equal, and the Alcohol by Volume (ABV) plays a significant role. Think of ABV as the drink's potency — the higher the percentage, the more alcohol it contains. Drinks with a higher ABV, like spirits such as whiskey and Scotch, are often more likely to trigger acid reflux. This is because concentrated alcohol can be more irritating to the stomach lining and the esophagus. If you're someone who frequently experiences heartburn, opting for drinks with a lower ABV might be a gentler choice for your digestive system. This is a core principle of mindful drinking: paying attention to how different drinks affect your body and making choices that support your well-being.
We’ve already touched on the main ways alcohol can lead to heartburn, but it’s worth a quick recap of the science. Alcohol relaxes the lower esophageal sphincter (LES), prompts the stomach to produce more acid, slows down how quickly the stomach empties, and can directly irritate the lining of your esophagus. It’s a four-pronged attack on your digestive comfort. But the type of alcohol is only part of the story; what it’s mixed with matters just as much. High-acid mixers like citrus juices (think margaritas and screwdrivers) are common culprits. Other ingredients like peppermint, chocolate, or coffee can also spell trouble for heartburn sufferers. Everyone’s triggers are unique, so listening to your body is key to figuring out what works for you.
When deciding between red and white wine, you might be surprised to learn that the color does play a role in its potential to cause acid reflux. So if you're choosing between the two, red wine might be the lesser of two evils. But remember: it still has the potential to cause heartburn.
Moreover, wine is often enjoyed with a meal. The type of food you pair with your wine can either amplify or mitigate heartburn risks. A spicy or very fatty meal, combined with wine, can be a recipe for increased acid reflux. Pairing wine with milder foods might help balance things out.
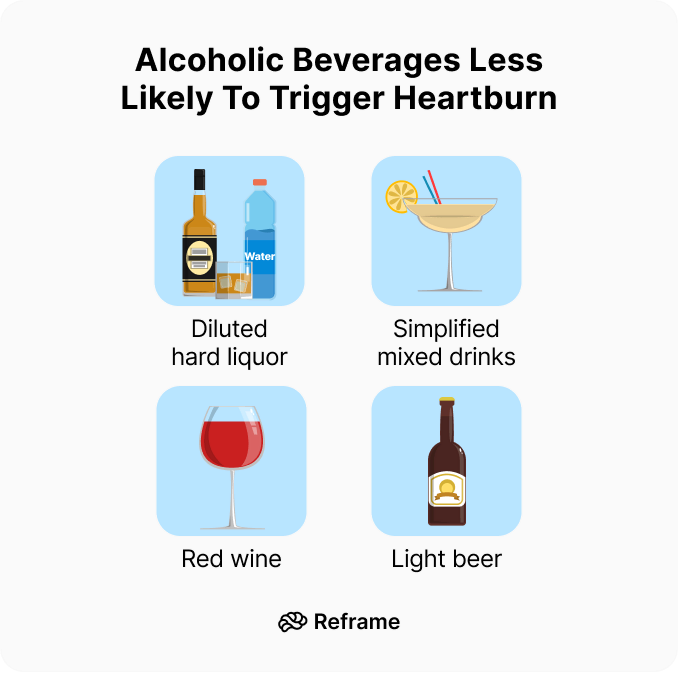
Beer, often referred to as “liquid bread,” has been a part of human life for thousands of years. However, for those prone to acid reflux, that comforting mug of beer might sometimes lead to uncomfortable consequences. Let's take a closer look at beer and its ties to acid reflux.
Beer is a fermented beverage made primarily from water, barley, hops, and yeast. The fermentation process results not just in alcohol — which enough to cause acid reflux by relaxing the LES — but also in certain compounds and gasses that can play a role in digestion:
The wide world of beer offers a diverse range of flavors and styles, from light lagers to rich stouts. The differences in ingredients and brewing processes can affect their potential to instigate reflux. While individual reactions may vary, it's always a good idea to be mindful and notice if a particular type of beer consistently triggers discomfort.
Spirits like whiskey, gin, and vodka might seem tempting, but they contain higher alcohol content, which can more readily relax the esophageal sphincter.
When it comes to beverages, hard liquor stands apart with its potent punch and distinct flavors. Whether it's a neat shot of whiskey, a gin on the rocks, or a simple vodka mixer, spirits are often the go-to choice for many. But how do these strong beverages fare when it comes to acid reflux? Let's sift through the facts.
The distinguishing feature of hard liquor over other alcoholic beverages is its higher alcohol content. Here's how that plays into acid reflux:
Often, spirits aren't consumed alone. They're mixed with a variety of beverages, from sodas to fruit juices. These mixers can be a double-edged sword:
You might wonder if reaching for a clear spirit like vodka or gin is a better choice than a dark one like whiskey or rum. The color difference isn't just for show; it comes from the aging process. Dark liquors spend time in barrels, picking up compounds that give them their distinct color and flavor. These compounds can be potential irritants for some people's stomachs. Clear spirits, on the other hand, are typically filtered to remove these extras, making them a purer form of alcohol. For this reason, some people find that clear liquors are a bit gentler on their digestive system.
However, it's important to remember the main issue with any hard liquor: its high alcohol content. Whether it's clear or dark, a concentrated spirit can relax the lower esophageal sphincter more effectively than beer or wine. So, while a clear spirit might have fewer potential irritants, the alcohol itself is still a primary trigger for acid reflux. Think of it as choosing the lesser of two evils — the fundamental risk remains the same because of the alcohol concentration.
Start Your Drink Less Journey Now!
Start For Free!Mixed drinks, with their variety and versatility, often steal the spotlight at gatherings and nights out. But how do these concoctions interact with acid reflux?
When we talk about mixed drinks, we're addressing a fusion of ingredients. Each component can play a role in influencing heartburn:
Some mixed drinks inherently pose a higher risk for reflux than others due to their ingredient list. A cocktail with multiple acidic components and carbonation might be more problematic than a simpler mix with non-acidic elements.
For those who have a soft spot for mixed drinks but are wary of acid reflux, a bit of cocktail creativity can go a long way:
The spirit in your glass is only half the story; the mixer you choose plays a huge role in whether you’ll feel that familiar burn later. Instead of reaching for highly acidic or bubbly options, think about gentler alternatives. Choose light juices like apple, pear, or cranberry, which are less likely to cause irritation than their citrusy counterparts like orange or grapefruit juice. If you prefer a simpler drink, try diluting your spirit with plain water or a soothing herbal infusion. This not only reduces the alcohol concentration but also avoids adding extra acid or carbonation. And if you just can’t resist a drink with a splash of citrus, make sure to have a glass of plain water on the side to help balance things out and keep your digestive system happy.
Some cocktails are practically designed to trigger heartburn. Drinks that rely heavily on citrus juice — think margaritas, daiquiris, and screwdrivers — are often the biggest offenders because of their high acid content. Carbonated mixers like soda and tonic water can also be problematic, as the fizz can increase pressure in your stomach and encourage acid to travel upward. Beyond the obvious, be mindful of other common triggers that can sneak into cocktails, such as peppermint, chocolate, and coffee. Being aware of these problematic ingredients can help you scan a menu and confidently choose a drink that’s less likely to cause discomfort later on.
So after diving deep into the world of wine, beer, hard liquor, and mixed drinks, what's the consensus on which are the best options for people dealing with acid reflux? Let's bring it all together.
If you’re struggling with acid reflux, avoid anything that will irritate your digestive tract further. In addition to alcohol, coffee and sometimes green tea can be an irritant, so opt for chamomile or rooibos instead. Smoothies, coconut water, and non-acidic juices are all great options as well. And if you’re set on having an alcoholic drink, choose one that has a lower alcohol content and low acidity, such as a light beer.
If you're a fan of spirits, you'll be glad to know some options are less likely to cause that fiery feeling. Generally, liquors with lower acidity are your best bet. According to the Tampa Bay Reflux Center, "Gin, tequila, and non-grain vodkas are generally the best choices because they have lower acidity." This means they are less likely to irritate your esophagus. Non-grain vodkas, which are made from things like potatoes or grapes instead of wheat or rye, can be particularly gentle. The distillation process for these spirits also removes many of the congeners and other compounds that can contribute to digestive upset, making them a cleaner choice if you’re trying to avoid heartburn.
Beyond the usual clear spirits, there are a few other interesting choices that some people find easier on the stomach. Good quality single malt scotch, for example, is often suggested as a gentler option. The key here is "good quality," as premium spirits tend to be more refined. You might also consider Japanese beverages like sake or shochu. Sake is a fermented rice beverage (often called rice wine), while shochu is a distilled spirit that can be made from barley, sweet potatoes, or rice. Both are known for their clean profiles, which can be less aggravating for a sensitive digestive system.
Have you ever heard of a digestif? It’s a drink traditionally served after a meal with the specific purpose of aiding digestion. While it might sound counterintuitive to have more alcohol, many of these drinks are made with herbs and botanicals that have been used for centuries to settle the stomach. Think of Italian Amaros like Averna or Montenegro, or other well-known options like Jägermeister and Limoncello. These drinks often have a bittersweet flavor profile that is thought to stimulate digestive enzymes. While they still contain alcohol, choosing a small serving of a digestif instead of a high-acid wine or a sugary cocktail could be a more comfortable way to end your evening.
Start Your Custom Plan With Reframe!
Join Now!Understanding the roots and mechanics of heartburn can provide not just relief but empowerment. It's always good to know what's happening inside our body and why.
Thankfully, with modern science and medical advancements, we have a clearer understanding of heartburn's causes and treatments, from over-the-counter antacids to lifestyle changes, making it easier for us to find relief. These are some common treatments:
If you have GERD or are prone to heartburn, the safest bet is to avoid alcohol altogether. However, if you do decide to have a drink, the key is to listen to your body and understand your personal limits. For many people, sticking to just one drink can make a world of difference. This practice of mindful drinking isn't about deprivation; it's about being present and aware of how alcohol affects you. By savoring a single, well-chosen beverage, you can reduce the likelihood of relaxing your LES too much and triggering that familiar burn, allowing you to enjoy a social occasion without the uncomfortable after-effects.
Timing is everything, especially when it comes to avoiding nighttime heartburn. When you lie down, you lose the help of gravity, which normally keeps your stomach contents where they belong. Drinking or eating anything within two to three hours of bedtime can set you up for a rough night of acid reflux and regurgitation. To give your digestive system a fighting chance, try to make your last sip of alcohol (and your last bite of food) happen at least three hours before you hit the pillow. This buffer period gives your stomach time to empty, significantly lowering the risk of acid creeping up your esophagus while you sleep.
Sometimes, it’s not just the alcohol itself but what’s mixed with it that causes problems. Many popular cocktails contain ingredients that are well-known acid reflux triggers on their own. Be particularly wary of drinks that include peppermint, chocolate, or coffee, as these can relax the LES and worsen heartburn. This means you might want to steer clear of creamy, dessert-like drinks such as a Grasshopper or a White Russian. Always consider the entire ingredient list of a cocktail before you order, as these hidden culprits can easily turn a pleasant evening into an uncomfortable one.
If you love a good margarita or a gin and tonic with a lime wedge, you don’t have to give them up entirely. While citrus is highly acidic and a common heartburn trigger, there’s a simple way to counteract its effects. If you’re having a drink with citrus, make a point to drink plenty of plain water alongside it. The water helps dilute the acid in your stomach, balancing its overall pH and reducing the chances of irritation. This easy trick allows you to enjoy the zesty flavors you love while being proactive about preventing the burn.
Keep these general tips in mind to avoid alcohol heartburn:
While cutting back or quitting alcohol is a commendable decision for numerous health reasons, understanding the nuanced relationship between heartburn and your drink choice is crucial. Always listen to your body, and when in doubt, consult with a healthcare professional. After all, a little knowledge (and maybe a splash of water in your drink) can go a long way in keeping that heartburn at bay. Here’s to smarter sipping — whether that means moderation or a refreshing glass of water!
Why does white wine seem to cause more heartburn than red wine? The main difference comes down to acidity. White wines are generally more acidic than red wines, and that crisp taste can directly irritate the lining of your esophagus. While red wine is often a gentler choice, it's not entirely risk-free. All alcohol, regardless of color, can relax the muscular valve at the bottom of your esophagus, which is the primary reason acid can creep back up.
Are clear spirits like vodka really better for acid reflux than dark ones like whiskey? While the high alcohol content in any spirit is the main trigger, the color can play a small role. Dark liquors get their color and flavor from compounds they absorb while aging in barrels, and these can sometimes be irritating. Clear spirits are typically filtered to be purer. For this reason, some people find that gin, tequila, or non-grain vodkas are a bit easier on their system. The most important factor, however, is diluting the spirit and drinking in moderation.
Besides the alcohol itself, what are the biggest heartburn triggers in cocktails? The mixers are often the biggest problem. Highly acidic ingredients like citrus juices (lemon, lime, orange, grapefruit) are common offenders. Carbonated mixers like soda and tonic water are also problematic because the bubbles can increase pressure in your stomach. You should also be mindful of other common triggers that can sneak into cocktails, such as peppermint, chocolate, or coffee.
Is there a "safest" time of day to have a drink to avoid heartburn? Yes, timing can make a huge difference. Try to have your last drink at least three hours before you plan to lie down. When you're upright, gravity is on your side, helping to keep stomach acid from traveling up your esophagus. Giving your body this buffer period allows your stomach to process the drink and begin to empty, significantly lowering your risk of uncomfortable nighttime reflux.
If I have to choose, what's the single best type of alcoholic drink to avoid acid reflux? While no alcohol is completely safe for heartburn sufferers, your best option is a drink with a lower alcohol content that is also low in acid and not carbonated. A diluted spirit, such as gin or a non-grain vodka mixed with a gentle, non-citrus juice like pear or apple, is often the most stomach-friendly choice. This approach minimizes the alcohol's direct impact and avoids adding extra irritants from mixers.