

Can you drink on Dramamine, or is it too risky? Read about the possible dangers of this combination in our latest blog.
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet millions of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
Nobody likes to feel nauseous. It’s that indescribable feeling — not quite “pain” but somehow just as bad. And often there seems to be no escape from it. Philosopher Jean-Paul Sartre dedicated a whole novel — Nausea — to the pervasive sensation. He writes, “The nausea has not left me and I don't believe it will leave me so soon; but I no longer have to bear it, it is no longer an illness or a passing fit: it is I.”
So if you tend to get nauseous — on planes, buses, that spinning teacup ride at Disney World — you probably have your travel kit stocked with over-the-counter nausea aids (if only they were around when Sartre’s protagonist was grappling with his affliction!).
But wait a second, is it okay to pop a Dramamine before knocking back a glass of wine on the plane or have a beer after you get off that bumpy bus ride? What are the dangers of mixing Dramamine and alcohol — can you drink on Dramamine at all? And what about using Dramamine for hangover-related nausea? Let’s find out more!

Unfortunately, motion sickness is a part of life for many of us. It can show up during our daily commute to work, in the back seat of an Uber, and even on vacation trips. As scientist Natasha Tuznik tells UC Davis Health, “A study conducted in 2019 found that almost everyone has experienced or will experience motion sickness at some point in their lifetime.”
This “sickness” goes way back — in fact, the word comes from the Greek naus, meaning “ship.” These days, of course, there are many other modes of transportation that seem to conspire to ruin our transit experience.
In a study published in Ergonomics, as many as 28.4% of people surveyed reported feeling ill during a total of 110 hours of test drives that included 5 types of vehicles and 17 different drivers. Moreover, 12.8% reported experiencing nausea, while 1.7% brave participants admitted to “losing their lunch” during the experiment!
Riding in cars is part of modern life. Thankfully, so is modern science! Enter: Dramamine.
Dramamine (Dimenhydrinate) is an antihistamine used to kick the most unpleasant symptoms of motion sickness (such as nausea, vomiting, and dizziness) right to the curb. In fact, it can even prevent them from starting in the first place!
Know Dramamine by another name? That’s quite possible. According to ScienceDirect, this trusty travel companion has many aliases:
Phew! That’s quite a list. Whichever alias you know it by, they all work the same way — and the mechanism is pretty clever!
Dramamine helps our body maintain a sense of balance during those bumpy bus rides and turbulent takeovers. It works by blocking certain signals in the brain that trigger these uncomfortable symptoms, providing much-needed relief during travel. While taking a pill when symptoms kick in is an option (it’s never too late!), many travelers opt for taking the precaution of popping one an hour or so before even getting on the bus (or plane, or car).
As for dosage, the standard for adults is 50-100 mg every 4-6 hours, with 400 mg per day being the limit.
While Dramamine is all about reducing the unpleasant “side effects” of travel, it comes with a bit of baggage of its own. The common side effects are usually pretty mild:
So what happens when we add alcohol to the mix? There are a couple of reasons why the two are not great “travel companions”:
Dramamine can make us drowsy on its own, but with alcohol in the picture, the effect gets much more pronounced — sometimes to a dangerous degree. As a depressant, alcohol numbs our senses and slows cognitive processing while impairing our motor skills.
The reason has to do with the way it affects our brain chemistry. Alcohol tends to increase the activity of GABA, an inhibitory neurotransmitter that slows down the nervous system, while simultaneously toning down the effects of glutamate, its “excitatory” counterpart. The result? Our reflexes take a hit, our cognitive abilities are dulled, and we feel drowsy.
The booze-dramamine combo can dangerously enhance impairment, raising the risk of accidents and injuries, especially in activities requiring alertness, such as driving. However, even if we’re not behind the wheel, the extra grogginess can get in the way. (After all, nobody wants to miss their connecting flight!) And if we end up having several drinks, we could get into dangerous waters by slowing down our central nervous system so much that it becomes a health risk.
Alcohol is notorious for leaving us parched and depleted of electrolytes, and adding Dramamine to the mix can make things worse. This dehydrating duo will leave you twice as thirsty — especially after a long plane ride!
Mixing alcohol and Dramamine can also worsen other side effects, such as dry mouth, blurred vision, and dizziness. If we’re already feeling drowsy, this could really spell trouble, especially for those of us who are a bit older.
You might be wondering, “How long after taking Dramamine can I drink alcohol?” The effects of the medication can last from 4 to 6 hours, and it takes about 1 to 3 hours for its peak effects to show up. Given its half-life, it's best to wait at least 24 hours after taking Dramamine before drinking so your body can fully process the medication. Waiting an extra few hours might reduce the risk of adverse interactions even more.
Is one drink okay to have with Dramamine? Not really. Even one drink can significantly increase the side effects and amp up the risks, so it's best to skip booze entirely until the medication has cleared from your system.
Given that nausea is a common hangover symptom, it seems that it would make sense to reach for a Dramamine pill for relief.
But is it a good idea? Not so much.
It’s true that Dramamine can potentially alleviate some symptoms of a hangover, such as nausea and a sense of balance disruption. However, Dramamine’s sedative effects can add to the grogginess and cognitive fuzziness often experienced during a hangover.
Moreover, taking Dramamine to combat hangover symptoms can be risky if alcohol is still present in the system. The combination can lead to increased drowsiness, dehydration, and further impairment of judgment and motor skills.
Moreover, it’s also worth noting that while Dramamine tends to be safe for many people when it comes to potential misuse, for some it’s been known to be habit-forming (sometimes very much so — we’re talking large daily doses). If we have a history of substance misuse, it’s important to be careful and mindful about our Dramamine intake.
Finally, many of us might have noticed that Dramamine has a travel partner that usually shares the same shelf in the drug store — Bonine. Is this a better choice to take along for the ride if we know we might drink?
Bonine (meclizine) is also marketed as a motion sickness aid but one that claims to work all day — as opposed to Dramamine’s 4- to 6-hour window. Unfortunately for those who might have been hoping Bonine could work as a booze-friendly alternative to Dramamine, this isn’t the case. Bonine shares the same risk of central nervous system suppression — along with increased dehydration and intensified side effects.
To ensure safety, it’s best to avoid alcohol when taking any motion sickness medication.

Ready for some tips on how to relieve nausea and hangovers more effectively (and maybe prevent them altogether)? Here we go!
If you’re finding that alcohol is taking up a bit too much air time in your life in general — whether or not Dramamine is part of the picture — here are some additional tips for the journey.
Nausea is, unfortunately, a part of life, and it’s great that Dramamine is here to help. But the not-so-helpful interactions between this medication and alcohol don’t have to be part of your journey. Happy booze-free, hangover-free travels!
Nobody likes to feel nauseous. It’s that indescribable feeling — not quite “pain” but somehow just as bad. And often there seems to be no escape from it. Philosopher Jean-Paul Sartre dedicated a whole novel — Nausea — to the pervasive sensation. He writes, “The nausea has not left me and I don't believe it will leave me so soon; but I no longer have to bear it, it is no longer an illness or a passing fit: it is I.”
So if you tend to get nauseous — on planes, buses, that spinning teacup ride at Disney World — you probably have your travel kit stocked with over-the-counter nausea aids (if only they were around when Sartre’s protagonist was grappling with his affliction!).
But wait a second, is it okay to pop a Dramamine before knocking back a glass of wine on the plane or have a beer after you get off that bumpy bus ride? What are the dangers of mixing Dramamine and alcohol — can you drink on Dramamine at all? And what about using Dramamine for hangover-related nausea? Let’s find out more!

Unfortunately, motion sickness is a part of life for many of us. It can show up during our daily commute to work, in the back seat of an Uber, and even on vacation trips. As scientist Natasha Tuznik tells UC Davis Health, “A study conducted in 2019 found that almost everyone has experienced or will experience motion sickness at some point in their lifetime.”
This “sickness” goes way back — in fact, the word comes from the Greek naus, meaning “ship.” These days, of course, there are many other modes of transportation that seem to conspire to ruin our transit experience.
In a study published in Ergonomics, as many as 28.4% of people surveyed reported feeling ill during a total of 110 hours of test drives that included 5 types of vehicles and 17 different drivers. Moreover, 12.8% reported experiencing nausea, while 1.7% brave participants admitted to “losing their lunch” during the experiment!
Riding in cars is part of modern life. Thankfully, so is modern science! Enter: Dramamine.
Dramamine (Dimenhydrinate) is an antihistamine used to kick the most unpleasant symptoms of motion sickness (such as nausea, vomiting, and dizziness) right to the curb. In fact, it can even prevent them from starting in the first place!
Know Dramamine by another name? That’s quite possible. According to ScienceDirect, this trusty travel companion has many aliases:
Phew! That’s quite a list. Whichever alias you know it by, they all work the same way — and the mechanism is pretty clever!
Dramamine helps our body maintain a sense of balance during those bumpy bus rides and turbulent takeovers. It works by blocking certain signals in the brain that trigger these uncomfortable symptoms, providing much-needed relief during travel. While taking a pill when symptoms kick in is an option (it’s never too late!), many travelers opt for taking the precaution of popping one an hour or so before even getting on the bus (or plane, or car).
As for dosage, the standard for adults is 50-100 mg every 4-6 hours, with 400 mg per day being the limit.
While Dramamine is all about reducing the unpleasant “side effects” of travel, it comes with a bit of baggage of its own. The common side effects are usually pretty mild:
So what happens when we add alcohol to the mix? There are a couple of reasons why the two are not great “travel companions”:
Dramamine can make us drowsy on its own, but with alcohol in the picture, the effect gets much more pronounced — sometimes to a dangerous degree. As a depressant, alcohol numbs our senses and slows cognitive processing while impairing our motor skills.
The reason has to do with the way it affects our brain chemistry. Alcohol tends to increase the activity of GABA, an inhibitory neurotransmitter that slows down the nervous system, while simultaneously toning down the effects of glutamate, its “excitatory” counterpart. The result? Our reflexes take a hit, our cognitive abilities are dulled, and we feel drowsy.
The booze-dramamine combo can dangerously enhance impairment, raising the risk of accidents and injuries, especially in activities requiring alertness, such as driving. However, even if we’re not behind the wheel, the extra grogginess can get in the way. (After all, nobody wants to miss their connecting flight!) And if we end up having several drinks, we could get into dangerous waters by slowing down our central nervous system so much that it becomes a health risk.
Alcohol is notorious for leaving us parched and depleted of electrolytes, and adding Dramamine to the mix can make things worse. This dehydrating duo will leave you twice as thirsty — especially after a long plane ride!
Mixing alcohol and Dramamine can also worsen other side effects, such as dry mouth, blurred vision, and dizziness. If we’re already feeling drowsy, this could really spell trouble, especially for those of us who are a bit older.
You might be wondering, “How long after taking Dramamine can I drink alcohol?” The effects of the medication can last from 4 to 6 hours, and it takes about 1 to 3 hours for its peak effects to show up. Given its half-life, it's best to wait at least 24 hours after taking Dramamine before drinking so your body can fully process the medication. Waiting an extra few hours might reduce the risk of adverse interactions even more.
Is one drink okay to have with Dramamine? Not really. Even one drink can significantly increase the side effects and amp up the risks, so it's best to skip booze entirely until the medication has cleared from your system.
Given that nausea is a common hangover symptom, it seems that it would make sense to reach for a Dramamine pill for relief.
But is it a good idea? Not so much.
It’s true that Dramamine can potentially alleviate some symptoms of a hangover, such as nausea and a sense of balance disruption. However, Dramamine’s sedative effects can add to the grogginess and cognitive fuzziness often experienced during a hangover.
Moreover, taking Dramamine to combat hangover symptoms can be risky if alcohol is still present in the system. The combination can lead to increased drowsiness, dehydration, and further impairment of judgment and motor skills.
Moreover, it’s also worth noting that while Dramamine tends to be safe for many people when it comes to potential misuse, for some it’s been known to be habit-forming (sometimes very much so — we’re talking large daily doses). If we have a history of substance misuse, it’s important to be careful and mindful about our Dramamine intake.
Finally, many of us might have noticed that Dramamine has a travel partner that usually shares the same shelf in the drug store — Bonine. Is this a better choice to take along for the ride if we know we might drink?
Bonine (meclizine) is also marketed as a motion sickness aid but one that claims to work all day — as opposed to Dramamine’s 4- to 6-hour window. Unfortunately for those who might have been hoping Bonine could work as a booze-friendly alternative to Dramamine, this isn’t the case. Bonine shares the same risk of central nervous system suppression — along with increased dehydration and intensified side effects.
To ensure safety, it’s best to avoid alcohol when taking any motion sickness medication.

Ready for some tips on how to relieve nausea and hangovers more effectively (and maybe prevent them altogether)? Here we go!
If you’re finding that alcohol is taking up a bit too much air time in your life in general — whether or not Dramamine is part of the picture — here are some additional tips for the journey.
Nausea is, unfortunately, a part of life, and it’s great that Dramamine is here to help. But the not-so-helpful interactions between this medication and alcohol don’t have to be part of your journey. Happy booze-free, hangover-free travels!

Is mixing cyclobenzaprine and alcohol a bad idea? Find out why Flexeril and alcohol are not a great mix and learn how to stay safe and keep your muscles healthy.
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually, with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet hundreds of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
If you’ve ever gotten a painful muscle spasm, you know it’s no joke. It can jolt you out of sleep or strike during the day, as you go about your business and are suddenly stopped in your tracks by what feels like a pair of tyrannosaurus jaws chomping into your muscles. Those moments can fill you with panic as you try to remember the tricks you’ve heard from your grandmother or read about online. Fill a bathtub with hot water and soak your foot in it? Stand on your heel and bend your toes back? Ugh! Nothing seems to help.
When our muscle pain and spasms become a regular thing, we might end up taking medication such as a muscle relaxant. Cyclobenzaprine (known by the brand name Flexeril) is often prescribed to alleviate spasms related to all sorts of musculoskeletal conditions. But what about cyclobenzaprine and alcohol — is it okay to mix the two? Can you drink on muscle relaxers in general, and what are the possible dangers? Let’s find out!

According to NIH, cyclobenzaprine, a muscle relaxant, is prescribed to help relieve pain from muscle spasms caused by different musculoskeletal conditions. It’s usually not a stand-alone measure, and is used in combination with rest, physical therapy exercises, and other techniques that help relax muscles, quiet pain, and relieve discomfort caused by strains, sprains, and various types of muscle injuries.
Muscle relaxants might sound very modern, but they’re actually nothing new! The earliest “muscle relaxants” were actually poison-tipped arrows used as weapons by peoples in the Amazon Basin in South America. The European explorers picked up on their potential medical applications and used them in early experiments that eventually led to the development of cyclobenzaprine and its many pharmacological cousins. And don’t worry — the variety doled out by the local pharmacy won’t do us any harm, provided we take them as prescribed.
Muscle relaxants work through a few different pathways that all have the same goal — quieting down those overactive signals to prevent painful spasms and muscle hyperactivity. Let’s see what their main mechanisms are and where cyclobenzaprine fits in.
The full list of options for muscle ailments is much longer, but these are the highlights. There are many individual factors that come into play when choosing the right option, and our physician can give us the best idea of which course of treatment is right for us.
Can you drink on muscle relaxers? And more specifically, can you drink alcohol with cyclobenzaprine? As it turns out, it’s not a good idea for several reasons.
Both of the main muscle relaxer types (antispastics and antispasmodics) can have negative interactions with alcohol. Most of the dangers center on amplified side effects (especially sedation). For a deeper look at the dangers of mixing alcohol and muscle relaxants in general, check out “Muscle Relaxers and Alcohol: A Dangerous Mix.” For now, let’s take a closer look at cyclobenzaprine and alcohol in particular.
One of the main reasons it’s best to avoid the combo has to do with some gnarly side effects we can end up with as a result. According to NIH, cyclobenzaprine comes with some fairly typical ones, as well as potentially dangerous ones. None of them mix too well with booze.
This last set of effects is the main reason mixing the two is not recommended, since it increases the chances of having a dangerous fall or another accident. Besides, the sedation could land us in dangerous waters if our heart and breathing rate slows down too much, causing respiratory depression.
Because of this, driving or operating machinery is out of the question (even if we’re below the legal alcohol limit). It’s important to stay safe and protect others around us!
Another reason why cyclobenzaprine and alcohol are a dangerous combination? Our liver probably won’t be too happy with the mix. Both substances are processed by the liver, which is already in danger of becoming overwhelmed by alcohol alone. Adding another burdensome to-do list item to its task list is asking for trouble.
Studies show that mixing alcohol and medications that are processed by the liver leads to a less-than-favorable metabolic fallout. Specifically, we end up with elevated levels of certain enzymes. The result? Higher fat deposits and overall stress that can eventually result in liver disease and other complications.
Alcohol’s effect on the heart could also put us at risk if we’re taking cyclobenzaprine. Booze is notorious for messing with our blood pressure, decreasing it at first through vasodilation (the widening of blood vessels) before leading to a rebound effect. It also causes potentially dangerous arrhythmias and increases our heart rate. Over time, these disruptions could even lead to cardiomyopathy — a serious form of heart disease. (For more information take a look at “How Does Alcohol Affect the Heart?”).
Moreover, alcohol’s effect on muscles can be counterproductive during the healing process. Science shows that alcohol contributes to muscle degeneration, gets in the way of muscle-building, and even leads to muscle atrophy in the long run.
Finally, there’s the matter of dependency. As we know, alcohol can be notoriously addictive since it affects the brain’s levels of dopamine, a “reward” neurotransmitter involved in pleasure-seeking behavior. Dopamine gets released through activities that make us feel good (delicious food, good company, a date that ends well — you get the picture). However, substances like alcohol cause an unnatural flood of dopamine that the brain eventually gets used to and comes to expect, leading us to become more and more dependent on that weekly (or nightly) drink.
Muscle relaxers affect our cognition a bit differently but can play a role in this process. By affecting our nervous system, they lower our “cognitive defenses,” making it more likely we’ll jump into certain situations or make decisions without thinking. Our inhibitions might be lower, and we might end up drinking more as a result, paving the way for potential problems in the future.

Cyclobenzaprine has a half-life of about 18 hours, which means that within 18 hours, half of it is no longer in our body. (It’s usually taken 3 times a day and is meant for short-term use — 2 or 3 weeks at most). Doctors generally recommend waiting at least 48 hours before drinking. (Of course, we might want to take a longer break from booze once we see the benefits!)
How can we stay safe when it comes to alcohol and cyclobenzaprine? Here are a few tips to start with.
With these tips, you can stay safe when it comes to cyclobenzaprine and alcohol while helping your muscles heal. We wish you a speedy recovery!
For some extra motivation, keep in mind that it’s not just your muscles that will reap the rewards — going easy on the booze and taking care of your physical health will also bring you closer to being the healthiest and happiest version of yourself.
We can think of our habits themselves as a sort of “mental muscle” we can exercise, leading us to form healthy habits over time. As Monjyoti Bhattacharyya writes in A Relentless Pursuit of the Truth: A Philosophical Guide to Living a Life of Fulfillment and Meaning, “We become muscular at whatever we are repeatedly exposed to. Same is true for all the unconscious habits we develop.” Let’s take care of our muscles — both the physical kind and the metaphorical muscles of habit that help us transform our lives and become the best versions of ourselves.
If you’ve ever gotten a painful muscle spasm, you know it’s no joke. It can jolt you out of sleep or strike during the day, as you go about your business and are suddenly stopped in your tracks by what feels like a pair of tyrannosaurus jaws chomping into your muscles. Those moments can fill you with panic as you try to remember the tricks you’ve heard from your grandmother or read about online. Fill a bathtub with hot water and soak your foot in it? Stand on your heel and bend your toes back? Ugh! Nothing seems to help.
When our muscle pain and spasms become a regular thing, we might end up taking medication such as a muscle relaxant. Cyclobenzaprine (known by the brand name Flexeril) is often prescribed to alleviate spasms related to all sorts of musculoskeletal conditions. But what about cyclobenzaprine and alcohol — is it okay to mix the two? Can you drink on muscle relaxers in general, and what are the possible dangers? Let’s find out!

According to NIH, cyclobenzaprine, a muscle relaxant, is prescribed to help relieve pain from muscle spasms caused by different musculoskeletal conditions. It’s usually not a stand-alone measure, and is used in combination with rest, physical therapy exercises, and other techniques that help relax muscles, quiet pain, and relieve discomfort caused by strains, sprains, and various types of muscle injuries.
Muscle relaxants might sound very modern, but they’re actually nothing new! The earliest “muscle relaxants” were actually poison-tipped arrows used as weapons by peoples in the Amazon Basin in South America. The European explorers picked up on their potential medical applications and used them in early experiments that eventually led to the development of cyclobenzaprine and its many pharmacological cousins. And don’t worry — the variety doled out by the local pharmacy won’t do us any harm, provided we take them as prescribed.
Muscle relaxants work through a few different pathways that all have the same goal — quieting down those overactive signals to prevent painful spasms and muscle hyperactivity. Let’s see what their main mechanisms are and where cyclobenzaprine fits in.
The full list of options for muscle ailments is much longer, but these are the highlights. There are many individual factors that come into play when choosing the right option, and our physician can give us the best idea of which course of treatment is right for us.
Can you drink on muscle relaxers? And more specifically, can you drink alcohol with cyclobenzaprine? As it turns out, it’s not a good idea for several reasons.
Both of the main muscle relaxer types (antispastics and antispasmodics) can have negative interactions with alcohol. Most of the dangers center on amplified side effects (especially sedation). For a deeper look at the dangers of mixing alcohol and muscle relaxants in general, check out “Muscle Relaxers and Alcohol: A Dangerous Mix.” For now, let’s take a closer look at cyclobenzaprine and alcohol in particular.
One of the main reasons it’s best to avoid the combo has to do with some gnarly side effects we can end up with as a result. According to NIH, cyclobenzaprine comes with some fairly typical ones, as well as potentially dangerous ones. None of them mix too well with booze.
This last set of effects is the main reason mixing the two is not recommended, since it increases the chances of having a dangerous fall or another accident. Besides, the sedation could land us in dangerous waters if our heart and breathing rate slows down too much, causing respiratory depression.
Because of this, driving or operating machinery is out of the question (even if we’re below the legal alcohol limit). It’s important to stay safe and protect others around us!
Another reason why cyclobenzaprine and alcohol are a dangerous combination? Our liver probably won’t be too happy with the mix. Both substances are processed by the liver, which is already in danger of becoming overwhelmed by alcohol alone. Adding another burdensome to-do list item to its task list is asking for trouble.
Studies show that mixing alcohol and medications that are processed by the liver leads to a less-than-favorable metabolic fallout. Specifically, we end up with elevated levels of certain enzymes. The result? Higher fat deposits and overall stress that can eventually result in liver disease and other complications.
Alcohol’s effect on the heart could also put us at risk if we’re taking cyclobenzaprine. Booze is notorious for messing with our blood pressure, decreasing it at first through vasodilation (the widening of blood vessels) before leading to a rebound effect. It also causes potentially dangerous arrhythmias and increases our heart rate. Over time, these disruptions could even lead to cardiomyopathy — a serious form of heart disease. (For more information take a look at “How Does Alcohol Affect the Heart?”).
Moreover, alcohol’s effect on muscles can be counterproductive during the healing process. Science shows that alcohol contributes to muscle degeneration, gets in the way of muscle-building, and even leads to muscle atrophy in the long run.
Finally, there’s the matter of dependency. As we know, alcohol can be notoriously addictive since it affects the brain’s levels of dopamine, a “reward” neurotransmitter involved in pleasure-seeking behavior. Dopamine gets released through activities that make us feel good (delicious food, good company, a date that ends well — you get the picture). However, substances like alcohol cause an unnatural flood of dopamine that the brain eventually gets used to and comes to expect, leading us to become more and more dependent on that weekly (or nightly) drink.
Muscle relaxers affect our cognition a bit differently but can play a role in this process. By affecting our nervous system, they lower our “cognitive defenses,” making it more likely we’ll jump into certain situations or make decisions without thinking. Our inhibitions might be lower, and we might end up drinking more as a result, paving the way for potential problems in the future.

Cyclobenzaprine has a half-life of about 18 hours, which means that within 18 hours, half of it is no longer in our body. (It’s usually taken 3 times a day and is meant for short-term use — 2 or 3 weeks at most). Doctors generally recommend waiting at least 48 hours before drinking. (Of course, we might want to take a longer break from booze once we see the benefits!)
How can we stay safe when it comes to alcohol and cyclobenzaprine? Here are a few tips to start with.
With these tips, you can stay safe when it comes to cyclobenzaprine and alcohol while helping your muscles heal. We wish you a speedy recovery!
For some extra motivation, keep in mind that it’s not just your muscles that will reap the rewards — going easy on the booze and taking care of your physical health will also bring you closer to being the healthiest and happiest version of yourself.
We can think of our habits themselves as a sort of “mental muscle” we can exercise, leading us to form healthy habits over time. As Monjyoti Bhattacharyya writes in A Relentless Pursuit of the Truth: A Philosophical Guide to Living a Life of Fulfillment and Meaning, “We become muscular at whatever we are repeatedly exposed to. Same is true for all the unconscious habits we develop.” Let’s take care of our muscles — both the physical kind and the metaphorical muscles of habit that help us transform our lives and become the best versions of ourselves.

Alcohol and Mounjaro don’t interact directly but mixing the two is still risky. Check out our latest blog for more info on why drinking on Mounjaro isn’t recommended.
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually, with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet hundreds of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
Finding information on whether it’s okay to drink alcohol while on Mounjaro can be a bit like climbing Mt. Kilimanjaro — it’s not easy. While not exactly like climbing a 19,000 ft. mountain, the ambiguous guidance on mixing alcohol and Mounjaro can make our decision on whether to drink or not a bit more muddled than it needs to be.
While the label may state no direct interactions between alcohol and Mounjaro, alcohol’s indirect effects on the medication can open the floodgates to a host of different complications. Let’s get to the bottom of how Mounjaro and alcohol interact to understand why drinking on Mounjaro may not be a good idea.

Mounjaro, the brand name for tirzepatide, is a relatively new treatment for type 2 diabetes approved by the Federal Drug Administration (FDA). It is a weekly injection that is used to help manage blood sugar levels and lower the risk of common complications that are associated with diabetes. Mounjaro dosages range from 2.5-15 mg/0.5 mL with the starting dosage typically at 2.5 and increasing as needed.
The drug is categorized as a dual-agonist that stimulates two different hormones — glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptors. GIP receptors promote the production of insulin and increase insulin sensitivity. GLP-1 receptors also stimulate the production of insulin and reduce elevated blood glucose. By increasing the production of GIP and GLP-1, Mounjaro helps treat type 2 diabetes by regulating blood sugar and decreasing the risk of diabetes-related complications.
Like other diabetes treatments, Mounjaro has also been studied and tested for its effectiveness in weight loss. How does a type 2 diabetes treatment aid in weight loss?
While Mounjaro and other popular medications such as Ozempic and Trulicity originated as diabetes treatments, they’ve also more recently been looked at as a weight loss treatment for clinical obesity due to their mechanisms.
GLP-1 receptor agonists like Ozempic and Trulicity help with weight loss by regulating blood sugar and delaying gastric emptying. Research shows that Mounjaro, which has a dual GLP-1/GIP mechanism, promises even greater effectiveness. GIP stimulates satiety in our hypothalamus which signals to our brain that we are full. It also enhances the function of GLP-1, and together they increase insulin production, decrease appetite, and improve insulin sensitivity — all contributing to weight loss.
Mounjaro was recently FDA-approved as a weight loss treatment for those who are obese, overweight, and also have weight-related medical conditions. The weight loss treatment is produced by Eli Lilly under the new name Zepbound. The dosages for Zepbound mirror Mounjaro, starting at 2.5 mg and increasing after 4 weeks if needed. As the first weight loss drug of its kind with its dual mechanism, interest has skyrocketed — creating a shortage. This prompted the company to release a statement strongly discouraging off-label use of the drug. If we do happen to be prescribed Mounjaro for type 2 diabetes or Zepbound for weight loss, we may be looking to get the best use out of it (as it’s hard to get our hands on it). Could alcohol affect the medication?
Drug interactions refer to changes in the mechanism of a drug due to factors such as foods, drinks, or other drugs. Since alcohol is a drug, it interacts with many prescription and over-the-counter medications.
Mounjaro and alcohol don’t have any direct interactions. However, this doesn’t mean that alcohol won’t negatively affect Mounjaro. It only confirms that the mechanism of Mounjaro on our body will continue to work in the same way even when alcohol is introduced into our system. That being said, is it a good idea to drink?
Drinking on Mounjaro is not recommended. Although there aren’t any direct interactions between Mounjaro and alcohol, drinking can still cause adverse effects and increase the risk of complications.
Alcohol has significant effects on many systems in our body, which disrupt key factors that Mounjaro targets. These may include factors such as blood sugar, appetite, insulin, and more. Drinking isn’t recommended while taking Mounjaro, but what about Zepbound (Mounjaro used for weight loss)?
Mixing alcohol and Mounjaro may not cause immediate dangers to our health like other direct drug interactions. However, it opens the door to adverse effects and increased complications that include the following:
Alcohol is a complex drug that can cause negative impacts, even without direct interactions. Let’s explore some ways we can approach alcohol more mindfully and safely while on Mounjaro.

Drinking while taking Mounjaro isn’t recommended, but if we do choose to consume alcohol, safe drinking practices can help limit the potential consequences. Six practices we can implement to navigate drinking while taking Mounjaro more safely include the following:
1. Consult a Doctor
Alcohol can affect us differently due to individual differences. Consulting with a physician provides us with more detailed guidance focused on our individual needs.
2. Know Limits
A “safe” amount of alcohol when taking Mounjaro isn’t able to be determined, but understanding our individual limits helps us avoid excessive alcohol consumption that can negatively affect our weight, blood sugar, or overall health.
3. Quit/Cut Back
Quitting or cutting back on alcohol removes or limits the negative effects that it may cause. This can improve different aspects of our life including our health, mental health, and social well-being.
4. Manage Blood Sugar
Keeping track and managing our blood sugar helps us avoid potential adverse effects. Since hypoglycemia is a common side effect of Mounjaro and drinking alcohol, it's even more crucial to monitor our blood sugar levels to ensure our safety.
5. Healthy Lifestyle
Following a healthy lifestyle through eating balanced meals and staying active supports the mechanisms of Mounjaro and helps to improve our overall well-being. It sets us up for the best chance to recover from the toxins in alcohol and fight against the conditions that Mounjaro aims to treat.
6. Seek Support
Managing health conditions and/or working through an unhealthy relationship with alcohol isn’t easy. Different types of social support can help us overcome challenges and remind us that we aren’t alone.
These mindful actions can reduce the indirect interactions between alcohol and Mounjaro, but the safest bet is to remove the risk entirely by replacing alcohol with alcohol-free alternatives.
Mounjaro is a newer medication used to treat type 2 diabetes and/or obesity. The first drug of its kind with its unique dual mechanism, Mounjaro is difficult to get a hold of. Understanding the risks associated with drinking on Mounjaro including worsened side effects, decreased effectiveness, and long-term health conditions helps us get the most out of the medication and keep us safe. Quitting or cutting back while on Mounjaro promotes a healthier tomorrow!
Finding information on whether it’s okay to drink alcohol while on Mounjaro can be a bit like climbing Mt. Kilimanjaro — it’s not easy. While not exactly like climbing a 19,000 ft. mountain, the ambiguous guidance on mixing alcohol and Mounjaro can make our decision on whether to drink or not a bit more muddled than it needs to be.
While the label may state no direct interactions between alcohol and Mounjaro, alcohol’s indirect effects on the medication can open the floodgates to a host of different complications. Let’s get to the bottom of how Mounjaro and alcohol interact to understand why drinking on Mounjaro may not be a good idea.

Mounjaro, the brand name for tirzepatide, is a relatively new treatment for type 2 diabetes approved by the Federal Drug Administration (FDA). It is a weekly injection that is used to help manage blood sugar levels and lower the risk of common complications that are associated with diabetes. Mounjaro dosages range from 2.5-15 mg/0.5 mL with the starting dosage typically at 2.5 and increasing as needed.
The drug is categorized as a dual-agonist that stimulates two different hormones — glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptors. GIP receptors promote the production of insulin and increase insulin sensitivity. GLP-1 receptors also stimulate the production of insulin and reduce elevated blood glucose. By increasing the production of GIP and GLP-1, Mounjaro helps treat type 2 diabetes by regulating blood sugar and decreasing the risk of diabetes-related complications.
Like other diabetes treatments, Mounjaro has also been studied and tested for its effectiveness in weight loss. How does a type 2 diabetes treatment aid in weight loss?
While Mounjaro and other popular medications such as Ozempic and Trulicity originated as diabetes treatments, they’ve also more recently been looked at as a weight loss treatment for clinical obesity due to their mechanisms.
GLP-1 receptor agonists like Ozempic and Trulicity help with weight loss by regulating blood sugar and delaying gastric emptying. Research shows that Mounjaro, which has a dual GLP-1/GIP mechanism, promises even greater effectiveness. GIP stimulates satiety in our hypothalamus which signals to our brain that we are full. It also enhances the function of GLP-1, and together they increase insulin production, decrease appetite, and improve insulin sensitivity — all contributing to weight loss.
Mounjaro was recently FDA-approved as a weight loss treatment for those who are obese, overweight, and also have weight-related medical conditions. The weight loss treatment is produced by Eli Lilly under the new name Zepbound. The dosages for Zepbound mirror Mounjaro, starting at 2.5 mg and increasing after 4 weeks if needed. As the first weight loss drug of its kind with its dual mechanism, interest has skyrocketed — creating a shortage. This prompted the company to release a statement strongly discouraging off-label use of the drug. If we do happen to be prescribed Mounjaro for type 2 diabetes or Zepbound for weight loss, we may be looking to get the best use out of it (as it’s hard to get our hands on it). Could alcohol affect the medication?
Drug interactions refer to changes in the mechanism of a drug due to factors such as foods, drinks, or other drugs. Since alcohol is a drug, it interacts with many prescription and over-the-counter medications.
Mounjaro and alcohol don’t have any direct interactions. However, this doesn’t mean that alcohol won’t negatively affect Mounjaro. It only confirms that the mechanism of Mounjaro on our body will continue to work in the same way even when alcohol is introduced into our system. That being said, is it a good idea to drink?
Drinking on Mounjaro is not recommended. Although there aren’t any direct interactions between Mounjaro and alcohol, drinking can still cause adverse effects and increase the risk of complications.
Alcohol has significant effects on many systems in our body, which disrupt key factors that Mounjaro targets. These may include factors such as blood sugar, appetite, insulin, and more. Drinking isn’t recommended while taking Mounjaro, but what about Zepbound (Mounjaro used for weight loss)?
Mixing alcohol and Mounjaro may not cause immediate dangers to our health like other direct drug interactions. However, it opens the door to adverse effects and increased complications that include the following:
Alcohol is a complex drug that can cause negative impacts, even without direct interactions. Let’s explore some ways we can approach alcohol more mindfully and safely while on Mounjaro.

Drinking while taking Mounjaro isn’t recommended, but if we do choose to consume alcohol, safe drinking practices can help limit the potential consequences. Six practices we can implement to navigate drinking while taking Mounjaro more safely include the following:
1. Consult a Doctor
Alcohol can affect us differently due to individual differences. Consulting with a physician provides us with more detailed guidance focused on our individual needs.
2. Know Limits
A “safe” amount of alcohol when taking Mounjaro isn’t able to be determined, but understanding our individual limits helps us avoid excessive alcohol consumption that can negatively affect our weight, blood sugar, or overall health.
3. Quit/Cut Back
Quitting or cutting back on alcohol removes or limits the negative effects that it may cause. This can improve different aspects of our life including our health, mental health, and social well-being.
4. Manage Blood Sugar
Keeping track and managing our blood sugar helps us avoid potential adverse effects. Since hypoglycemia is a common side effect of Mounjaro and drinking alcohol, it's even more crucial to monitor our blood sugar levels to ensure our safety.
5. Healthy Lifestyle
Following a healthy lifestyle through eating balanced meals and staying active supports the mechanisms of Mounjaro and helps to improve our overall well-being. It sets us up for the best chance to recover from the toxins in alcohol and fight against the conditions that Mounjaro aims to treat.
6. Seek Support
Managing health conditions and/or working through an unhealthy relationship with alcohol isn’t easy. Different types of social support can help us overcome challenges and remind us that we aren’t alone.
These mindful actions can reduce the indirect interactions between alcohol and Mounjaro, but the safest bet is to remove the risk entirely by replacing alcohol with alcohol-free alternatives.
Mounjaro is a newer medication used to treat type 2 diabetes and/or obesity. The first drug of its kind with its unique dual mechanism, Mounjaro is difficult to get a hold of. Understanding the risks associated with drinking on Mounjaro including worsened side effects, decreased effectiveness, and long-term health conditions helps us get the most out of the medication and keep us safe. Quitting or cutting back while on Mounjaro promotes a healthier tomorrow!

Ever wondered if Cialis interacts with alcohol? Find out in our latest blog, where we uncover everything you need to know about mixing these two popular date-night companions. The answers might surprise you!
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually, with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet hundreds of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
It’s date night, you’ve had a couple of glasses of wine, and now the bedroom is calling your names. But wait. You got a new prescription for Cialis earlier this week. Is it safe to take it after drinking wine? Should you take your chances or hold off?
Hopefully, you’re reading this before you find yourself frantically pacing and Googling answers in the bathroom. Fortunately, you’re not the only one who has ever asked this question, and we have answers. In this blog, we’ll cover all you need to know about the interactions between Cialis and alcohol.

Cialis is a brand name of the phosphodiesterase-5 inhibitor (PDE5) known as tadalafil. Much like its cousin, Viagra (sildenafil), it’s mainly used to treat erectile dysfunction (ED). It works by boosting the chemicals the body naturally produces during arousal. The main difference is that Cialis stays in the body longer (up to 36 hours) than Viagra.
The general guideline is to take Cialis at least 30 minutes before sexual activity, but not more than once daily. It’s generally proven safe and effective, but it may come with unwanted, mood-killing side effects like headache, indigestion, back pain, muscle pain, flushing, or even a stuffy nose. If it’s any encouragement, the muscle aches usually come 12-24 hours after taking it.
The most important side effect to be aware of is the tendency for Cialis to lower your blood pressure, which is particularly important where alcohol is involved.
We’ve all seen what happens when someone throws back a few too many drinks. Word vomit, actual vomit, and impromptu table dances are some of the most common consequences (according to Hollywood, anyway). Drunk driving accidents are among the more tragic consequences. How do a few drinks lead to such chaos?
When ethanol, the main intoxicating ingredient in alcohol, enters the bloodstream, it affects nearly every vital system and organ. At first, we get the familiar “buzz” that helps us let loose and relax, but if we keep drinking beyond that, chaos ensues. It fogs our central nervous system, leading to impaired coordination and judgment. It overwhelms our liver, affecting metabolism and long-term liver health. It disrupts our hormones, our heart, and our immune system. And most people don’t realize it, but it also wreaks havoc on our reproductive system, which we’ll get into later.
So what happens when you take Cialis before or after drinking alcohol? How do tadalafil and alcohol interact?
As a general rule, keep in mind that ethanol can affect any drug. It can affect metabolism and absorption, increase side effects, and more. When it comes to tadalafil specifically, there are a couple of interactions to be aware of:
While neither of these interactions is necessarily life-threatening, it’s important to be aware of and plan for them to avoid further complications. Now, let’s get to the burning question.

If you have a clean bill of health, and Cialis is the only drug you’re taking, sipping on a glass of wine at dinner likely won’t cause any problems. Throwing back whiskey shots on an empty stomach, however, could be a different story with or without Cialis in the picture. Here are some general guidelines to help you plan a safe night out or in.
If you have a drink or two before or after taking Cialis, it probably won’t cause any problems. There is no known interaction (like pain pills and alcohol) that would make the mixture inherently dangerous.
If you drink more than two, it might decrease the effectiveness of Cialis and/or increase the likelihood of its side effects. Either way, it could definitely put a damper on date night.
If you drink five or more drinks within two hours, (classified as binge drinking), it could lead to several serious health problems and poor decisions (and possibly fewer date nights in the future). When combined with Cialis, the main concern with binge drinking is a sudden drop in blood pressure, known as orthostatic hypotension.
When it comes to alcohol, less is always safer, especially when other medications are involved.
If mixing Cialis and alcohol is a concern for you, it might be worth exploring how alcohol affects our sexual health. Research shows that persistent alcohol use is directly linked to sexual dysfunction, ranging from decreased libido to physical difficulties. If that’s the case, could quitting alcohol help resolve the need for Cialis? Let’s find out.
There are many different causes of ED, from illness to medications to emotional issues. Whatever the reason, alcohol can make matters worse.
To sum up, while we can’t say that quitting or even cutting back on alcohol will cure ED, we can confidently say it will help.
Fortunately, there are things you can do to stay safe while your mind adjusts to a new way of thinking.
Above all, be sure to repair and/or nourish your relationships, whether they be sexual or not. Stronger relationships lead to greater satisfaction and well-being in all areas of your life.
While mixing alcohol and Cialis isn’t inherently life-threatening, it could lead to dangerous blood pressure fluctuations. Furthermore, alcohol could counteract the effects of Cialis. If you’re looking to improve your sexual health, nourish your body with good sleep and nutrition, and nurture the relationships that mean the most to you. And as always, pay close attention to new symptoms and seek medical advice when needed. We’re here to help and cheer you on!
It’s date night, you’ve had a couple of glasses of wine, and now the bedroom is calling your names. But wait. You got a new prescription for Cialis earlier this week. Is it safe to take it after drinking wine? Should you take your chances or hold off?
Hopefully, you’re reading this before you find yourself frantically pacing and Googling answers in the bathroom. Fortunately, you’re not the only one who has ever asked this question, and we have answers. In this blog, we’ll cover all you need to know about the interactions between Cialis and alcohol.

Cialis is a brand name of the phosphodiesterase-5 inhibitor (PDE5) known as tadalafil. Much like its cousin, Viagra (sildenafil), it’s mainly used to treat erectile dysfunction (ED). It works by boosting the chemicals the body naturally produces during arousal. The main difference is that Cialis stays in the body longer (up to 36 hours) than Viagra.
The general guideline is to take Cialis at least 30 minutes before sexual activity, but not more than once daily. It’s generally proven safe and effective, but it may come with unwanted, mood-killing side effects like headache, indigestion, back pain, muscle pain, flushing, or even a stuffy nose. If it’s any encouragement, the muscle aches usually come 12-24 hours after taking it.
The most important side effect to be aware of is the tendency for Cialis to lower your blood pressure, which is particularly important where alcohol is involved.
We’ve all seen what happens when someone throws back a few too many drinks. Word vomit, actual vomit, and impromptu table dances are some of the most common consequences (according to Hollywood, anyway). Drunk driving accidents are among the more tragic consequences. How do a few drinks lead to such chaos?
When ethanol, the main intoxicating ingredient in alcohol, enters the bloodstream, it affects nearly every vital system and organ. At first, we get the familiar “buzz” that helps us let loose and relax, but if we keep drinking beyond that, chaos ensues. It fogs our central nervous system, leading to impaired coordination and judgment. It overwhelms our liver, affecting metabolism and long-term liver health. It disrupts our hormones, our heart, and our immune system. And most people don’t realize it, but it also wreaks havoc on our reproductive system, which we’ll get into later.
So what happens when you take Cialis before or after drinking alcohol? How do tadalafil and alcohol interact?
As a general rule, keep in mind that ethanol can affect any drug. It can affect metabolism and absorption, increase side effects, and more. When it comes to tadalafil specifically, there are a couple of interactions to be aware of:
While neither of these interactions is necessarily life-threatening, it’s important to be aware of and plan for them to avoid further complications. Now, let’s get to the burning question.

If you have a clean bill of health, and Cialis is the only drug you’re taking, sipping on a glass of wine at dinner likely won’t cause any problems. Throwing back whiskey shots on an empty stomach, however, could be a different story with or without Cialis in the picture. Here are some general guidelines to help you plan a safe night out or in.
If you have a drink or two before or after taking Cialis, it probably won’t cause any problems. There is no known interaction (like pain pills and alcohol) that would make the mixture inherently dangerous.
If you drink more than two, it might decrease the effectiveness of Cialis and/or increase the likelihood of its side effects. Either way, it could definitely put a damper on date night.
If you drink five or more drinks within two hours, (classified as binge drinking), it could lead to several serious health problems and poor decisions (and possibly fewer date nights in the future). When combined with Cialis, the main concern with binge drinking is a sudden drop in blood pressure, known as orthostatic hypotension.
When it comes to alcohol, less is always safer, especially when other medications are involved.
If mixing Cialis and alcohol is a concern for you, it might be worth exploring how alcohol affects our sexual health. Research shows that persistent alcohol use is directly linked to sexual dysfunction, ranging from decreased libido to physical difficulties. If that’s the case, could quitting alcohol help resolve the need for Cialis? Let’s find out.
There are many different causes of ED, from illness to medications to emotional issues. Whatever the reason, alcohol can make matters worse.
To sum up, while we can’t say that quitting or even cutting back on alcohol will cure ED, we can confidently say it will help.
Fortunately, there are things you can do to stay safe while your mind adjusts to a new way of thinking.
Above all, be sure to repair and/or nourish your relationships, whether they be sexual or not. Stronger relationships lead to greater satisfaction and well-being in all areas of your life.
While mixing alcohol and Cialis isn’t inherently life-threatening, it could lead to dangerous blood pressure fluctuations. Furthermore, alcohol could counteract the effects of Cialis. If you’re looking to improve your sexual health, nourish your body with good sleep and nutrition, and nurture the relationships that mean the most to you. And as always, pay close attention to new symptoms and seek medical advice when needed. We’re here to help and cheer you on!

Can you drink alcohol with Paxlovid? As it turns out, the mix could be risky and might set you up for a longer recovery from COVID. Find out more in our latest blog!
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually, with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet hundreds of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
Back in December 2019 in the city of Wuhan, China, a few patients came down with an “atypical pneumonia-like illness that does not respond well to standard treatments.” The rest, as we know it, is history.
The COVID pandemic will live on in history books as a major world disaster, but for most of us, it was an everyday reality. Caused by the coronavirus SARS-CoV-2 that triggered severe respiratory symptoms (and was deadly to vulnerable populations), the pandemic turned our lives upside down, leading to lockdowns, social distancing, mask-wearing, and rigorous hygiene practices.
We stocked up on toilet paper and Lysol wipes, cleared out grocery store shelves of everything from canned soup to asparagus, and waited anxiously for updates from officials who, for a long time, knew as little as the rest of us about the situation.
In all the chaos and confusion, a lot of people turned to booze to deal with the stress of it all. When Paxlovid came out, it left many wondering: can you drink alcohol while taking Paxlovid? In this article, we’ll explore the link between Paxlovid, alcohol, and liver and kidney problems.

“If it’s COVID, Paxlovid.” This catchy slogan aired to promote the new “wonder drug” said to diminish COVID symptoms. It wasn’t a cure, but it was pretty close. With Paxlovid, the outlook for COVID patients changed considerably. They could ride it out at home with enough energy to play video games in the living room or type away on a laptop. They were still sick, but they were getting better.
Paxlovid combines 2 medicines — nirmatrelvir and ritonavir — to throw a wrench in the virus’s attack on the body. Nirmatrelvir stops it from growing and spreading while keeping its levels to a minimum by blocking a specific enzyme, robbing the virus of its ability to multiply. The second member of the antiviral duo is there for support, keeping nirmatrelvir from getting metabolized by the liver, giving it enough time to do its job.
Paxlovid is for those at risk of developing severe COVID symptoms. And while many of us might say, “That’s not me, I’m healthy,” at least 75% of U.S. adults have at least one risk factor that puts them in this category. Here are the most common ones:
According to the CDC, certain life circumstances also put us in a higher risk category. For example, where we live or work and access to healthcare can make a difference.
How does it interact with alcohol? Let’s explore what happens when we mix alcohol and Paxlovid.
For one thing, alcohol can amp up many of the side effects of Paxlovid. And when we’re already battling an infection that’s uncomfortable (to say the least), extra obstacles are the last thing we need. Let’s dig deeper into what we can expect from the Paxlovid-alcohol combo.
All in all, the picture that emerges is clear: if it’s COVID, Paxlovid (but not booze).
Paxlovid is cleared by the kidneys, but it can also cause liver strain in people who are dealing with serious liver disease or are on dialysis. For everyone else, the FDA cautions to be on the lookout for signs of liver problems, such as appetite loss, jaundice (a yellow tinge to the skin and the whites of the eyes), dark urine, itchy skin, and stomach issues.
Adding alcohol to the mix can only make matters worse. It’s notoriously rough on the liver, which is at the frontlines of processing alcohol. Since nirmatrelvir competes with alcohol for metabolism, our liver can easily be overworked. But the kidneys aren’t immune to the effects either: in fact, heavy drinking is linked to kidney disease.

Moreover, alcohol can do a number on our immune system and lungs, which doesn’t help matters when it comes to fighting off a deadly respiratory virus.
Want to learn more about how alcohol affects our immunity? Check out “Alcohol's Impact on the Immune System.”
Moreover, there’s the issue of “Long COVID” to consider. As if “regular” COVID wasn't enough, this “enhanced” version started rearing its ugly head as many of us found ourselves feeling drained, fatigued, and emotionally unwell for weeks or even months battling through the acute infection.
This dreaded lengthy stay of the virus was precisely what Paxlovid was meant to address. But if we add alcohol to the picture, things can get a bit more complicated.
As we can see, alcohol is likely to stand in the way of our recovery, and there’s no point in making Long COVID last even longer.
As it turns out, however, the relationship between alcohol and COVID goes beyond the Paxlovid-alcohol interactions. For many of us, COVID itself became (on top of everything else) an unexpected trigger for drinking. And it’s not hard to see why.
Some of us were cooped up indoors with rambunctious toddlers, moody teenagers, and spouses (who, lovely as they might be, are usually not in our faces 24/7). Others had the opposite dilemma, finding themselves isolated for weeks that turned into months. If we happened to see a neighbor on one of our toilet paper runs to the store, we probably wouldn’t have recognized them in their face mask from six feet away.
At the same time, home delivery of everything from the aforementioned toilet paper to, yes, alcohol, skyrocketed. The result? Our drinking habits did too.
Statistics around the country back this up. According to the NIH, a rise in drinking during times of crisis is common, as shown by data after the 1993 World Trade Center bombing, Hurricane Katrina, and 9/11. During the first year of the pandemic, alcohol sales saw the largest increase in half a century (around 3%). Many studies showed that about a quarter of the population drank more than before due to the stress and uncertainty of the situation.
Unfortunately, this meant that hospitalizations and deaths from alcohol misuse added to the already soaring casualty rates from COVID. According to George F. Koob, director of the National Institute on Alcohol Abuse and Alcoholism, the first two years brought about a 38% increase in death certificates listing alcohol as a contributing cause, with the largest increase affecting people in the 25-44 age bracket.
Alcohol-related injuries became more frequent and the demand for liver transplants grew, with record-breaking numbers of patients under the age of 30. Regrettably, many ended up waiting in vain: deaths from liver disease went up by more than 22% during these already difficult years. (To learn more about the effects of COVID on alcohol use, take a look at “How Has Alcohol Use Changed After the COVID-19 Pandemic?”)
So how can we stay safe when we’re taking Paxlovid? And how can we avoid the deeper pitfalls of alcohol misuse triggered by the pandemic itself? Here are some tips to consider:
And remember, there are millions of others around the world who have been where you are and know how you feel. Connect to them and swap stories and advice through the Reframe 24/7 Forum! The journey is more fun and more rewarding when you can share it with others like you.
In the end, the pandemic made us rethink a lot of our daily habits. And if alcohol is one of them, so be it — let’s take this opportunity to revamp our relationship with it to be healthier, happier, and COVID-free.
Back in December 2019 in the city of Wuhan, China, a few patients came down with an “atypical pneumonia-like illness that does not respond well to standard treatments.” The rest, as we know it, is history.
The COVID pandemic will live on in history books as a major world disaster, but for most of us, it was an everyday reality. Caused by the coronavirus SARS-CoV-2 that triggered severe respiratory symptoms (and was deadly to vulnerable populations), the pandemic turned our lives upside down, leading to lockdowns, social distancing, mask-wearing, and rigorous hygiene practices.
We stocked up on toilet paper and Lysol wipes, cleared out grocery store shelves of everything from canned soup to asparagus, and waited anxiously for updates from officials who, for a long time, knew as little as the rest of us about the situation.
In all the chaos and confusion, a lot of people turned to booze to deal with the stress of it all. When Paxlovid came out, it left many wondering: can you drink alcohol while taking Paxlovid? In this article, we’ll explore the link between Paxlovid, alcohol, and liver and kidney problems.

“If it’s COVID, Paxlovid.” This catchy slogan aired to promote the new “wonder drug” said to diminish COVID symptoms. It wasn’t a cure, but it was pretty close. With Paxlovid, the outlook for COVID patients changed considerably. They could ride it out at home with enough energy to play video games in the living room or type away on a laptop. They were still sick, but they were getting better.
Paxlovid combines 2 medicines — nirmatrelvir and ritonavir — to throw a wrench in the virus’s attack on the body. Nirmatrelvir stops it from growing and spreading while keeping its levels to a minimum by blocking a specific enzyme, robbing the virus of its ability to multiply. The second member of the antiviral duo is there for support, keeping nirmatrelvir from getting metabolized by the liver, giving it enough time to do its job.
Paxlovid is for those at risk of developing severe COVID symptoms. And while many of us might say, “That’s not me, I’m healthy,” at least 75% of U.S. adults have at least one risk factor that puts them in this category. Here are the most common ones:
According to the CDC, certain life circumstances also put us in a higher risk category. For example, where we live or work and access to healthcare can make a difference.
How does it interact with alcohol? Let’s explore what happens when we mix alcohol and Paxlovid.
For one thing, alcohol can amp up many of the side effects of Paxlovid. And when we’re already battling an infection that’s uncomfortable (to say the least), extra obstacles are the last thing we need. Let’s dig deeper into what we can expect from the Paxlovid-alcohol combo.
All in all, the picture that emerges is clear: if it’s COVID, Paxlovid (but not booze).
Paxlovid is cleared by the kidneys, but it can also cause liver strain in people who are dealing with serious liver disease or are on dialysis. For everyone else, the FDA cautions to be on the lookout for signs of liver problems, such as appetite loss, jaundice (a yellow tinge to the skin and the whites of the eyes), dark urine, itchy skin, and stomach issues.
Adding alcohol to the mix can only make matters worse. It’s notoriously rough on the liver, which is at the frontlines of processing alcohol. Since nirmatrelvir competes with alcohol for metabolism, our liver can easily be overworked. But the kidneys aren’t immune to the effects either: in fact, heavy drinking is linked to kidney disease.

Moreover, alcohol can do a number on our immune system and lungs, which doesn’t help matters when it comes to fighting off a deadly respiratory virus.
Want to learn more about how alcohol affects our immunity? Check out “Alcohol's Impact on the Immune System.”
Moreover, there’s the issue of “Long COVID” to consider. As if “regular” COVID wasn't enough, this “enhanced” version started rearing its ugly head as many of us found ourselves feeling drained, fatigued, and emotionally unwell for weeks or even months battling through the acute infection.
This dreaded lengthy stay of the virus was precisely what Paxlovid was meant to address. But if we add alcohol to the picture, things can get a bit more complicated.
As we can see, alcohol is likely to stand in the way of our recovery, and there’s no point in making Long COVID last even longer.
As it turns out, however, the relationship between alcohol and COVID goes beyond the Paxlovid-alcohol interactions. For many of us, COVID itself became (on top of everything else) an unexpected trigger for drinking. And it’s not hard to see why.
Some of us were cooped up indoors with rambunctious toddlers, moody teenagers, and spouses (who, lovely as they might be, are usually not in our faces 24/7). Others had the opposite dilemma, finding themselves isolated for weeks that turned into months. If we happened to see a neighbor on one of our toilet paper runs to the store, we probably wouldn’t have recognized them in their face mask from six feet away.
At the same time, home delivery of everything from the aforementioned toilet paper to, yes, alcohol, skyrocketed. The result? Our drinking habits did too.
Statistics around the country back this up. According to the NIH, a rise in drinking during times of crisis is common, as shown by data after the 1993 World Trade Center bombing, Hurricane Katrina, and 9/11. During the first year of the pandemic, alcohol sales saw the largest increase in half a century (around 3%). Many studies showed that about a quarter of the population drank more than before due to the stress and uncertainty of the situation.
Unfortunately, this meant that hospitalizations and deaths from alcohol misuse added to the already soaring casualty rates from COVID. According to George F. Koob, director of the National Institute on Alcohol Abuse and Alcoholism, the first two years brought about a 38% increase in death certificates listing alcohol as a contributing cause, with the largest increase affecting people in the 25-44 age bracket.
Alcohol-related injuries became more frequent and the demand for liver transplants grew, with record-breaking numbers of patients under the age of 30. Regrettably, many ended up waiting in vain: deaths from liver disease went up by more than 22% during these already difficult years. (To learn more about the effects of COVID on alcohol use, take a look at “How Has Alcohol Use Changed After the COVID-19 Pandemic?”)
So how can we stay safe when we’re taking Paxlovid? And how can we avoid the deeper pitfalls of alcohol misuse triggered by the pandemic itself? Here are some tips to consider:
And remember, there are millions of others around the world who have been where you are and know how you feel. Connect to them and swap stories and advice through the Reframe 24/7 Forum! The journey is more fun and more rewarding when you can share it with others like you.
In the end, the pandemic made us rethink a lot of our daily habits. And if alcohol is one of them, so be it — let’s take this opportunity to revamp our relationship with it to be healthier, happier, and COVID-free.

Is drinking on Wegovy a bad idea? Between increased side effects and alcohol sabotaging your weight loss efforts, science says it’s risky. Learn more in our latest blog!
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually, with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet hundreds of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
Picture this: you’ve tried it all. You’ve been measuring your yogurt and granola religiously, swinging those kettlebells every morning (watch out for the glass table!), and even made Calorie King your homepage. And yet the scale isn’t budging.
Whatever the reason, these days there are medications that can help get the weight loss process going. A new one that’s been making waves is Wegovy — the brand-name version of semaglutide, which has become one of the go-to meds prescribed for weight loss. But you might be wondering, what about mixing Wegovy and alcohol — can you drink on Wegovy? Or is it a no-go? Let’s find out!

Wegovy was originally developed to treat type 2 diabetes — a condition caused by our body’s inability to use insulin, a hormone that moves glucose (our primary source of energy) from our blood into our cells. According to the CDC, diabetes affects around 38.4 million people in the U.S. — a whopping 11.6% of the U.S. population. Sometimes we can chalk it up to the luck of the genetic draw: one form of diabetes — type 1 — is an inherited autoimmune disease. Type 2 diabetes, on the other hand, develops over time and is the fallout of unhealthy eating habits and a sedentary lifestyle.
And while being overweight isn’t a “prerequisite” for diabetes, obesity and diabetes share some biological features, and benefit from the same treatment.
Wegovy belongs to a class of drugs known as GLP-1 receptor agonists. GLP-1 is a hormone that helps us regulate blood sugar levels and appetite. In its natural form, GLP-1 gets released by the gut after we eat and binds to GLP-1 receptors in the brain and pancreas, triggering insulin release while making us feel full. GLP-1 receptor agonists such as Wegovy step in to do the same: research shows that Wegovy promotes insulin release while making it easier to keep a lid on our snacking habits.
First things first: we might find that taking Wegovy curbs our desire to drink altogether. The reason has to do with the brain. Wegovy works by altering pathways in the hypothalamus — a region that regulates hunger and satiety. As it turns out, it also plays a key role in the reward system that’s at the center of addictive behaviors such as alcohol misuse.
Alcohol hijacks the reward system by artificially boosting dopamine — a neurotransmitter associated with pleasure that’s also involved in motivation and learning. While the reward system evolved to allow us to develop habits necessary for survival — for example, eating or finding a romantic partner — substances such as alcohol trigger dopamine release artificially. That’s what makes it so hard to stop!
Wegovy, in turn, tweaks the reward system pathways in a way that makes alcohol less potent. We don’t get the same “high,” so we’re not as tempted to keep coming back for more. In fact, studies have even shown that Wegovy could be used to curb drinking!
That said, what happens if we do decide to mix alcohol and Wegovy?
We’ve established that our cravings for booze might naturally simmer down when Wegovy is in the mix. But what if they don’t? Can you drink alcohol on Wegovy? Mixing the two could spell trouble for a number of reasons.
If we do mix alcohol and Wegovy, the result isn’t pretty. For one thing, our blood sugar levels could go out of whack. While alcohol increases blood sugar in the long run, the immediate effect is usually a blood sugar drop. Because the body sees alcohol as a poison and prioritizes its metabolism over everything else, it stops releasing glucose — causing a temporary dip in blood sugar.
Because semaglutide lowers our blood sugar as well, we’re in for an all-time low when we combine Wegovy and alcohol. The result? We might feel dizzy, confused, or even pass out.
But that’s not all! Like any medication, Wegovy is not without its side effects.
What are Wegovy side effects with alcohol? Here’s what we might be in store for if we combine the two:
It’s clear that combining Wegovy side effects with alcohol’s impact makes for an unpleasant — and possibly dangerous — combination. Drinking on Wegovy is likely to cause trouble, especially if we overdo it.
Last but certainly not least, here’s one of the most important reasons why alcohol and Wegovy are a problematic pair: booze can sabotage our weight loss efforts, throwing a wrench in the progress we’ve made, and maybe even sending us back to the state that led us to start taking the medication in the first place. Here’s why the two play for opposite teams:
It’s best to steer clear of alcohol while on Wegovy. This not only helps us with our weight loss but promotes a healthier lifestyle all around.

It can feel challenging to navigate the weight loss journey while also trying to drink less. The great news is that the same tools can make both goals easier to reach. Here are some of the most effective ones:
And remember, the Reframe community is here to help you every step of the way. Check out our vibrant 24/7 Forum where others who’ve been in your shoes and know what it’s like are ready to share their stories and advice. We’re rooting for you!
Whether or not we’re taking Wegovy, quitting alcohol will only help our weight loss efforts. Losing weight and reducing alcohol intake both involve being mindful of what we put in our body, and as we adjust our habits, we can look forward to a healthier, more vibrant lifestyle!
Picture this: you’ve tried it all. You’ve been measuring your yogurt and granola religiously, swinging those kettlebells every morning (watch out for the glass table!), and even made Calorie King your homepage. And yet the scale isn’t budging.
Whatever the reason, these days there are medications that can help get the weight loss process going. A new one that’s been making waves is Wegovy — the brand-name version of semaglutide, which has become one of the go-to meds prescribed for weight loss. But you might be wondering, what about mixing Wegovy and alcohol — can you drink on Wegovy? Or is it a no-go? Let’s find out!

Wegovy was originally developed to treat type 2 diabetes — a condition caused by our body’s inability to use insulin, a hormone that moves glucose (our primary source of energy) from our blood into our cells. According to the CDC, diabetes affects around 38.4 million people in the U.S. — a whopping 11.6% of the U.S. population. Sometimes we can chalk it up to the luck of the genetic draw: one form of diabetes — type 1 — is an inherited autoimmune disease. Type 2 diabetes, on the other hand, develops over time and is the fallout of unhealthy eating habits and a sedentary lifestyle.
And while being overweight isn’t a “prerequisite” for diabetes, obesity and diabetes share some biological features, and benefit from the same treatment.
Wegovy belongs to a class of drugs known as GLP-1 receptor agonists. GLP-1 is a hormone that helps us regulate blood sugar levels and appetite. In its natural form, GLP-1 gets released by the gut after we eat and binds to GLP-1 receptors in the brain and pancreas, triggering insulin release while making us feel full. GLP-1 receptor agonists such as Wegovy step in to do the same: research shows that Wegovy promotes insulin release while making it easier to keep a lid on our snacking habits.
First things first: we might find that taking Wegovy curbs our desire to drink altogether. The reason has to do with the brain. Wegovy works by altering pathways in the hypothalamus — a region that regulates hunger and satiety. As it turns out, it also plays a key role in the reward system that’s at the center of addictive behaviors such as alcohol misuse.
Alcohol hijacks the reward system by artificially boosting dopamine — a neurotransmitter associated with pleasure that’s also involved in motivation and learning. While the reward system evolved to allow us to develop habits necessary for survival — for example, eating or finding a romantic partner — substances such as alcohol trigger dopamine release artificially. That’s what makes it so hard to stop!
Wegovy, in turn, tweaks the reward system pathways in a way that makes alcohol less potent. We don’t get the same “high,” so we’re not as tempted to keep coming back for more. In fact, studies have even shown that Wegovy could be used to curb drinking!
That said, what happens if we do decide to mix alcohol and Wegovy?
We’ve established that our cravings for booze might naturally simmer down when Wegovy is in the mix. But what if they don’t? Can you drink alcohol on Wegovy? Mixing the two could spell trouble for a number of reasons.
If we do mix alcohol and Wegovy, the result isn’t pretty. For one thing, our blood sugar levels could go out of whack. While alcohol increases blood sugar in the long run, the immediate effect is usually a blood sugar drop. Because the body sees alcohol as a poison and prioritizes its metabolism over everything else, it stops releasing glucose — causing a temporary dip in blood sugar.
Because semaglutide lowers our blood sugar as well, we’re in for an all-time low when we combine Wegovy and alcohol. The result? We might feel dizzy, confused, or even pass out.
But that’s not all! Like any medication, Wegovy is not without its side effects.
What are Wegovy side effects with alcohol? Here’s what we might be in store for if we combine the two:
It’s clear that combining Wegovy side effects with alcohol’s impact makes for an unpleasant — and possibly dangerous — combination. Drinking on Wegovy is likely to cause trouble, especially if we overdo it.
Last but certainly not least, here’s one of the most important reasons why alcohol and Wegovy are a problematic pair: booze can sabotage our weight loss efforts, throwing a wrench in the progress we’ve made, and maybe even sending us back to the state that led us to start taking the medication in the first place. Here’s why the two play for opposite teams:
It’s best to steer clear of alcohol while on Wegovy. This not only helps us with our weight loss but promotes a healthier lifestyle all around.

It can feel challenging to navigate the weight loss journey while also trying to drink less. The great news is that the same tools can make both goals easier to reach. Here are some of the most effective ones:
And remember, the Reframe community is here to help you every step of the way. Check out our vibrant 24/7 Forum where others who’ve been in your shoes and know what it’s like are ready to share their stories and advice. We’re rooting for you!
Whether or not we’re taking Wegovy, quitting alcohol will only help our weight loss efforts. Losing weight and reducing alcohol intake both involve being mindful of what we put in our body, and as we adjust our habits, we can look forward to a healthier, more vibrant lifestyle!

Mixing Excedrin and alcohol can strain your liver and increase health risks. Learn how long to wait after taking Excedrin before having a drink.
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually, with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet hundreds of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
You're headed out for a friend's birthday, but a familiar migraine starts to creep in. You take an Excedrin, hoping to stop it before it ruins the night. Later, as everyone raises a glass to celebrate, you hesitate. Can you drink on Excedrin? It feels like a simple question, but the interaction between Excedrin and alcohol is more serious than you might think, putting a huge strain on your liver. We'll break down exactly what happens in your body and answer that crucial question: how long after taking Excedrin can I drink alcohol?
Your migraine may be at bay, but having a drink while taking Excedrin still isn’t a good idea. Let’s examine how alcohol and Excedrin interact to understand why mixing the two can be a recipe for disaster.

Excedrin is an over-the-counter pain medication used specifically to treat migraines and tension headaches. The medication is made of a combination of three main components:
Together, the three components work together to mitigate migraines and tension headaches, distinguishing Excedrin from other pain medications.
Alcohol is a common trigger for migraines due to the numerous factors:
As we can see, alcohol is directly linked to an increased risk of migraines, as it sets the scene. So if we take Excedrin to ease our migraines, does it cancel out the negative effects of alcohol?
On the contrary, alcohol can interact with all three components of Excedrin — making it even more dangerous than mixing alcohol with each of the ingredients on its own. Alcohol, acetaminophen, and aspirin are all broken down by our mighty liver. However, our liver can only do so much at once.
Since alcohol interacts with all three active ingredients in Excedrin, drinking can cause serious consequences.
Excedrin isn’t recommended to be taken before, during, or after drinking. Both substances stay in our body for much longer than when they’re first consumed. This means that even though some time may have passed since we started drinking, alcohol can still be in our body and negatively interact with Excedrin.
We all metabolize alcohol differently, and the time it takes our body to break down and eliminate alcohol can differ from person to person, depending on factors such as the amount of alcohol and the timeframe in which it was consumed. In general, it takes about an hour to metabolize a standard drink. However, since this changes depending on many factors, it’s difficult to determine an exact timeframe, so it’s best to err on the side of caution.
Our migraine may be going away after taking Excedrin, so we may be wondering when it’s okay to drink. As with alcohol, the medication takes time to be metabolized and eliminated from our system.
The half-life of Excedrin is 10 hours. This means that it takes about 10 hours for half of the medication to be eliminated. For it to be completely eliminated, it can take a minimum of 20 hours. To be safe, it’s recommended to wait at least 24-48 hours after taking Excedrin to drink.
Drinking after taking Excedrin can also increase the risk of triggering another migraine. Although we may feel better after taking the medication, Excedrin could just be suppressing symptoms. Drinking alcohol, a known migraine trigger, could aggravate symptoms that can become even more severe once the medication subsides. If we’ve already accidentally had a drink, should we panic?
It’s best to avoid all alcohol when taking Excedrin. That being said, if we drink, it’s best to wait an hour for each standard drink we consume. This can minimize the adverse effects and give our body time to metabolize each of the substances separately. However, it’s important to note that the “one standard drink per hour” rule is an average and may not be the same for everyone. In addition, two or three standard drinks in one hour can overload our liver and drastically change everything.
To avoid any adverse effects, the best course of action is to avoid mixing alcohol and Excedrin.
Beyond the immediate risks of mixing substances, there’s another tricky situation to consider: rebound headaches. This happens when you overuse pain medication, leading to a cycle where the medicine itself starts causing headaches once it wears off. Since Excedrin is so effective, it can be tempting to take it frequently, but this can unfortunately lead to this very pattern. Adding alcohol to the mix only complicates things. Since alcohol is a known migraine trigger, drinking while Excedrin is still in your system can set you up for a more severe headache once the medication’s effects fade.
This is why timing is so important. The half-life of Excedrin is about 10 hours, meaning it takes that long for just half of the drug to leave your system. For it to be completely eliminated, you’re looking at a minimum of 20 hours. To be on the safe side, it’s best to wait at least 24 to 48 hours after taking Excedrin before you have a drink. This gives your body, especially your liver, enough time to process the medication fully, reducing the risk of a dangerous interaction and helping you avoid a potential rebound headache triggered by alcohol.
So, what if you’ve already had a drink after taking Excedrin? First, don’t panic. The best thing you can do is stop drinking immediately to prevent any further interaction. Since alcohol interacts with all three active ingredients in Excedrin, the potential for adverse effects is real, and continuing to drink will only increase that risk. Pay close attention to how you’re feeling. If you notice symptoms like severe stomach pain, nausea, vomiting, dizziness, or black, tarry stools, it’s time to seek medical attention right away. These could be signs of gastrointestinal bleeding or liver issues.
If you find yourself in this situation often—relying on Excedrin for frequent headaches while also wanting to drink—it’s a good idea to talk to a doctor. This pattern could point to an underlying issue, like chronic migraines, that needs a different management plan. A healthcare professional can help find the root cause and explore safer treatments. This is also a great opportunity to reflect on your drinking patterns and how they affect your well-being, which is a key part of practicing mindful drinking.
Alcohol and Excedrin have direct interactions that can lead to serious effects:
Now that we’ve determined that mixing the two can be dangerous, how long should we wait between them?
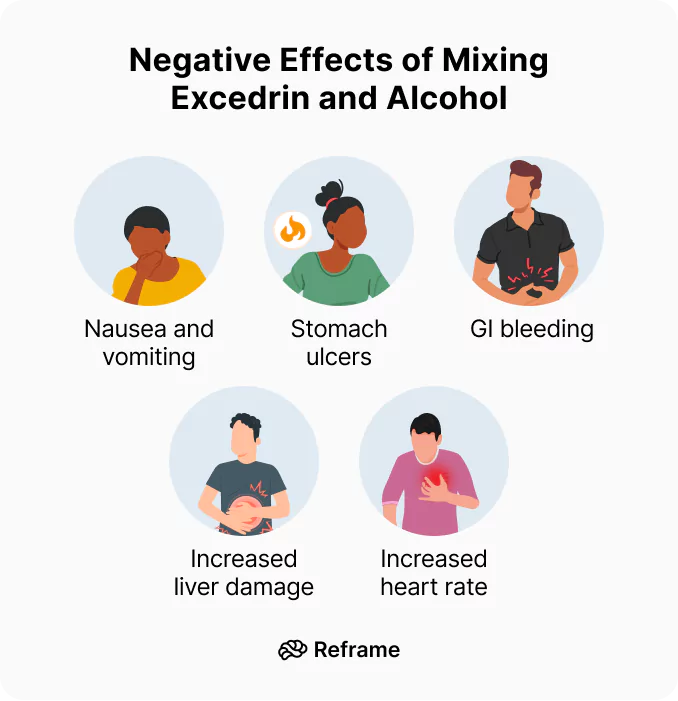
While some side effects are mild, mixing Excedrin and alcohol can lead to severe health complications that require immediate medical attention. Knowing the warning signs can help you act quickly if a serious issue arises. It’s crucial to listen to your body and not dismiss symptoms that could indicate a deeper problem, especially when combining substances that are hard on your system.
Your liver works hard to process both acetaminophen and alcohol, and combining them can cause severe liver damage. Be on the lookout for symptoms like fever, chills, unusual tiredness, joint pain, nausea, or a loss of appetite. More obvious signs include yellowing of your skin or the whites of your eyes (jaundice) and any unusual bleeding or bruising. The aspirin in Excedrin, an NSAID, also increases the risk of stomach bleeding. When mixed with alcohol, which thins the blood, this danger becomes even more pronounced. If you experience any of these symptoms, it’s time to seek medical help right away.
Beyond liver and stomach issues, other symptoms can signal a bad reaction. Nausea and vomiting are potential side effects of Excedrin on its own, and alcohol can certainly cause the same. When you take them together, you significantly increase the chances of feeling sick to your stomach. While it might be easy to brush this off as a typical side effect of drinking, persistent or severe vomiting after mixing the two shouldn't be ignored. It’s your body’s way of telling you that something is wrong, and it’s important to pay attention to these signals to prevent further complications.
Because both substances are processed by the same organ, your liver becomes overworked when you mix alcohol and Excedrin. This strain makes it harder for your body to break down the harmful byproducts of the medication and the toxins from alcohol, which can build up in your system. This overload increases the risk of an accidental overdose, even if you’ve taken the recommended dose of Excedrin. Your liver can only handle so much at once, and pushing it past its limit can lead to lasting damage. This is why it’s so important to give your body a break and avoid this combination entirely.
While mixing Excedrin and alcohol is risky for everyone, certain groups of people are even more vulnerable to the potential negative effects. Factors like age, pre-existing health conditions, and life stages can significantly change how your body reacts to this combination. Understanding these specific risks can help you make safer choices for yourself and your loved ones.
It’s critical to remember that Excedrin contains aspirin, which should not be given to children or teenagers who are recovering from the flu or chickenpox. This is due to the risk of Reye's syndrome, a rare but extremely serious condition that causes swelling in the brain and liver. While it’s uncommon, Reye’s syndrome can be life-threatening. Because of this, it’s always best to consult a doctor for pain relief options for children and teens, and to keep medications containing aspirin away from them, especially when they are ill.
The caffeine in Excedrin is there to help constrict blood vessels and relieve headache pain, but it can also make your heart beat faster and raise your blood pressure. For someone with an existing heart condition or high blood pressure, this can be particularly dangerous. Alcohol can also affect heart rate and blood pressure, and when you combine the two, these cardiovascular effects can be amplified. This added strain on your heart is an unnecessary risk, so if you have any heart-related health concerns, you should be especially cautious about this mixture.
If you are pregnant or breastfeeding, it’s always best to be extra careful about any medications you take. The safety of taking Excedrin during pregnancy or while nursing has not been fully established. The ingredients can pass to the baby through the placenta or breast milk. Given the potential risks and the lack of conclusive safety data, you should always talk to your doctor before taking Excedrin or any other over-the-counter medication. They can help you weigh the benefits and risks and suggest the safest way to manage your headaches.
As we get older, our bodies often process medications and alcohol differently. Older adults may be more sensitive to the side effects of Excedrin, particularly when it’s combined with alcohol. The risk of gastrointestinal bleeding from aspirin and liver damage from acetaminophen can be higher in this age group. Slower metabolism can also mean that both substances stay in the body longer, increasing the window for negative interactions. Because of this heightened vulnerability, older adults should exercise extreme caution and consider alternative pain relief methods if they plan on drinking.
Beyond the direct physical side effects, there are other hidden dangers that come from mixing Excedrin and alcohol. These substances can interact in ways that affect your judgment and mask warning signs from your body, leading to potentially dangerous situations. Understanding these less obvious interactions is just as important as knowing the direct health risks.
The caffeine in Excedrin is a stimulant, while alcohol is a depressant. When you mix them, the caffeine can mask some of alcohol’s sedative effects, making you feel more alert and less intoxicated than you actually are. This can be a dangerous illusion, as it might lead you to drink more than you normally would, thinking you’re fine. However, your motor skills, judgment, and reaction time are still impaired by the alcohol. This false sense of sobriety increases the risk of accidents and alcohol poisoning, all while both substances continue to strain your heart and liver.
The danger of Excedrin lies in its three active ingredients, and alcohol interacts negatively with every single one of them. This isn't like mixing alcohol with a single-ingredient medication; it's a triple threat. The acetaminophen strains your liver, the aspirin increases the risk of stomach bleeding, and the caffeine puts extra stress on your heart. Each of these interactions is risky on its own, but when they happen all at once, the potential for harm is much greater. This is why the advice is so clear: avoid drinking alcohol if you have taken Excedrin.
There’s no need to panic if we accidentally mix the two, but it’s best to stop drinking immediately and take the proper precautions:
Migraines can be debilitating. Mixing a treatment and trigger for migraines is a recipe for disaster. So, how can we approach drinking and Excedrin safely?
There’s no “safe” way to drink while taking Excedrin. However, implementing mindful drinking practices can help reduce the risk of harmful consequences:
These mindful practices will limit interactions between Excedrin and alcohol and help us better manage our migraines.
If you’re dealing with a headache but know you’ll be in a situation where you might drink, it’s smart to reconsider your choice of pain reliever. The combination of acetaminophen and aspirin in Excedrin poses specific dangers when mixed with alcohol. As we’ve covered, the acetaminophen-alcohol duo puts significant strain on your liver, while the aspirin-alcohol mix can increase the risk of stomach bleeding. Mixing Excedrin and alcohol can lead to serious health issues that are best avoided. If you absolutely need pain relief, some alternatives like ibuprofen or naproxen don’t carry the same risk of liver damage. However, they can still irritate the stomach, so the safest bet is always to avoid mixing any medication with alcohol.
Beyond just avoiding a dangerous interaction, it’s helpful to look at the bigger picture: your relationship with alcohol and migraines. Alcohol is a very common trigger for migraines for several reasons, including dehydration, the expansion of blood vessels in the brain, and sleep disruption. By choosing not to drink, you’re not only preventing the risky combination with Excedrin, but you may also be preventing the migraine from happening in the first place. This is where mindful drinking comes in. By becoming more aware of how alcohol affects your body, you can better identify your personal triggers and make choices that support your overall well-being, leading to fewer migraines and less need for medication over time.
Excedrin is made of a specific combination of ingredients that make it an effective pain reliever for migraines and tension headaches. Alcohol not only acts as a trigger for migraines, which Excedrin is used to treat but also directly interacts with all three components of the medication — leading to potentially dangerous symptoms. Avoiding drinking not only prevents the adverse effects of mixing alcohol and Excedrin but also minimizes triggers for migraines. Skip the champagne (and all alcohol for that matter) and avoid a migraine!
How long after taking Excedrin can I safely have a drink? The safest bet is to wait at least 24 to 48 hours. Excedrin has a half-life of about 10 hours, which means it takes that long for just half of the medication to leave your system. Giving your body a full day or two ensures your liver has completely processed the medicine, so it isn't overworked when you introduce alcohol.
What if I only have one drink? Is it still risky? Yes, it's still a risk I wouldn't recommend taking. Even a single drink requires your liver to process it, and if it's already busy breaking down the three active ingredients in Excedrin, you're putting it under unnecessary strain. This can increase your chances of side effects like stomach irritation and potential liver damage. It's just not worth it for one drink.
I sometimes take Excedrin for a hangover headache. Is that a bad idea? This is a really common habit, but it's unfortunately one of the worst times to take Excedrin. When you have a hangover, your body is already dealing with dehydration and your liver is working hard to clear the byproducts of alcohol. Adding Excedrin to the mix puts a heavy burden on your already-stressed liver and can seriously increase the risk of stomach bleeding and other complications.
What are the most serious symptoms I should watch for if I've already mixed them? Pay close attention to how your body feels. If you experience severe stomach pain, persistent nausea or vomiting, dizziness, or notice any signs of internal bleeding like black or tarry stools, you should seek medical attention right away. Other serious warning signs include yellowing of your skin or eyes, which can indicate liver issues. Don't try to wait these symptoms out.
Are other painkillers like Advil or Tylenol safer to take with alcohol? No painkiller is completely safe to mix with alcohol, but they carry different risks. Tylenol (acetaminophen) combined with alcohol is notoriously hard on your liver. Advil (ibuprofen), like the aspirin in Excedrin, is an NSAID that can increase the risk of stomach bleeding when taken with alcohol. Because Excedrin contains both acetaminophen and an NSAID (aspirin), it presents a unique combination of risks to both your liver and your stomach.
You're headed out for a friend's birthday, but a familiar migraine starts to creep in. You take an Excedrin, hoping to stop it before it ruins the night. Later, as everyone raises a glass to celebrate, you hesitate. Can you drink on Excedrin? It feels like a simple question, but the interaction between Excedrin and alcohol is more serious than you might think, putting a huge strain on your liver. We'll break down exactly what happens in your body and answer that crucial question: how long after taking Excedrin can I drink alcohol?
Your migraine may be at bay, but having a drink while taking Excedrin still isn’t a good idea. Let’s examine how alcohol and Excedrin interact to understand why mixing the two can be a recipe for disaster.

Excedrin is an over-the-counter pain medication used specifically to treat migraines and tension headaches. The medication is made of a combination of three main components:
Together, the three components work together to mitigate migraines and tension headaches, distinguishing Excedrin from other pain medications.
Alcohol is a common trigger for migraines due to the numerous factors:
As we can see, alcohol is directly linked to an increased risk of migraines, as it sets the scene. So if we take Excedrin to ease our migraines, does it cancel out the negative effects of alcohol?
On the contrary, alcohol can interact with all three components of Excedrin — making it even more dangerous than mixing alcohol with each of the ingredients on its own. Alcohol, acetaminophen, and aspirin are all broken down by our mighty liver. However, our liver can only do so much at once.
Since alcohol interacts with all three active ingredients in Excedrin, drinking can cause serious consequences.
Excedrin isn’t recommended to be taken before, during, or after drinking. Both substances stay in our body for much longer than when they’re first consumed. This means that even though some time may have passed since we started drinking, alcohol can still be in our body and negatively interact with Excedrin.
We all metabolize alcohol differently, and the time it takes our body to break down and eliminate alcohol can differ from person to person, depending on factors such as the amount of alcohol and the timeframe in which it was consumed. In general, it takes about an hour to metabolize a standard drink. However, since this changes depending on many factors, it’s difficult to determine an exact timeframe, so it’s best to err on the side of caution.
Our migraine may be going away after taking Excedrin, so we may be wondering when it’s okay to drink. As with alcohol, the medication takes time to be metabolized and eliminated from our system.
The half-life of Excedrin is 10 hours. This means that it takes about 10 hours for half of the medication to be eliminated. For it to be completely eliminated, it can take a minimum of 20 hours. To be safe, it’s recommended to wait at least 24-48 hours after taking Excedrin to drink.
Drinking after taking Excedrin can also increase the risk of triggering another migraine. Although we may feel better after taking the medication, Excedrin could just be suppressing symptoms. Drinking alcohol, a known migraine trigger, could aggravate symptoms that can become even more severe once the medication subsides. If we’ve already accidentally had a drink, should we panic?
It’s best to avoid all alcohol when taking Excedrin. That being said, if we drink, it’s best to wait an hour for each standard drink we consume. This can minimize the adverse effects and give our body time to metabolize each of the substances separately. However, it’s important to note that the “one standard drink per hour” rule is an average and may not be the same for everyone. In addition, two or three standard drinks in one hour can overload our liver and drastically change everything.
To avoid any adverse effects, the best course of action is to avoid mixing alcohol and Excedrin.
Beyond the immediate risks of mixing substances, there’s another tricky situation to consider: rebound headaches. This happens when you overuse pain medication, leading to a cycle where the medicine itself starts causing headaches once it wears off. Since Excedrin is so effective, it can be tempting to take it frequently, but this can unfortunately lead to this very pattern. Adding alcohol to the mix only complicates things. Since alcohol is a known migraine trigger, drinking while Excedrin is still in your system can set you up for a more severe headache once the medication’s effects fade.
This is why timing is so important. The half-life of Excedrin is about 10 hours, meaning it takes that long for just half of the drug to leave your system. For it to be completely eliminated, you’re looking at a minimum of 20 hours. To be on the safe side, it’s best to wait at least 24 to 48 hours after taking Excedrin before you have a drink. This gives your body, especially your liver, enough time to process the medication fully, reducing the risk of a dangerous interaction and helping you avoid a potential rebound headache triggered by alcohol.
So, what if you’ve already had a drink after taking Excedrin? First, don’t panic. The best thing you can do is stop drinking immediately to prevent any further interaction. Since alcohol interacts with all three active ingredients in Excedrin, the potential for adverse effects is real, and continuing to drink will only increase that risk. Pay close attention to how you’re feeling. If you notice symptoms like severe stomach pain, nausea, vomiting, dizziness, or black, tarry stools, it’s time to seek medical attention right away. These could be signs of gastrointestinal bleeding or liver issues.
If you find yourself in this situation often—relying on Excedrin for frequent headaches while also wanting to drink—it’s a good idea to talk to a doctor. This pattern could point to an underlying issue, like chronic migraines, that needs a different management plan. A healthcare professional can help find the root cause and explore safer treatments. This is also a great opportunity to reflect on your drinking patterns and how they affect your well-being, which is a key part of practicing mindful drinking.
Alcohol and Excedrin have direct interactions that can lead to serious effects:
Now that we’ve determined that mixing the two can be dangerous, how long should we wait between them?
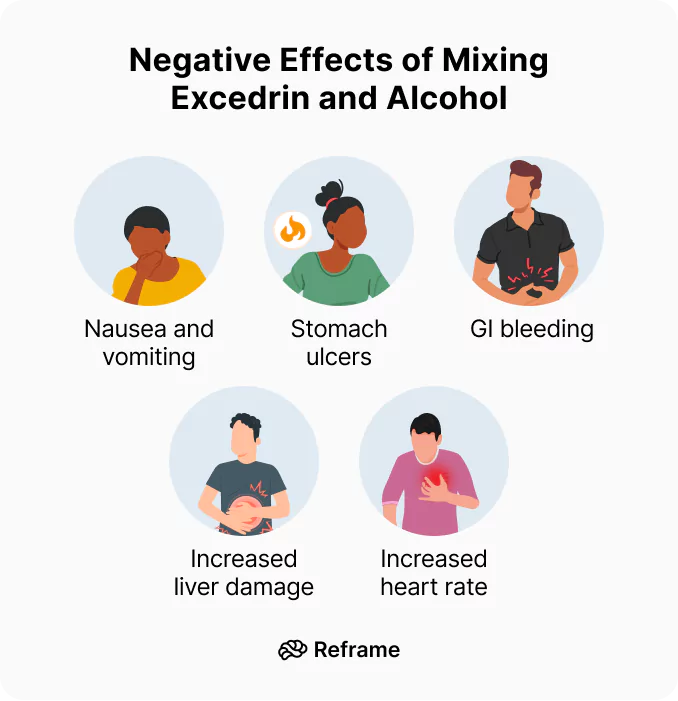
While some side effects are mild, mixing Excedrin and alcohol can lead to severe health complications that require immediate medical attention. Knowing the warning signs can help you act quickly if a serious issue arises. It’s crucial to listen to your body and not dismiss symptoms that could indicate a deeper problem, especially when combining substances that are hard on your system.
Your liver works hard to process both acetaminophen and alcohol, and combining them can cause severe liver damage. Be on the lookout for symptoms like fever, chills, unusual tiredness, joint pain, nausea, or a loss of appetite. More obvious signs include yellowing of your skin or the whites of your eyes (jaundice) and any unusual bleeding or bruising. The aspirin in Excedrin, an NSAID, also increases the risk of stomach bleeding. When mixed with alcohol, which thins the blood, this danger becomes even more pronounced. If you experience any of these symptoms, it’s time to seek medical help right away.
Beyond liver and stomach issues, other symptoms can signal a bad reaction. Nausea and vomiting are potential side effects of Excedrin on its own, and alcohol can certainly cause the same. When you take them together, you significantly increase the chances of feeling sick to your stomach. While it might be easy to brush this off as a typical side effect of drinking, persistent or severe vomiting after mixing the two shouldn't be ignored. It’s your body’s way of telling you that something is wrong, and it’s important to pay attention to these signals to prevent further complications.
Because both substances are processed by the same organ, your liver becomes overworked when you mix alcohol and Excedrin. This strain makes it harder for your body to break down the harmful byproducts of the medication and the toxins from alcohol, which can build up in your system. This overload increases the risk of an accidental overdose, even if you’ve taken the recommended dose of Excedrin. Your liver can only handle so much at once, and pushing it past its limit can lead to lasting damage. This is why it’s so important to give your body a break and avoid this combination entirely.
While mixing Excedrin and alcohol is risky for everyone, certain groups of people are even more vulnerable to the potential negative effects. Factors like age, pre-existing health conditions, and life stages can significantly change how your body reacts to this combination. Understanding these specific risks can help you make safer choices for yourself and your loved ones.
It’s critical to remember that Excedrin contains aspirin, which should not be given to children or teenagers who are recovering from the flu or chickenpox. This is due to the risk of Reye's syndrome, a rare but extremely serious condition that causes swelling in the brain and liver. While it’s uncommon, Reye’s syndrome can be life-threatening. Because of this, it’s always best to consult a doctor for pain relief options for children and teens, and to keep medications containing aspirin away from them, especially when they are ill.
The caffeine in Excedrin is there to help constrict blood vessels and relieve headache pain, but it can also make your heart beat faster and raise your blood pressure. For someone with an existing heart condition or high blood pressure, this can be particularly dangerous. Alcohol can also affect heart rate and blood pressure, and when you combine the two, these cardiovascular effects can be amplified. This added strain on your heart is an unnecessary risk, so if you have any heart-related health concerns, you should be especially cautious about this mixture.
If you are pregnant or breastfeeding, it’s always best to be extra careful about any medications you take. The safety of taking Excedrin during pregnancy or while nursing has not been fully established. The ingredients can pass to the baby through the placenta or breast milk. Given the potential risks and the lack of conclusive safety data, you should always talk to your doctor before taking Excedrin or any other over-the-counter medication. They can help you weigh the benefits and risks and suggest the safest way to manage your headaches.
As we get older, our bodies often process medications and alcohol differently. Older adults may be more sensitive to the side effects of Excedrin, particularly when it’s combined with alcohol. The risk of gastrointestinal bleeding from aspirin and liver damage from acetaminophen can be higher in this age group. Slower metabolism can also mean that both substances stay in the body longer, increasing the window for negative interactions. Because of this heightened vulnerability, older adults should exercise extreme caution and consider alternative pain relief methods if they plan on drinking.
Beyond the direct physical side effects, there are other hidden dangers that come from mixing Excedrin and alcohol. These substances can interact in ways that affect your judgment and mask warning signs from your body, leading to potentially dangerous situations. Understanding these less obvious interactions is just as important as knowing the direct health risks.
The caffeine in Excedrin is a stimulant, while alcohol is a depressant. When you mix them, the caffeine can mask some of alcohol’s sedative effects, making you feel more alert and less intoxicated than you actually are. This can be a dangerous illusion, as it might lead you to drink more than you normally would, thinking you’re fine. However, your motor skills, judgment, and reaction time are still impaired by the alcohol. This false sense of sobriety increases the risk of accidents and alcohol poisoning, all while both substances continue to strain your heart and liver.
The danger of Excedrin lies in its three active ingredients, and alcohol interacts negatively with every single one of them. This isn't like mixing alcohol with a single-ingredient medication; it's a triple threat. The acetaminophen strains your liver, the aspirin increases the risk of stomach bleeding, and the caffeine puts extra stress on your heart. Each of these interactions is risky on its own, but when they happen all at once, the potential for harm is much greater. This is why the advice is so clear: avoid drinking alcohol if you have taken Excedrin.
There’s no need to panic if we accidentally mix the two, but it’s best to stop drinking immediately and take the proper precautions:
Migraines can be debilitating. Mixing a treatment and trigger for migraines is a recipe for disaster. So, how can we approach drinking and Excedrin safely?
There’s no “safe” way to drink while taking Excedrin. However, implementing mindful drinking practices can help reduce the risk of harmful consequences:
These mindful practices will limit interactions between Excedrin and alcohol and help us better manage our migraines.
If you’re dealing with a headache but know you’ll be in a situation where you might drink, it’s smart to reconsider your choice of pain reliever. The combination of acetaminophen and aspirin in Excedrin poses specific dangers when mixed with alcohol. As we’ve covered, the acetaminophen-alcohol duo puts significant strain on your liver, while the aspirin-alcohol mix can increase the risk of stomach bleeding. Mixing Excedrin and alcohol can lead to serious health issues that are best avoided. If you absolutely need pain relief, some alternatives like ibuprofen or naproxen don’t carry the same risk of liver damage. However, they can still irritate the stomach, so the safest bet is always to avoid mixing any medication with alcohol.
Beyond just avoiding a dangerous interaction, it’s helpful to look at the bigger picture: your relationship with alcohol and migraines. Alcohol is a very common trigger for migraines for several reasons, including dehydration, the expansion of blood vessels in the brain, and sleep disruption. By choosing not to drink, you’re not only preventing the risky combination with Excedrin, but you may also be preventing the migraine from happening in the first place. This is where mindful drinking comes in. By becoming more aware of how alcohol affects your body, you can better identify your personal triggers and make choices that support your overall well-being, leading to fewer migraines and less need for medication over time.
Excedrin is made of a specific combination of ingredients that make it an effective pain reliever for migraines and tension headaches. Alcohol not only acts as a trigger for migraines, which Excedrin is used to treat but also directly interacts with all three components of the medication — leading to potentially dangerous symptoms. Avoiding drinking not only prevents the adverse effects of mixing alcohol and Excedrin but also minimizes triggers for migraines. Skip the champagne (and all alcohol for that matter) and avoid a migraine!
How long after taking Excedrin can I safely have a drink? The safest bet is to wait at least 24 to 48 hours. Excedrin has a half-life of about 10 hours, which means it takes that long for just half of the medication to leave your system. Giving your body a full day or two ensures your liver has completely processed the medicine, so it isn't overworked when you introduce alcohol.
What if I only have one drink? Is it still risky? Yes, it's still a risk I wouldn't recommend taking. Even a single drink requires your liver to process it, and if it's already busy breaking down the three active ingredients in Excedrin, you're putting it under unnecessary strain. This can increase your chances of side effects like stomach irritation and potential liver damage. It's just not worth it for one drink.
I sometimes take Excedrin for a hangover headache. Is that a bad idea? This is a really common habit, but it's unfortunately one of the worst times to take Excedrin. When you have a hangover, your body is already dealing with dehydration and your liver is working hard to clear the byproducts of alcohol. Adding Excedrin to the mix puts a heavy burden on your already-stressed liver and can seriously increase the risk of stomach bleeding and other complications.
What are the most serious symptoms I should watch for if I've already mixed them? Pay close attention to how your body feels. If you experience severe stomach pain, persistent nausea or vomiting, dizziness, or notice any signs of internal bleeding like black or tarry stools, you should seek medical attention right away. Other serious warning signs include yellowing of your skin or eyes, which can indicate liver issues. Don't try to wait these symptoms out.
Are other painkillers like Advil or Tylenol safer to take with alcohol? No painkiller is completely safe to mix with alcohol, but they carry different risks. Tylenol (acetaminophen) combined with alcohol is notoriously hard on your liver. Advil (ibuprofen), like the aspirin in Excedrin, is an NSAID that can increase the risk of stomach bleeding when taken with alcohol. Because Excedrin contains both acetaminophen and an NSAID (aspirin), it presents a unique combination of risks to both your liver and your stomach.

Alcohol has many interactions with different medications and doxycycline is no exception. Check out our latest blog for more info on how long we should wait to drink safely.
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually, with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet hundreds of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
You’ve just finished your dose of doxycycline and are out with friends for dinner. Everyone orders a drink and as you’re about to order a glass of wine, you remember that alcohol and antibiotics shouldn’t be mixed. Although you’re feeling better, you don’t want to compromise the recovery process. But how long you should wait after taking doxycycline before drinking?
Let’s learn how doxycycline works in our body and understand why taking a brief hiatus from alcohol can be a small yet significant step in our quest for safer and more mindful drinking.

Doxycycline is a medication used to treat bacterial infections in many parts of the body. Known as a tetracycline antibiotic, it kills bacteria or prevents their growth by stopping the production of proteins that bacteria need to survive. Given its anti-inflammatory properties, Doxycycline is often used to treat skin, chest, dental, and some sexually transmitted infections.
The medication comes in several variations such as a liquid, capsule, tablet, and delayed-relapse tablet. It’s sold under the brand names Vibramycin-D, Efracea, and Periostat. The dosage depends on the reason the medication is prescribed but is typically between 100 mg to 200 mg. Low doses typically used for skin and gum infections aren’t associated with adverse effects. Doxycycline (100 mg) side effects may include diarrhea, vomiting, oral or vaginal thrush, rash, irritation of the esophagus, loss of sense of taste, and ringing in ears. More serious side effects may require emergency medical attention:
Before we discuss specific doxycycline interactions, let’s first understand why alcohol and antibiotics are a dangerous combination.
Drinking while taking any type of antibiotic is not recommended. Some antibiotics, such as metronidazole, tinidazole, griseofulvin, cefoperazone, and more, interact directly with alcohol. Mixing these antibiotics with alcohol can lead to such side effects as a racing heart rate, vomiting, and severe headache.
Even antibiotics without direct interactions can result in increased risks and negative effects when mixed with alcohol. Alcohol impairs our immune function, which is critical in helping us fight against infection and recover quickly. If we’re looking to give our body the best fighting chance to rid us of infections and avoid adverse reactions, drinking while on antibiotics is never a good idea. Let’s further examine how doxycycline and alcohol interact to give us a better idea of how long we should wait to drink.
Research on the specific ways that alcohol impacts doxycycline is limited, but we do know that mixing alcohol with medications is not recommended since alcohol affects absorption. This means that drinking impacts the effectiveness of doxycycline.
Alcohol also negatively impacts our immune system, which is critical in fighting infections. It’s a toxin that increases stress in our body and distracts our body from critical functions. Alcohol also kills healthy bacteria that aids in maintaining immune health and can indirectly compromise the effectiveness of the medication, slowing down recovery.
Although the combination of doxycycline and alcohol aren’t associated with dangerous effects, many of their side effects overlap. This can increase the risk and exacerbate overlapping side effects. Due to the many potential interactions between alcohol and doxycycline, manufacturers recommend choosing an alternative medication if a patient chooses to drink. But what about after completing the medication regimen?
Doxycycline has an average half-life of 16 to 22 hours. This means that it can take anywhere from 32-44 hours to be eliminated. However, studies show that it can take about five half-lives for a drug to be completely eliminated from our system. To be safe, waiting about five days after stopping doxycycline to drink alcohol is what’s recommended.
Drinking before the five-day period ends may not present any immediate dangers, as there are no direct interactions between alcohol and doxycycline. However, it can indirectly impact healing and open the door to potential risks. With that in mind, if we’ve accidentally had one drink, should we be worried?

When taking doxycycline, alcohol consumption isn’t recommended in any amount. Although mixing doxycycline and alcohol isn’t associated with severely dangerous effects, we all are affected by alcohol and other substances differently. This makes it difficult to determine a “safe” amount of alcohol when taking doxycycline.
According to the World Health Organization (WHO), no amount of alcohol is safe — with or without doxycycline. If we’re choosing to drink, we should aim to follow moderation consumption guidelines to minimize the risks. We can also consult with our doctor for more individualized recommendations. Even after stopping doxycycline, the drug lingers in our body — opening the door to indirect interactions with alcohol. Let’s get a better picture of the risks.
Even without any direct interactions, mixing doxycycline and alcohol can cause serious effects:
As we can see from the long list of negative effects, mixing doxycycline and alcohol can lead to double the trouble. If we’re prescribed doxycycline, how can we navigate drinking safely?
Drinking while taking doxycycline and before the five-day elimination period of the medication isn’t recommended. However, if we’re choosing to drink, we can minimize the risks and improve our safety by implementing these mindful drinking practices:
These mindful consumption strategies can apply to doxycycline and, in general, help us develop a more balanced approach to drinking.
Understanding the interplay between medications like doxycycline and alcohol is a commitment to better health and mindful living. Although there are no direct interactions between doxycycline and alcohol, the combination can still cause unnecessary risks. We can avoid the adverse effects of mixing alcohol and doxycycline by ensuring that we wait for the five-day elimination window to pass. Whether we're stepping away from doxycycline or simply exploring a more temperate relationship with alcohol, patience, and timing are our trusted allies.
You’ve just finished your dose of doxycycline and are out with friends for dinner. Everyone orders a drink and as you’re about to order a glass of wine, you remember that alcohol and antibiotics shouldn’t be mixed. Although you’re feeling better, you don’t want to compromise the recovery process. But how long you should wait after taking doxycycline before drinking?
Let’s learn how doxycycline works in our body and understand why taking a brief hiatus from alcohol can be a small yet significant step in our quest for safer and more mindful drinking.

Doxycycline is a medication used to treat bacterial infections in many parts of the body. Known as a tetracycline antibiotic, it kills bacteria or prevents their growth by stopping the production of proteins that bacteria need to survive. Given its anti-inflammatory properties, Doxycycline is often used to treat skin, chest, dental, and some sexually transmitted infections.
The medication comes in several variations such as a liquid, capsule, tablet, and delayed-relapse tablet. It’s sold under the brand names Vibramycin-D, Efracea, and Periostat. The dosage depends on the reason the medication is prescribed but is typically between 100 mg to 200 mg. Low doses typically used for skin and gum infections aren’t associated with adverse effects. Doxycycline (100 mg) side effects may include diarrhea, vomiting, oral or vaginal thrush, rash, irritation of the esophagus, loss of sense of taste, and ringing in ears. More serious side effects may require emergency medical attention:
Before we discuss specific doxycycline interactions, let’s first understand why alcohol and antibiotics are a dangerous combination.
Drinking while taking any type of antibiotic is not recommended. Some antibiotics, such as metronidazole, tinidazole, griseofulvin, cefoperazone, and more, interact directly with alcohol. Mixing these antibiotics with alcohol can lead to such side effects as a racing heart rate, vomiting, and severe headache.
Even antibiotics without direct interactions can result in increased risks and negative effects when mixed with alcohol. Alcohol impairs our immune function, which is critical in helping us fight against infection and recover quickly. If we’re looking to give our body the best fighting chance to rid us of infections and avoid adverse reactions, drinking while on antibiotics is never a good idea. Let’s further examine how doxycycline and alcohol interact to give us a better idea of how long we should wait to drink.
Research on the specific ways that alcohol impacts doxycycline is limited, but we do know that mixing alcohol with medications is not recommended since alcohol affects absorption. This means that drinking impacts the effectiveness of doxycycline.
Alcohol also negatively impacts our immune system, which is critical in fighting infections. It’s a toxin that increases stress in our body and distracts our body from critical functions. Alcohol also kills healthy bacteria that aids in maintaining immune health and can indirectly compromise the effectiveness of the medication, slowing down recovery.
Although the combination of doxycycline and alcohol aren’t associated with dangerous effects, many of their side effects overlap. This can increase the risk and exacerbate overlapping side effects. Due to the many potential interactions between alcohol and doxycycline, manufacturers recommend choosing an alternative medication if a patient chooses to drink. But what about after completing the medication regimen?
Doxycycline has an average half-life of 16 to 22 hours. This means that it can take anywhere from 32-44 hours to be eliminated. However, studies show that it can take about five half-lives for a drug to be completely eliminated from our system. To be safe, waiting about five days after stopping doxycycline to drink alcohol is what’s recommended.
Drinking before the five-day period ends may not present any immediate dangers, as there are no direct interactions between alcohol and doxycycline. However, it can indirectly impact healing and open the door to potential risks. With that in mind, if we’ve accidentally had one drink, should we be worried?

When taking doxycycline, alcohol consumption isn’t recommended in any amount. Although mixing doxycycline and alcohol isn’t associated with severely dangerous effects, we all are affected by alcohol and other substances differently. This makes it difficult to determine a “safe” amount of alcohol when taking doxycycline.
According to the World Health Organization (WHO), no amount of alcohol is safe — with or without doxycycline. If we’re choosing to drink, we should aim to follow moderation consumption guidelines to minimize the risks. We can also consult with our doctor for more individualized recommendations. Even after stopping doxycycline, the drug lingers in our body — opening the door to indirect interactions with alcohol. Let’s get a better picture of the risks.
Even without any direct interactions, mixing doxycycline and alcohol can cause serious effects:
As we can see from the long list of negative effects, mixing doxycycline and alcohol can lead to double the trouble. If we’re prescribed doxycycline, how can we navigate drinking safely?
Drinking while taking doxycycline and before the five-day elimination period of the medication isn’t recommended. However, if we’re choosing to drink, we can minimize the risks and improve our safety by implementing these mindful drinking practices:
These mindful consumption strategies can apply to doxycycline and, in general, help us develop a more balanced approach to drinking.
Understanding the interplay between medications like doxycycline and alcohol is a commitment to better health and mindful living. Although there are no direct interactions between doxycycline and alcohol, the combination can still cause unnecessary risks. We can avoid the adverse effects of mixing alcohol and doxycycline by ensuring that we wait for the five-day elimination window to pass. Whether we're stepping away from doxycycline or simply exploring a more temperate relationship with alcohol, patience, and timing are our trusted allies.

Mixing Librium and alcohol is dangerous. Learn how long after taking Librium can I drink alcohol, plus key risks and safety tips for your health.
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually, with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet hundreds of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
Alcohol withdrawal is a uniquely miserable experience. If you’ve been there, you know the feeling: drenched in sweat but shivering, with hands too shaky to even hold a glass of water. It’s a physical and mental ordeal that often requires medical help to get through safely. That’s where a medication like Librium often comes in, prescribed by doctors to calm the storm in your nervous system. But this raises a critical question, especially once the worst is over. Many people wonder, how long after taking Librium can I drink alcohol? It’s a tempting thought, but mixing the two is a dangerous game. This article will break down exactly why this combination is so risky, what happens in your body, and what you need to know before even considering a drink.
Luckily, these days we have Librium to help us out when the situation calls for it. While it was originally developed to treat anxiety, these days it’s primarily used to treat alcohol withdrawal. But what happens if you mix Librium with alcohol? Let’s look into the harmful effects of mixing these two substances.

Had history taken a different turn, Librium could have gone undiscovered, tossed into a garbage can at the Hoffmann-La Roche labs in New Jersey in 1954. As the story goes, it was discovered by accident when scientist Leo Sternbach started tinkering with a class of heretofore unknown compounds dubbed “benzheptoxdiazines.” He helped synthesize these compounds 20 years earlier but couldn’t derive any pharmacological use out of them. One of the versions he came up with — a crystalline powder labeled “Ro 5-0690” — ended up on the shelf (and almost in the garbage can, when Sternbach’s lab was getting cleaned over a year later).
As you may have guessed, this was the first version of Librium — a compound that ended up having powerful hypnotic and sedative effects in mice and acted as a potent muscle relaxer in cats. Soon enough this early benzodiazepine passed clinical trials and went from relaxing felines to quelling anxiety and insomnia in humans. Unfortunately, it also made people slur their words and lose coordination, so the interest in the drug fizzled out until it was picked up by other investigators who had better luck and eventually got it approved by the FDA in 1960.
### Chlordiazepoxide: The Generic NameWhile Librium is the name most people recognize, its generic name is chlordiazepoxide. According to MedlinePlus, "Chlordiazepoxide (Librium) is a medicine used for anxiety, pre-surgery worries, and to help with alcohol withdrawal symptoms. It's a type of calming drug called a 'benzodiazepine.'" Think of it like Tylenol versus acetaminophen — one is the brand name, and the other is the active ingredient doing the work. As the first-ever benzodiazepine, chlordiazepoxide paved the way for other well-known medications like Valium and Xanax. It works by slowing down activity in the brain, which is why it’s so effective at managing the intense symptoms that come with alcohol withdrawal.
Although it’s a go-to for managing alcohol withdrawal today, chlordiazepoxide was originally created to treat anxiety. Its calming effect on the central nervous system makes it useful for a variety of conditions beyond just helping people safely stop drinking. As MedlinePlus notes, "Chlordiazepoxide is a medicine that helps calm the brain. It is mainly used to ease anxiety. It also helps control the shaking and upset feelings that happen when someone stops drinking alcohol." This versatility is why it has remained a relevant medication for over 60 years, helping people manage both psychological and physical symptoms tied to an overactive nervous system.
Chlordiazepoxide is highly effective for short-term anxiety relief. It helps quiet the mental noise and physical restlessness that come with anxiety disorders. Interestingly, this calming effect also extends to the gut. Because of the strong connection between our brain and digestive system, chlordiazepoxide is sometimes prescribed to manage the symptoms of irritable bowel syndrome (IBS). Its ability to relax the body can soothe the stomach cramps and discomfort often triggered by stress and anxiety, offering relief when other treatments might not have worked.
It’s completely normal to feel nervous before surgery or a medical procedure. To help manage this, doctors sometimes prescribe chlordiazepoxide to ease pre-operative jitters. A dose before a procedure can help a patient relax, making the experience less stressful for them and easier for the medical team. This short-term use ensures the patient is in a calm state of mind, which can be beneficial for the procedure itself and for their overall comfort. It’s a simple and effective way to take the edge off a high-anxiety situation.
While the original patent for Librium has long expired, you’ll still find chlordiazepoxide sold under that brand name. It’s also available as a generic, which is often more affordable. You might also see it as part of a combination drug called Librax, which pairs chlordiazepoxide with clidinium to treat stomach issues like ulcers and IBS. Whether you’re prescribed the brand name or the generic, the active ingredient is the same. It typically comes in a capsule form, and the dosage will depend entirely on what you’re being treated for and your doctor’s recommendation.
Remember those slurring and stumbling early Librium patients? When we look at how Librium works at a chemical level, it’s not surprising that they seemed, well, drunk.
Just like alcohol, Librium works by enhancing the effects of a neurotransmitter in the brain called gamma-aminobutyric acid (GABA), which helps to calm nervous-system activity. Alcohol does the same (along with suppressing glutamate, its excitatory counterpart).
The result? Relaxation and tranquility. Exactly what we need when our brain chemistry is going haywire during withdrawal. Why? Because the brain is all about balance. If we’ve been drinking for a while, it gets used to the flood of GABA and suppresses its natural production. Switching gears suddenly doesn’t give it time to adjust, so replenishing our GABA with the help of Librium during the transition period makes for a much smoother ride.
Time went on, and benzodiazepines evolved as Valium, Klonopin, and Xanax came onto the scene. While these days they’re usually given preference when it comes to treating anxiety disorders, Librium has become the go-to medication for treating alcohol withdrawal (as well as presurgery anxiety).
Although it’s effective for alcohol withdrawal, taking Librium with alcohol is a whole different story.
In short, it’s not a good idea — and it could be dangerous. Here’s why:
Both Librium and alcohol are depressants that slow down the nervous system. Librium itself can cause severe drowsiness, slowing our heart rate and breathing to potentially dangerous levels.
When we mix the two substances, the downer effects get even more risky. The sedative properties are enhanced, potentially causing dangerous levels of respiratory depression, drowsiness, and dizziness. Even if we don’t stop breathing, the dizziness alone can pose a risk, especially if we’re out and about, crossing streets or operating machinery.
Librium has other side effects that don’t mix well with alcohol:
As we can see, the side effects of Librium don’t combine well with the effects of booze. But there’s even more to the story!
Both alcohol and Librium are processed by the liver, and as we know, the liver is already working overtime to process booze, so adding to its already full plate is asking for trouble.
Besides, if we’ve been drinking for a long time (let’s face it, that’s usually the context in which we get introduced to Librium to begin with), we might already be showing signs of liver disease, such as fatty liver or even cirrhosis. So let’s give it a break! (For more information, check out “How Much Alcohol Causes Liver Damage?”)
Another risk of mixing Librium with booze? We’re playing with danger when it comes to potential overdose risk. Taking both together makes overdose more likely than taking either substance alone. Here are the telltale symptoms:
If things progress, we could end up in a coma or worse. Never ignore the signs of an overdose — seek medical help right away!
What makes an overdose from this combination so dangerous is that there’s no simple fix. Unlike an opioid overdose, which can often be reversed with medication like naloxone, there’s no magic antidote for an overdose on Librium and alcohol. Since both substances are depressants that slow down your central nervous system, their combined effect can dangerously slow or even stop your breathing. Medical teams have very limited options to reverse the effects, making treatment incredibly challenging. Emergency care focuses on life support — like helping a person breathe and managing their vitals — while waiting for the body to process and clear the substances on its own. This is why it’s so critical to avoid this mix in the first place. Once an overdose happens, the situation is extremely dangerous, with very few direct treatments available.
Last but not least, both Librium and alcohol can lead to dependence. In addition to causing a surge of GABA, both trigger the release of dopamine — the so-called “reward neurotransmitter.” As the name suggests, dopamine makes us feel good — it’s a neurological “gold star” our brain rewards us with when we perform a habitual action.
While the reward system evolved to keep habits alive in order to ensure our survival, unfortunately it can’t distinguish between beneficial habits (such as socializing or eating nutritious foods) or destructive ones (such as substance use, gambling, and any other number of habits that also trigger a rush of dopamine).
With both Librium and alcohol in our system, we become more likely to fall into habitual use of either or both substances. We are also more prone to act impulsively, ending up embarrassed at best and possibly putting ourselves in serious danger. (Driving under the influence, jumping into the pool in the middle of December — whatever it is, we’re more likely to do it.) Want to know more about how dependence develops? Take a look at “Understanding Alcohol Dependence: Health Issues, Causes, and How To Overcome.”
The cognitive effects don't stop at fuzzy thinking. Librium on its own can make our memory a bit hazy, and we all know alcohol isn't great for our recall. When you put them together, their ability to disrupt memory formation is amplified, significantly increasing the risk of blackouts. This can lead to those frightening situations where you lose entire chunks of time, unable to piece together what happened or how you got home. It’s more than just forgetting a few details from the night; it’s a complete gap in your memory that can leave you feeling vulnerable and put your personal safety in serious jeopardy. The extreme sleepiness caused by this mix can even lead to passing out, which is dangerous in any situation.
On top of the memory issues, this combination can take a serious toll on our mental health. Both substances are central nervous system depressants, and mixing them can intensify feelings of sadness, hopelessness, and anxiety. Because they both affect our brain's reward system, they can also lead to unpredictable mood swings and impulsive behavior. For anyone already managing depression or other mental health conditions, this mix is especially dangerous, as it can worsen symptoms and make recovery much more difficult. It's a cycle that can be hard to break, as the low mood might make us feel like we need the substances even more. (For more on this, see our article on the link between alcohol and depression.)
If dependence develops on both substances, trying to quit them at the same time can be incredibly risky. Think of it this way: both alcohol and Librium tell your brain to calm down by working on the same neurotransmitter, GABA. When you suddenly take both away, your brain doesn't just go back to normal — it rebounds into a state of high alert. This isn't just a more intense hangover; it's a dangerous situation that can trigger severe withdrawal symptoms, including seizures, hallucinations, and delirium tremens (DTs). Because of these life-threatening risks, detoxing from both substances at once is something that should always be done under medical supervision. It’s simply not safe to go it alone.
Most doctors recommend waiting to make sure Librium is completely out of your system before considering drinking. With a long half-life that ranges anywhere from 5 to 30 hours, some of Librium’s metabolites remain in the system for quite a while, so it’s best to wait at least a few days.
That said, there might be additional considerations to keep in mind when weighing whether drinking after taking Librium is a good idea, even if it’s been a few days. If you were taking Librium for alcohol withdrawal, adding booze back into your life so soon afterwards (or at all) might not be in your best interests. Always check with your doctor first, and stick to the treatment plan you’ve chosen together!
Alcohol withdrawal can be an incredibly challenging experience, both physically and mentally, for those grappling with dependence. When someone decides to quit drinking after prolonged heavy use, their body and brain often struggle to adjust to the sudden absence of alcohol. Symptoms range from mild anxiety and tremors to severe complications like seizures and hallucinations.
In medical settings, managing these symptoms effectively is crucial, and Librium is often used to alleviate some of these uncomfortable symptoms. Librium’s calming effects help mitigate the intensity of withdrawal symptoms, providing a safer and more comfortable transition towards sobriety. However, it's important for individuals undergoing alcohol withdrawal to be under medical supervision, as the dosage and duration of Librium treatment need careful monitoring to prevent dependence on this medication.
Mixing Librium and alcohol can be extremely dangerous due to their combined depressant effects on the central nervous system. Both substances slow down brain activity and cause drowsiness, dizziness, impaired coordination, and memory problems. When taken together, they amplify each other's negative impacts. This combination increases the risk of accidents, falls, and other injuries. Moreover, mixing Librium and alcohol can lead to dangerously low blood pressure, slowed breathing, and even coma in severe cases. Additionally, both substances can be habit-forming on their own, and combining them increases the likelihood of developing dependence and addiction.
It is crucial for individuals prescribed Librium to avoid alcohol completely during treatment and to follow their healthcare provider's instructions carefully to ensure safe and effective recovery
While Librium can be a helpful tool, especially during alcohol withdrawal, it’s a powerful medication that requires respect and caution. It’s not just about avoiding alcohol; there are other important safety measures and potential side effects to be aware of. Understanding these precautions helps ensure you’re using it safely under your doctor's guidance. Think of it as having a complete user manual — knowing the ins and outs is key to a smooth and safe experience. Let's walk through what you need to know, from common side effects to specific warnings for certain situations.
Even when taken exactly as prescribed, Librium can cause side effects. Most are mild and tend to fade as your body adjusts to the medication, but it’s always good to know what to expect. Being aware of potential reactions allows you to monitor how you’re feeling and communicate effectively with your doctor. If anything feels off, don't hesitate to reach out to them. Your well-being is the top priority, and keeping an open line of communication with your healthcare provider is a crucial part of the process.
When you first start taking Librium, you might notice a few changes. The most common side effects include feeling drowsy, dizzy, or tired. Some people also experience a dry mouth, an upset stomach, or changes in their appetite. You might also feel a bit restless or notice things like constipation or blurred vision. These effects are generally not severe, but they can be bothersome. It’s important to give your body time to adapt, but if any of these side effects persist or become particularly annoying, it's a good idea to check in with your doctor.
While rare, Librium can cause more serious side effects that require immediate medical attention. Be on the lookout for symptoms like a shuffling walk, persistent shaking, or an inability to sit still. Other red flags include developing a fever, having trouble breathing or swallowing, or seeing a severe skin rash appear. Yellowing of the skin or eyes (jaundice) or an irregular heartbeat are also serious signs. If you experience any of these, you should contact your doctor or seek emergency medical help right away. Don't wait to see if they go away on their own.
Librium doesn't just interact with alcohol; it can have dangerous reactions with other substances, too. Because it's a central nervous system depressant, mixing it with other drugs that have a similar effect can amplify its sedative properties to a dangerous degree. This is why it's absolutely critical to tell your doctor about every single medication, supplement, or substance you are taking, including over-the-counter drugs and herbal remedies. This transparency allows your doctor to manage your treatment safely and avoid potentially life-threatening combinations that could compromise your health.
Mixing Librium with opioids is extremely dangerous. Both are powerful depressants that slow down your body's functions, particularly your breathing. When taken together, their combined effect is much stronger than either one alone, which can lead to severe respiratory depression — meaning your breathing can slow down to a critical level or stop altogether. This combination greatly increases the risk of a fatal overdose. It can also cause extreme drowsiness, confusion, and loss of consciousness. If you are prescribed opioids for pain, you must inform your doctor that you are also taking Librium.
Librium isn't the right choice for everyone. Certain groups of people need to be extra cautious or avoid the medication entirely due to increased risks. Your age, daily activities, and whether you are pregnant or breastfeeding all play a significant role in determining if Librium is a safe option for you. Always have an honest conversation with your doctor about your lifestyle and health history to ensure your treatment plan is tailored to your specific needs and circumstances, minimizing any potential harm while you focus on your recovery.
Because Librium can cause significant drowsiness and dizziness, you should not drive a car or operate any heavy machinery until you know how the medication affects you. Its sedative effects can impair your judgment, coordination, and reaction time, making these activities unsafe. It’s best to err on the side of caution and avoid getting behind the wheel until you and your doctor are confident that you can do so safely. Your ability to perform these tasks can be unpredictable, especially when you first start the medication.
If you are 65 or older, it’s important to discuss the risks of taking Librium with your doctor. Older adults are often more sensitive to the sedative effects of benzodiazepines, which can increase the risk of falls, confusion, and other adverse effects. Because of this, Librium is often not considered the best choice for this age group, as there may be other medications that are safer and more effective. Your doctor can help you weigh the pros and cons and determine the most appropriate course of action for your situation.
If you are pregnant, planning to become pregnant, or breastfeeding, you need to have a serious talk with your doctor before taking Librium. This medication can pass into breast milk and may cause harm to a nursing baby. Its effects during pregnancy are also a concern, so it's crucial to explore the potential risks to the fetus. Your doctor can provide guidance on the safest way to manage your health while protecting your child, which might involve finding an alternative treatment during this important time.
One of the most important things to understand about Librium is its potential for physical dependence. This isn't the same as addiction, but it means your body gets used to the presence of the drug to function normally. This typically happens if you take it for several weeks or longer. Dependence is a predictable physiological response, not a sign of weakness. Recognizing this is the first step in managing the medication responsibly and ensuring you can stop taking it safely when the time comes, without experiencing severe withdrawal symptoms.
Never stop taking Librium abruptly. If your body has become dependent on it, a sudden stop can trigger severe withdrawal symptoms. These can include shaking, anxiety, memory problems, and even seizures. In some cases, people may experience hallucinations or have thoughts of harming themselves. To avoid this, your doctor will create a plan to slowly lower your dose over time. This tapering process gives your body a chance to adjust gradually, minimizing discomfort and keeping you safe. Always follow your doctor’s instructions for discontinuing the medication.
Finally, here are some tips to stay safe while taking Librium (as well as advice for coping with withdrawal):
And remember, Reframe is here for you as you navigate your relationship with alcohol. Join our thriving community and hear the stories of others who have been exactly where you are and know what it’s like. We wish you the best and are here to support you every step of the way.
When you're prescribed Librium, it’s essential to follow your doctor's instructions to the letter. This medication typically comes as a capsule or tablet that you swallow, and you’ll likely take it one to four times a day. You can take it with or without food, but the most important thing is consistency and adherence to the plan your healthcare provider has set out for you. Think of your doctor as your co-pilot during this process; they have the map, and following their directions ensures the smoothest and safest journey. Deviating from the prescribed dosage won't speed up your recovery and could introduce unnecessary risks.
Life happens, and sometimes a dose gets missed. If you’re taking Librium several times a day and you forget one, don't panic or try to play catch-up. The best course of action is to simply skip the dose you missed and get back on track with your next scheduled one. Whatever you do, don't take a double dose to make up for the one you forgot. Doubling up can increase the risk of side effects and won’t provide any extra benefit. Just let it go and continue with your regular schedule as if it never happened. It’s all about maintaining a steady, consistent level of the medication in your system.
It’s crucial to recognize the signs of an overdose, as this is a medical emergency that requires immediate action. If you or someone else taking Librium collapses, has a seizure, has trouble breathing, or cannot be woken up, you need to call 911 right away. These are serious symptoms that indicate the central nervous system is dangerously depressed. Don't wait to see if things improve. In these situations, every second counts, and prompt medical attention is the only safe response. Keep emergency numbers handy and make sure someone you trust is aware you are taking this medication.
Open and honest communication with your doctor is your best tool for staying safe. Before you start taking Librium, give your doctor a complete picture of your health. This includes telling them about every single thing you take — all prescription and non-prescription medicines, vitamins, and even herbal products. It’s also vital to share your medical history, especially if you’ve ever had glaucoma, seizures, or any problems with your lungs, heart, or liver. This information helps your doctor tailor your treatment plan, avoid harmful drug interactions, and ensure Librium is the right choice for you.
Once you have your prescription, handling it correctly at home is just as important as taking it correctly. Proper storage and disposal keep you and others in your home safe.
Keep your Librium in the bottle it came in, with the lid screwed on tightly, and store it somewhere out of the reach of children and pets. A medicine cabinet in a bedroom is a much better spot than one in the bathroom. You’ll want to store it at room temperature and away from excess heat and moisture, which can degrade the medication and make it less effective. The bathroom is often warm and steamy, making it a poor choice for storing most medicines.
If you have leftover Librium, don’t just toss it in the trash or flush it down the toilet. Flushing medication can contaminate the water supply. The safest way to get rid of it is through a medicine take-back program. Many pharmacies or police stations offer this service. If a take-back program isn't available, you can follow the FDA guidelines for safe disposal at home, which often involves mixing the medication with an unappealing substance like coffee grounds or cat litter before sealing it in a bag and throwing it away.
The single most important rule when taking Librium is to avoid alcohol completely. Since both substances depress the central nervous system, combining them can lead to dangerous outcomes. Your recovery journey is a partnership between you and your healthcare provider, and sticking to their instructions is key to a safe and effective outcome. Librium is a tool to help you through the acute phase of withdrawal, but it's part of a larger strategy for your well-being. Once you’re through the toughest part, you can focus on building long-term, sustainable habits with tools like the Reframe app to support your goals.
If you’ve found yourself using both Librium and alcohol, you’re far from alone. The connection between the two is more common than you might think. Because both substances work on the brain in similar ways — calming the central nervous system — people sometimes use them together to amplify that effect, or one to manage the withdrawal from the other. This overlap, however, creates a significant public health issue, leading to a higher risk of dependence, accidents, and overdose. Understanding the scale of this problem is the first step in recognizing the importance of seeking safe, effective support when you’re ready to make a change in your relationship with either substance.
The numbers paint a clear picture of how intertwined benzodiazepine and alcohol use can be. Research shows that a significant number of people with an alcohol problem also use benzodiazepines like Librium, with some estimates suggesting the overlap is between 29% and 76%. This combination is a major contributor to emergency room visits, with one report noting that benzodiazepines were involved in about 425,000 ER visits in a single year. The danger is compounded when other substances are involved; tragically, over 30% of fatal overdoses involving benzodiazepines also involve opioids, highlighting the critical risks of mixing depressant drugs.
Recognizing that you need help is a huge step, and it’s important to know that safe, effective support is available. Because of the serious risks associated with stopping both Librium and alcohol, especially if you’ve developed a dependence, trying to quit on your own is not recommended. The withdrawal process can be medically complex and even dangerous. Professional guidance ensures you can manage this transition safely and comfortably, setting you up for long-term success. The journey starts with a safe detox, but it continues with building a foundation of support and new habits for the future.
If someone is dependent on both Librium and alcohol, stopping them abruptly can be incredibly dangerous. The withdrawal symptoms can be severe, which is why 24-hour medical care is often necessary to manage the process safely. This is where Librium plays a crucial role in a controlled, clinical setting. Under a doctor’s supervision, Librium’s calming effects can help ease the intensity of alcohol withdrawal symptoms, making the transition to sobriety much more manageable. A medically supervised detox provides a secure environment where your health is the top priority, allowing your body to adjust without the life-threatening risks of quitting cold turkey.
Getting through detox is a massive accomplishment, but it’s just the beginning of the recovery process. The real work starts once your body is no longer physically dependent. It is absolutely crucial to avoid alcohol completely while on a Librium treatment plan and to follow your healthcare provider's instructions to the letter. This period is about building new coping mechanisms and a strong support system. This might include therapy, support groups, or using tools designed for habit change. Creating a sustainable, long-term plan for your well-being is what turns a successful detox into a lasting, positive change in your life.
All in all, deciding to take a break from booze — especially if Librium is in the picture — might open up exciting new possibilities. Let’s not look at it as deprivation and instead get curious about exploring life beyond booze. There’s so much to discover!
Why is mixing Librium and alcohol considered so dangerous? Think of both Librium and alcohol as substances that tell your central nervous system to slow down. When you take them together, they don't just add to each other's effects—they multiply them. This can dangerously slow your breathing and heart rate to critical levels. It’s a much riskier situation than just having too much to drink because your body's essential functions are being suppressed from two different directions at once.
So, how long do I really need to wait to drink after taking Librium? Because Librium can stay in your system for a while, the safest bet is to wait at least a few days after your last dose before even considering a drink. However, there isn't a single magic number that applies to everyone, as factors like your metabolism, dosage, and how long you were taking it all play a role. The most important step is to have an honest conversation with your doctor. They can give you a personalized and safe timeline based on your specific health situation.
I take Librium for anxiety, not alcohol withdrawal. Do the same risks with alcohol still apply? Yes, absolutely. The dangerous chemical interaction between Librium and alcohol happens regardless of why you were prescribed the medication. Your body doesn't distinguish the reason for taking it; it only processes the substances. Combining them will still lead to the same risks of extreme sedation, impaired coordination, and potentially fatal respiratory depression.
What are the immediate warning signs that someone is in trouble after mixing Librium and alcohol? You should be on high alert for signs of a potential overdose. This includes severe confusion, extreme drowsiness to the point where you can't wake them, very poor coordination or stumbling, and slowed or difficult breathing. If you notice any of these symptoms, it's a medical emergency. You need to call 911 immediately, as waiting to see if they "sleep it off" could be a fatal mistake.
If my body gets used to Librium, does that mean I'm addicted? Not necessarily, and it's important to understand the difference. Your body can develop a physical dependence on Librium, which is a predictable physiological response where it adapts to the medication's presence. This is why you should never stop taking it suddenly. Addiction, on the other hand, involves compulsive use and behaviors despite harmful consequences. Safely tapering off the medication with your doctor's guidance is designed to manage the physical dependence without causing severe withdrawal.
Alcohol withdrawal is a uniquely miserable experience. If you’ve been there, you know the feeling: drenched in sweat but shivering, with hands too shaky to even hold a glass of water. It’s a physical and mental ordeal that often requires medical help to get through safely. That’s where a medication like Librium often comes in, prescribed by doctors to calm the storm in your nervous system. But this raises a critical question, especially once the worst is over. Many people wonder, how long after taking Librium can I drink alcohol? It’s a tempting thought, but mixing the two is a dangerous game. This article will break down exactly why this combination is so risky, what happens in your body, and what you need to know before even considering a drink.
Luckily, these days we have Librium to help us out when the situation calls for it. While it was originally developed to treat anxiety, these days it’s primarily used to treat alcohol withdrawal. But what happens if you mix Librium with alcohol? Let’s look into the harmful effects of mixing these two substances.

Had history taken a different turn, Librium could have gone undiscovered, tossed into a garbage can at the Hoffmann-La Roche labs in New Jersey in 1954. As the story goes, it was discovered by accident when scientist Leo Sternbach started tinkering with a class of heretofore unknown compounds dubbed “benzheptoxdiazines.” He helped synthesize these compounds 20 years earlier but couldn’t derive any pharmacological use out of them. One of the versions he came up with — a crystalline powder labeled “Ro 5-0690” — ended up on the shelf (and almost in the garbage can, when Sternbach’s lab was getting cleaned over a year later).
As you may have guessed, this was the first version of Librium — a compound that ended up having powerful hypnotic and sedative effects in mice and acted as a potent muscle relaxer in cats. Soon enough this early benzodiazepine passed clinical trials and went from relaxing felines to quelling anxiety and insomnia in humans. Unfortunately, it also made people slur their words and lose coordination, so the interest in the drug fizzled out until it was picked up by other investigators who had better luck and eventually got it approved by the FDA in 1960.
### Chlordiazepoxide: The Generic NameWhile Librium is the name most people recognize, its generic name is chlordiazepoxide. According to MedlinePlus, "Chlordiazepoxide (Librium) is a medicine used for anxiety, pre-surgery worries, and to help with alcohol withdrawal symptoms. It's a type of calming drug called a 'benzodiazepine.'" Think of it like Tylenol versus acetaminophen — one is the brand name, and the other is the active ingredient doing the work. As the first-ever benzodiazepine, chlordiazepoxide paved the way for other well-known medications like Valium and Xanax. It works by slowing down activity in the brain, which is why it’s so effective at managing the intense symptoms that come with alcohol withdrawal.
Although it’s a go-to for managing alcohol withdrawal today, chlordiazepoxide was originally created to treat anxiety. Its calming effect on the central nervous system makes it useful for a variety of conditions beyond just helping people safely stop drinking. As MedlinePlus notes, "Chlordiazepoxide is a medicine that helps calm the brain. It is mainly used to ease anxiety. It also helps control the shaking and upset feelings that happen when someone stops drinking alcohol." This versatility is why it has remained a relevant medication for over 60 years, helping people manage both psychological and physical symptoms tied to an overactive nervous system.
Chlordiazepoxide is highly effective for short-term anxiety relief. It helps quiet the mental noise and physical restlessness that come with anxiety disorders. Interestingly, this calming effect also extends to the gut. Because of the strong connection between our brain and digestive system, chlordiazepoxide is sometimes prescribed to manage the symptoms of irritable bowel syndrome (IBS). Its ability to relax the body can soothe the stomach cramps and discomfort often triggered by stress and anxiety, offering relief when other treatments might not have worked.
It’s completely normal to feel nervous before surgery or a medical procedure. To help manage this, doctors sometimes prescribe chlordiazepoxide to ease pre-operative jitters. A dose before a procedure can help a patient relax, making the experience less stressful for them and easier for the medical team. This short-term use ensures the patient is in a calm state of mind, which can be beneficial for the procedure itself and for their overall comfort. It’s a simple and effective way to take the edge off a high-anxiety situation.
While the original patent for Librium has long expired, you’ll still find chlordiazepoxide sold under that brand name. It’s also available as a generic, which is often more affordable. You might also see it as part of a combination drug called Librax, which pairs chlordiazepoxide with clidinium to treat stomach issues like ulcers and IBS. Whether you’re prescribed the brand name or the generic, the active ingredient is the same. It typically comes in a capsule form, and the dosage will depend entirely on what you’re being treated for and your doctor’s recommendation.
Remember those slurring and stumbling early Librium patients? When we look at how Librium works at a chemical level, it’s not surprising that they seemed, well, drunk.
Just like alcohol, Librium works by enhancing the effects of a neurotransmitter in the brain called gamma-aminobutyric acid (GABA), which helps to calm nervous-system activity. Alcohol does the same (along with suppressing glutamate, its excitatory counterpart).
The result? Relaxation and tranquility. Exactly what we need when our brain chemistry is going haywire during withdrawal. Why? Because the brain is all about balance. If we’ve been drinking for a while, it gets used to the flood of GABA and suppresses its natural production. Switching gears suddenly doesn’t give it time to adjust, so replenishing our GABA with the help of Librium during the transition period makes for a much smoother ride.
Time went on, and benzodiazepines evolved as Valium, Klonopin, and Xanax came onto the scene. While these days they’re usually given preference when it comes to treating anxiety disorders, Librium has become the go-to medication for treating alcohol withdrawal (as well as presurgery anxiety).
Although it’s effective for alcohol withdrawal, taking Librium with alcohol is a whole different story.
In short, it’s not a good idea — and it could be dangerous. Here’s why:
Both Librium and alcohol are depressants that slow down the nervous system. Librium itself can cause severe drowsiness, slowing our heart rate and breathing to potentially dangerous levels.
When we mix the two substances, the downer effects get even more risky. The sedative properties are enhanced, potentially causing dangerous levels of respiratory depression, drowsiness, and dizziness. Even if we don’t stop breathing, the dizziness alone can pose a risk, especially if we’re out and about, crossing streets or operating machinery.
Librium has other side effects that don’t mix well with alcohol:
As we can see, the side effects of Librium don’t combine well with the effects of booze. But there’s even more to the story!
Both alcohol and Librium are processed by the liver, and as we know, the liver is already working overtime to process booze, so adding to its already full plate is asking for trouble.
Besides, if we’ve been drinking for a long time (let’s face it, that’s usually the context in which we get introduced to Librium to begin with), we might already be showing signs of liver disease, such as fatty liver or even cirrhosis. So let’s give it a break! (For more information, check out “How Much Alcohol Causes Liver Damage?”)
Another risk of mixing Librium with booze? We’re playing with danger when it comes to potential overdose risk. Taking both together makes overdose more likely than taking either substance alone. Here are the telltale symptoms:
If things progress, we could end up in a coma or worse. Never ignore the signs of an overdose — seek medical help right away!
What makes an overdose from this combination so dangerous is that there’s no simple fix. Unlike an opioid overdose, which can often be reversed with medication like naloxone, there’s no magic antidote for an overdose on Librium and alcohol. Since both substances are depressants that slow down your central nervous system, their combined effect can dangerously slow or even stop your breathing. Medical teams have very limited options to reverse the effects, making treatment incredibly challenging. Emergency care focuses on life support — like helping a person breathe and managing their vitals — while waiting for the body to process and clear the substances on its own. This is why it’s so critical to avoid this mix in the first place. Once an overdose happens, the situation is extremely dangerous, with very few direct treatments available.
Last but not least, both Librium and alcohol can lead to dependence. In addition to causing a surge of GABA, both trigger the release of dopamine — the so-called “reward neurotransmitter.” As the name suggests, dopamine makes us feel good — it’s a neurological “gold star” our brain rewards us with when we perform a habitual action.
While the reward system evolved to keep habits alive in order to ensure our survival, unfortunately it can’t distinguish between beneficial habits (such as socializing or eating nutritious foods) or destructive ones (such as substance use, gambling, and any other number of habits that also trigger a rush of dopamine).
With both Librium and alcohol in our system, we become more likely to fall into habitual use of either or both substances. We are also more prone to act impulsively, ending up embarrassed at best and possibly putting ourselves in serious danger. (Driving under the influence, jumping into the pool in the middle of December — whatever it is, we’re more likely to do it.) Want to know more about how dependence develops? Take a look at “Understanding Alcohol Dependence: Health Issues, Causes, and How To Overcome.”
The cognitive effects don't stop at fuzzy thinking. Librium on its own can make our memory a bit hazy, and we all know alcohol isn't great for our recall. When you put them together, their ability to disrupt memory formation is amplified, significantly increasing the risk of blackouts. This can lead to those frightening situations where you lose entire chunks of time, unable to piece together what happened or how you got home. It’s more than just forgetting a few details from the night; it’s a complete gap in your memory that can leave you feeling vulnerable and put your personal safety in serious jeopardy. The extreme sleepiness caused by this mix can even lead to passing out, which is dangerous in any situation.
On top of the memory issues, this combination can take a serious toll on our mental health. Both substances are central nervous system depressants, and mixing them can intensify feelings of sadness, hopelessness, and anxiety. Because they both affect our brain's reward system, they can also lead to unpredictable mood swings and impulsive behavior. For anyone already managing depression or other mental health conditions, this mix is especially dangerous, as it can worsen symptoms and make recovery much more difficult. It's a cycle that can be hard to break, as the low mood might make us feel like we need the substances even more. (For more on this, see our article on the link between alcohol and depression.)
If dependence develops on both substances, trying to quit them at the same time can be incredibly risky. Think of it this way: both alcohol and Librium tell your brain to calm down by working on the same neurotransmitter, GABA. When you suddenly take both away, your brain doesn't just go back to normal — it rebounds into a state of high alert. This isn't just a more intense hangover; it's a dangerous situation that can trigger severe withdrawal symptoms, including seizures, hallucinations, and delirium tremens (DTs). Because of these life-threatening risks, detoxing from both substances at once is something that should always be done under medical supervision. It’s simply not safe to go it alone.
Most doctors recommend waiting to make sure Librium is completely out of your system before considering drinking. With a long half-life that ranges anywhere from 5 to 30 hours, some of Librium’s metabolites remain in the system for quite a while, so it’s best to wait at least a few days.
That said, there might be additional considerations to keep in mind when weighing whether drinking after taking Librium is a good idea, even if it’s been a few days. If you were taking Librium for alcohol withdrawal, adding booze back into your life so soon afterwards (or at all) might not be in your best interests. Always check with your doctor first, and stick to the treatment plan you’ve chosen together!
Alcohol withdrawal can be an incredibly challenging experience, both physically and mentally, for those grappling with dependence. When someone decides to quit drinking after prolonged heavy use, their body and brain often struggle to adjust to the sudden absence of alcohol. Symptoms range from mild anxiety and tremors to severe complications like seizures and hallucinations.
In medical settings, managing these symptoms effectively is crucial, and Librium is often used to alleviate some of these uncomfortable symptoms. Librium’s calming effects help mitigate the intensity of withdrawal symptoms, providing a safer and more comfortable transition towards sobriety. However, it's important for individuals undergoing alcohol withdrawal to be under medical supervision, as the dosage and duration of Librium treatment need careful monitoring to prevent dependence on this medication.
Mixing Librium and alcohol can be extremely dangerous due to their combined depressant effects on the central nervous system. Both substances slow down brain activity and cause drowsiness, dizziness, impaired coordination, and memory problems. When taken together, they amplify each other's negative impacts. This combination increases the risk of accidents, falls, and other injuries. Moreover, mixing Librium and alcohol can lead to dangerously low blood pressure, slowed breathing, and even coma in severe cases. Additionally, both substances can be habit-forming on their own, and combining them increases the likelihood of developing dependence and addiction.
It is crucial for individuals prescribed Librium to avoid alcohol completely during treatment and to follow their healthcare provider's instructions carefully to ensure safe and effective recovery
While Librium can be a helpful tool, especially during alcohol withdrawal, it’s a powerful medication that requires respect and caution. It’s not just about avoiding alcohol; there are other important safety measures and potential side effects to be aware of. Understanding these precautions helps ensure you’re using it safely under your doctor's guidance. Think of it as having a complete user manual — knowing the ins and outs is key to a smooth and safe experience. Let's walk through what you need to know, from common side effects to specific warnings for certain situations.
Even when taken exactly as prescribed, Librium can cause side effects. Most are mild and tend to fade as your body adjusts to the medication, but it’s always good to know what to expect. Being aware of potential reactions allows you to monitor how you’re feeling and communicate effectively with your doctor. If anything feels off, don't hesitate to reach out to them. Your well-being is the top priority, and keeping an open line of communication with your healthcare provider is a crucial part of the process.
When you first start taking Librium, you might notice a few changes. The most common side effects include feeling drowsy, dizzy, or tired. Some people also experience a dry mouth, an upset stomach, or changes in their appetite. You might also feel a bit restless or notice things like constipation or blurred vision. These effects are generally not severe, but they can be bothersome. It’s important to give your body time to adapt, but if any of these side effects persist or become particularly annoying, it's a good idea to check in with your doctor.
While rare, Librium can cause more serious side effects that require immediate medical attention. Be on the lookout for symptoms like a shuffling walk, persistent shaking, or an inability to sit still. Other red flags include developing a fever, having trouble breathing or swallowing, or seeing a severe skin rash appear. Yellowing of the skin or eyes (jaundice) or an irregular heartbeat are also serious signs. If you experience any of these, you should contact your doctor or seek emergency medical help right away. Don't wait to see if they go away on their own.
Librium doesn't just interact with alcohol; it can have dangerous reactions with other substances, too. Because it's a central nervous system depressant, mixing it with other drugs that have a similar effect can amplify its sedative properties to a dangerous degree. This is why it's absolutely critical to tell your doctor about every single medication, supplement, or substance you are taking, including over-the-counter drugs and herbal remedies. This transparency allows your doctor to manage your treatment safely and avoid potentially life-threatening combinations that could compromise your health.
Mixing Librium with opioids is extremely dangerous. Both are powerful depressants that slow down your body's functions, particularly your breathing. When taken together, their combined effect is much stronger than either one alone, which can lead to severe respiratory depression — meaning your breathing can slow down to a critical level or stop altogether. This combination greatly increases the risk of a fatal overdose. It can also cause extreme drowsiness, confusion, and loss of consciousness. If you are prescribed opioids for pain, you must inform your doctor that you are also taking Librium.
Librium isn't the right choice for everyone. Certain groups of people need to be extra cautious or avoid the medication entirely due to increased risks. Your age, daily activities, and whether you are pregnant or breastfeeding all play a significant role in determining if Librium is a safe option for you. Always have an honest conversation with your doctor about your lifestyle and health history to ensure your treatment plan is tailored to your specific needs and circumstances, minimizing any potential harm while you focus on your recovery.
Because Librium can cause significant drowsiness and dizziness, you should not drive a car or operate any heavy machinery until you know how the medication affects you. Its sedative effects can impair your judgment, coordination, and reaction time, making these activities unsafe. It’s best to err on the side of caution and avoid getting behind the wheel until you and your doctor are confident that you can do so safely. Your ability to perform these tasks can be unpredictable, especially when you first start the medication.
If you are 65 or older, it’s important to discuss the risks of taking Librium with your doctor. Older adults are often more sensitive to the sedative effects of benzodiazepines, which can increase the risk of falls, confusion, and other adverse effects. Because of this, Librium is often not considered the best choice for this age group, as there may be other medications that are safer and more effective. Your doctor can help you weigh the pros and cons and determine the most appropriate course of action for your situation.
If you are pregnant, planning to become pregnant, or breastfeeding, you need to have a serious talk with your doctor before taking Librium. This medication can pass into breast milk and may cause harm to a nursing baby. Its effects during pregnancy are also a concern, so it's crucial to explore the potential risks to the fetus. Your doctor can provide guidance on the safest way to manage your health while protecting your child, which might involve finding an alternative treatment during this important time.
One of the most important things to understand about Librium is its potential for physical dependence. This isn't the same as addiction, but it means your body gets used to the presence of the drug to function normally. This typically happens if you take it for several weeks or longer. Dependence is a predictable physiological response, not a sign of weakness. Recognizing this is the first step in managing the medication responsibly and ensuring you can stop taking it safely when the time comes, without experiencing severe withdrawal symptoms.
Never stop taking Librium abruptly. If your body has become dependent on it, a sudden stop can trigger severe withdrawal symptoms. These can include shaking, anxiety, memory problems, and even seizures. In some cases, people may experience hallucinations or have thoughts of harming themselves. To avoid this, your doctor will create a plan to slowly lower your dose over time. This tapering process gives your body a chance to adjust gradually, minimizing discomfort and keeping you safe. Always follow your doctor’s instructions for discontinuing the medication.
Finally, here are some tips to stay safe while taking Librium (as well as advice for coping with withdrawal):
And remember, Reframe is here for you as you navigate your relationship with alcohol. Join our thriving community and hear the stories of others who have been exactly where you are and know what it’s like. We wish you the best and are here to support you every step of the way.
When you're prescribed Librium, it’s essential to follow your doctor's instructions to the letter. This medication typically comes as a capsule or tablet that you swallow, and you’ll likely take it one to four times a day. You can take it with or without food, but the most important thing is consistency and adherence to the plan your healthcare provider has set out for you. Think of your doctor as your co-pilot during this process; they have the map, and following their directions ensures the smoothest and safest journey. Deviating from the prescribed dosage won't speed up your recovery and could introduce unnecessary risks.
Life happens, and sometimes a dose gets missed. If you’re taking Librium several times a day and you forget one, don't panic or try to play catch-up. The best course of action is to simply skip the dose you missed and get back on track with your next scheduled one. Whatever you do, don't take a double dose to make up for the one you forgot. Doubling up can increase the risk of side effects and won’t provide any extra benefit. Just let it go and continue with your regular schedule as if it never happened. It’s all about maintaining a steady, consistent level of the medication in your system.
It’s crucial to recognize the signs of an overdose, as this is a medical emergency that requires immediate action. If you or someone else taking Librium collapses, has a seizure, has trouble breathing, or cannot be woken up, you need to call 911 right away. These are serious symptoms that indicate the central nervous system is dangerously depressed. Don't wait to see if things improve. In these situations, every second counts, and prompt medical attention is the only safe response. Keep emergency numbers handy and make sure someone you trust is aware you are taking this medication.
Open and honest communication with your doctor is your best tool for staying safe. Before you start taking Librium, give your doctor a complete picture of your health. This includes telling them about every single thing you take — all prescription and non-prescription medicines, vitamins, and even herbal products. It’s also vital to share your medical history, especially if you’ve ever had glaucoma, seizures, or any problems with your lungs, heart, or liver. This information helps your doctor tailor your treatment plan, avoid harmful drug interactions, and ensure Librium is the right choice for you.
Once you have your prescription, handling it correctly at home is just as important as taking it correctly. Proper storage and disposal keep you and others in your home safe.
Keep your Librium in the bottle it came in, with the lid screwed on tightly, and store it somewhere out of the reach of children and pets. A medicine cabinet in a bedroom is a much better spot than one in the bathroom. You’ll want to store it at room temperature and away from excess heat and moisture, which can degrade the medication and make it less effective. The bathroom is often warm and steamy, making it a poor choice for storing most medicines.
If you have leftover Librium, don’t just toss it in the trash or flush it down the toilet. Flushing medication can contaminate the water supply. The safest way to get rid of it is through a medicine take-back program. Many pharmacies or police stations offer this service. If a take-back program isn't available, you can follow the FDA guidelines for safe disposal at home, which often involves mixing the medication with an unappealing substance like coffee grounds or cat litter before sealing it in a bag and throwing it away.
The single most important rule when taking Librium is to avoid alcohol completely. Since both substances depress the central nervous system, combining them can lead to dangerous outcomes. Your recovery journey is a partnership between you and your healthcare provider, and sticking to their instructions is key to a safe and effective outcome. Librium is a tool to help you through the acute phase of withdrawal, but it's part of a larger strategy for your well-being. Once you’re through the toughest part, you can focus on building long-term, sustainable habits with tools like the Reframe app to support your goals.
If you’ve found yourself using both Librium and alcohol, you’re far from alone. The connection between the two is more common than you might think. Because both substances work on the brain in similar ways — calming the central nervous system — people sometimes use them together to amplify that effect, or one to manage the withdrawal from the other. This overlap, however, creates a significant public health issue, leading to a higher risk of dependence, accidents, and overdose. Understanding the scale of this problem is the first step in recognizing the importance of seeking safe, effective support when you’re ready to make a change in your relationship with either substance.
The numbers paint a clear picture of how intertwined benzodiazepine and alcohol use can be. Research shows that a significant number of people with an alcohol problem also use benzodiazepines like Librium, with some estimates suggesting the overlap is between 29% and 76%. This combination is a major contributor to emergency room visits, with one report noting that benzodiazepines were involved in about 425,000 ER visits in a single year. The danger is compounded when other substances are involved; tragically, over 30% of fatal overdoses involving benzodiazepines also involve opioids, highlighting the critical risks of mixing depressant drugs.
Recognizing that you need help is a huge step, and it’s important to know that safe, effective support is available. Because of the serious risks associated with stopping both Librium and alcohol, especially if you’ve developed a dependence, trying to quit on your own is not recommended. The withdrawal process can be medically complex and even dangerous. Professional guidance ensures you can manage this transition safely and comfortably, setting you up for long-term success. The journey starts with a safe detox, but it continues with building a foundation of support and new habits for the future.
If someone is dependent on both Librium and alcohol, stopping them abruptly can be incredibly dangerous. The withdrawal symptoms can be severe, which is why 24-hour medical care is often necessary to manage the process safely. This is where Librium plays a crucial role in a controlled, clinical setting. Under a doctor’s supervision, Librium’s calming effects can help ease the intensity of alcohol withdrawal symptoms, making the transition to sobriety much more manageable. A medically supervised detox provides a secure environment where your health is the top priority, allowing your body to adjust without the life-threatening risks of quitting cold turkey.
Getting through detox is a massive accomplishment, but it’s just the beginning of the recovery process. The real work starts once your body is no longer physically dependent. It is absolutely crucial to avoid alcohol completely while on a Librium treatment plan and to follow your healthcare provider's instructions to the letter. This period is about building new coping mechanisms and a strong support system. This might include therapy, support groups, or using tools designed for habit change. Creating a sustainable, long-term plan for your well-being is what turns a successful detox into a lasting, positive change in your life.
All in all, deciding to take a break from booze — especially if Librium is in the picture — might open up exciting new possibilities. Let’s not look at it as deprivation and instead get curious about exploring life beyond booze. There’s so much to discover!
Why is mixing Librium and alcohol considered so dangerous? Think of both Librium and alcohol as substances that tell your central nervous system to slow down. When you take them together, they don't just add to each other's effects—they multiply them. This can dangerously slow your breathing and heart rate to critical levels. It’s a much riskier situation than just having too much to drink because your body's essential functions are being suppressed from two different directions at once.
So, how long do I really need to wait to drink after taking Librium? Because Librium can stay in your system for a while, the safest bet is to wait at least a few days after your last dose before even considering a drink. However, there isn't a single magic number that applies to everyone, as factors like your metabolism, dosage, and how long you were taking it all play a role. The most important step is to have an honest conversation with your doctor. They can give you a personalized and safe timeline based on your specific health situation.
I take Librium for anxiety, not alcohol withdrawal. Do the same risks with alcohol still apply? Yes, absolutely. The dangerous chemical interaction between Librium and alcohol happens regardless of why you were prescribed the medication. Your body doesn't distinguish the reason for taking it; it only processes the substances. Combining them will still lead to the same risks of extreme sedation, impaired coordination, and potentially fatal respiratory depression.
What are the immediate warning signs that someone is in trouble after mixing Librium and alcohol? You should be on high alert for signs of a potential overdose. This includes severe confusion, extreme drowsiness to the point where you can't wake them, very poor coordination or stumbling, and slowed or difficult breathing. If you notice any of these symptoms, it's a medical emergency. You need to call 911 immediately, as waiting to see if they "sleep it off" could be a fatal mistake.
If my body gets used to Librium, does that mean I'm addicted? Not necessarily, and it's important to understand the difference. Your body can develop a physical dependence on Librium, which is a predictable physiological response where it adapts to the medication's presence. This is why you should never stop taking it suddenly. Addiction, on the other hand, involves compulsive use and behaviors despite harmful consequences. Safely tapering off the medication with your doctor's guidance is designed to manage the physical dependence without causing severe withdrawal.