

Holiday heart syndrome refers to an increased risk of heart-related issues during festive periods, often caused by excessive alcohol consumption, overeating, lack of exercise, stress, and sleep deprivation. Learn how to avoid holiday heart in this blog post.
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually, with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet millions of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
The holiday season is a time for celebration, indulgence, and relaxation. However, it can also spell trouble for our hearts.
What is “holiday heart”? The term was first coined in 1978 to describe a sudden increase in heart-related issues during the holiday season. However, this phenomenon is not just limited to the winter holidays — it can occur during any festive period that includes excessive eating, drinking, and stress. What are holiday heart symptoms? In this blog, we’ll explore the concept of holiday heart, its causes, and how to avoid it.
While “holiday heart syndrome” may sound lighthearted, its implications can be anything but. This condition can result in atrial fibrillation (AFib) (a rapid and irregular heartbeat that can increase the risk of stroke), heart failure, and other heart-related complications.
AFib occurs when the heart's upper chambers, the atria, beat out of sync with the lower chambers. Instead of maintaining a harmonious and coordinated contraction, the atria begin to quiver, or fibrillate, resulting in a chaotic and rapid heart rhythm. This erratic behavior isn't just a simple flutter in the chest; its ramifications can dramatically affect a person’s overall health.
Common holiday heart symptoms related to AFib include palpitations, breathlessness, and fatigue. Depending on the severity of the person’s condition, these symptoms can range from mild to debilitating. The true danger lurks beneath the surface, though. When the atria are in fibrillation, they aren't efficiently moving blood into the heart's ventricles. This inefficiency can lead to blood pooling in the atria, creating an environment conducive to clot formation.
The risk of blood clots is one of the most concerning aspects of AFib. These clots can be ejected from the heart’s chambers and travel through the bloodstream. If a clot reaches the brain, it can block vital blood flow, resulting in an ischemic stroke. Strokes can lead to an array of severe neurological consequences, from paralysis to cognitive deficits. Notably, AFib-induced strokes are often more severe and more likely to result in death compared to strokes from other causes.
Beyond stroke risk, the heart's inability to maintain a regular and effective rhythm means that it can't pump blood efficiently to the rest of the body. Over time, this inefficiency can lead to heart failure. The heart begins to weaken and can't meet the body's demand for oxygenated blood, leading to symptoms such swelling of the legs, fluid accumulation in the lungs, and chronic fatigue.
AFib doesn't exist in isolation. Its onset can trigger a domino effect of other cardiac issues. The rapid heart rates often seen in AFib can lead to other forms of arrhythmias, further complicating the clinical picture. Moreover, the persistent strain on the heart muscle can lead to myocardial remodeling, changing the heart's structure and function, making the affected person more susceptible to other heart diseases.
Furthermore, the persistent state of AFib can lead to the enlargement of the heart's chambers, especially the atria. This enlargement, known as atrial dilation, can further increase the risk of clot formation, creating a vicious cycle of increased stroke risk.
Several factors contribute to the development of holiday heart. Let’s take a look at the most common culprits.
When consumed excessively, especially in binge patterns, alcohol can lead to dehydration. This dehydration both reduces the volume of blood in circulation, making the heart work harder, and upsets the body's electrolyte balance. Electrolytes such as potassium, sodium, and calcium play pivotal roles in transmitting electrical signals across heart cells. An imbalance can render the heart's electrical system erratic, predisposing it to arrhythmias.
Furthermore, the cardiac muscle is not immune to alcohol’s toxic effects. With excessive consumption, the heart faces undue stress, leading to a state in which it's more susceptible to irregular rhythms. Intriguingly, not everyone needs to consume large volumes to experience these effects. Some people, due to genetic or physiological reasons, might be more sensitive to alcohol, experiencing symptoms with only moderate amounts.
Feasts and holidays seem almost synonymous. However, the pleasure of indulging in large, sumptuous meals can reap cardiac consequences. Foods particularly rich in salt can temporarily spike blood pressure. High blood pressure, even if transient, exerts additional pressure on the cardiac walls, potentially leading to arrhythmias.
Furthermore, fatty foods, especially those rich in saturated fats, elevate cholesterol levels, contributing to atherosclerosis — a condition in which arteries become narrowed and hardened. This can further compromise heart health. Additionally, consistent overindulgence can lead to weight gain, a prominent risk factor for both heart diseases and AFib.
Exercise plays a vital role in maintaining cardiovascular health by regulating weight, reducing blood pressure, and enhancing heart efficiency. The holiday season, coupled with the chill of winter (for northern hemisphere folks), can lead many of us away from our exercise routines.
Abandoning physical activity can lead to weight gain, pushing the heart to work harder. High blood pressure and reduced cardiac efficiency, common consequences of a sedentary lifestyle, set the stage for conditions such as holiday heart syndrome.
Holidays, while celebratory, come with their share of stressors: the pressures of perfecting celebrations, managing finances, and navigating complex family dynamics. This heightened stress stimulates the adrenal glands to release hormones such as cortisol and adrenaline.
Elevated levels of these hormones increase heart rate and blood pressure — factors known to cause arrhythmias. Moreover, chronic stress can lead to inflammation, further jeopardizing heart health.
Sleep is the body's natural reset button, especially for the cardiovascular system. Holidays often bring with them late-night revelries, travel across time zones, or simply the anxiety of preparations, all of which can upset regular sleep patterns.
A sleep-deprived body struggles to regulate stress hormones, leading to increased blood pressure and heart rate. Fatigue and irritability stemming from poor sleep can further escalate stress, creating a feedback loop detrimental to heart health.

In most cases, the symptoms of HHS (including palpitations, shortness of breath, or a feeling of unease in the chest) manifest within a few hours to 48 hours after heavy alcohol consumption. Their duration can vary significantly from person to person.
For many, holiday heart syndrome is transient, lasting only a few hours to a couple of days. With adequate rest, hydration, and abstaining from further alcohol or triggering foods, the heart often corrects its rhythm spontaneously, returning to its baseline state without medical intervention. This brief manifestation of holiday heart, especially in those who experience it for the first time, can make it seem unproblematic. However, even transient episodes can have implications for future cardiac health.
In some people, especially those with pre-existing heart conditions or those who have had recurrent episodes of holiday heart syndrome, the irregular rhythm might persist. AFib or other arrhythmias could continue for several days or even weeks, requiring medical intervention. In these cases, healthcare professionals might use medication or electrical cardioversion to restore the heart's normal rhythm.
It's worth noting that even after the heart's rhythm normalizes, some residual effects of holiday heart syndrome might linger. People may feel fatigued, experience bouts of dizziness, or have a general sense of malaise for a few days after the episode.
Finally, and perhaps most critically, if repeated, even brief episodes of holiday heart syndrome can reshape the heart's electrical framework. The more frequently we experience holiday heart syndrome, the more predisposed we become to potentially more dangerous episodes in the future. This cumulative effect underscores the importance of recognizing and addressing the syndrome early.
While the holiday season can be a time of increased risk for heart-related issues, you can protect your heart and enjoy the festivities without worry. Here are some tips for preventing holiday heart.
Alcohol, while a staple in many celebrations, can slowly take a toll on our heart. Moderation is key! The Centers for Disease Control and Prevention (CDC) has guidelines that recommend no more than one to two alcoholic drinks per day for men and one drink per day for women. Staying within these boundaries shields our heart (and prevents a myriad of other alcohol-related complications!).
Binge drinking, characterized by consuming an excessive amount of alcohol in a short time frame, is particularly detrimental. It can lead to dehydration, electrolyte imbalances, and a transient spike in blood pressure, all of which strain the heart. If alcohol is a part of your holiday festivities, pacing your consumption and interspersing with water can make a significant difference.
Holiday feasts can tempt us to eat more than we’d intended. While indulgence is part of the celebrations, a discerning approach to food choices can stave off potential cardiac repercussions. Foods loaded with excessive fats and salt can acutely raise blood pressure and increase the heart’s workload.
Mindfulness during meals involves being cognizant of portion sizes, savoring each bite, and recognizing satiety cues. Prioritizing fresh, whole foods and limiting processed, high-sodium options can be a game-changer. Additionally, eating substantial meals late into the night can exacerbate reflux and strain the heart, making timing as crucial as the food choices.
The festive season often disrupts regular exercise routines. Physical activity is paramount in safeguarding cardiovascular health. The American Heart Association recommends at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity each week.
Holiday fitness doesn't have to be a structured gym session. Integrating activity into celebrations — a post-feast stroll, dancing the night away, or even participating in themed fun runs — ensures that the heart remains safe.
The holidays, ironically, often come riddled with stress. From the pressures of executing perfect celebrations to managing year-end deadlines, stress can spike cortisol levels, inadvertently increasing our heart rate and blood pressure. Embracing relaxation techniques such as deep breathing, meditation, or even simple mindfulness practices can mitigate these effects. Setting realistic expectations, delegating tasks, and leaning on loved ones for support can also help diffuse holiday pressures.
Sleep is the body's natural restorative. Amid the holiday chaos, carve out your regular (we hope!) seven to nine hours of quality sleep. Practice the same good sleep hygiene during the holidays that you practice the rest of the year: regularizing sleep patterns, cultivating a serene bedtime environment, and minimizing screen time before bed. A rested body ensures the heart functions optimally, ready to participate in the festivities with vigor.
Holiday heart syndrome is a real phenomenon that can put a damper on your festive celebrations. By understanding the causes and taking steps to prevent it, you can protect your heart and enjoy the holiday season without worry. Remember to practice moderation, maintain a healthy lifestyle, and prioritize self-care during this busy time of year. Doing so not only reduces your risk of holiday heart — it also sets yourself up for a healthier, happier new year.
The holiday season is a time for celebration, indulgence, and relaxation. However, it can also spell trouble for our hearts.
What is “holiday heart”? The term was first coined in 1978 to describe a sudden increase in heart-related issues during the holiday season. However, this phenomenon is not just limited to the winter holidays — it can occur during any festive period that includes excessive eating, drinking, and stress. What are holiday heart symptoms? In this blog, we’ll explore the concept of holiday heart, its causes, and how to avoid it.
While “holiday heart syndrome” may sound lighthearted, its implications can be anything but. This condition can result in atrial fibrillation (AFib) (a rapid and irregular heartbeat that can increase the risk of stroke), heart failure, and other heart-related complications.
AFib occurs when the heart's upper chambers, the atria, beat out of sync with the lower chambers. Instead of maintaining a harmonious and coordinated contraction, the atria begin to quiver, or fibrillate, resulting in a chaotic and rapid heart rhythm. This erratic behavior isn't just a simple flutter in the chest; its ramifications can dramatically affect a person’s overall health.
Common holiday heart symptoms related to AFib include palpitations, breathlessness, and fatigue. Depending on the severity of the person’s condition, these symptoms can range from mild to debilitating. The true danger lurks beneath the surface, though. When the atria are in fibrillation, they aren't efficiently moving blood into the heart's ventricles. This inefficiency can lead to blood pooling in the atria, creating an environment conducive to clot formation.
The risk of blood clots is one of the most concerning aspects of AFib. These clots can be ejected from the heart’s chambers and travel through the bloodstream. If a clot reaches the brain, it can block vital blood flow, resulting in an ischemic stroke. Strokes can lead to an array of severe neurological consequences, from paralysis to cognitive deficits. Notably, AFib-induced strokes are often more severe and more likely to result in death compared to strokes from other causes.
Beyond stroke risk, the heart's inability to maintain a regular and effective rhythm means that it can't pump blood efficiently to the rest of the body. Over time, this inefficiency can lead to heart failure. The heart begins to weaken and can't meet the body's demand for oxygenated blood, leading to symptoms such swelling of the legs, fluid accumulation in the lungs, and chronic fatigue.
AFib doesn't exist in isolation. Its onset can trigger a domino effect of other cardiac issues. The rapid heart rates often seen in AFib can lead to other forms of arrhythmias, further complicating the clinical picture. Moreover, the persistent strain on the heart muscle can lead to myocardial remodeling, changing the heart's structure and function, making the affected person more susceptible to other heart diseases.
Furthermore, the persistent state of AFib can lead to the enlargement of the heart's chambers, especially the atria. This enlargement, known as atrial dilation, can further increase the risk of clot formation, creating a vicious cycle of increased stroke risk.
Several factors contribute to the development of holiday heart. Let’s take a look at the most common culprits.
When consumed excessively, especially in binge patterns, alcohol can lead to dehydration. This dehydration both reduces the volume of blood in circulation, making the heart work harder, and upsets the body's electrolyte balance. Electrolytes such as potassium, sodium, and calcium play pivotal roles in transmitting electrical signals across heart cells. An imbalance can render the heart's electrical system erratic, predisposing it to arrhythmias.
Furthermore, the cardiac muscle is not immune to alcohol’s toxic effects. With excessive consumption, the heart faces undue stress, leading to a state in which it's more susceptible to irregular rhythms. Intriguingly, not everyone needs to consume large volumes to experience these effects. Some people, due to genetic or physiological reasons, might be more sensitive to alcohol, experiencing symptoms with only moderate amounts.
Feasts and holidays seem almost synonymous. However, the pleasure of indulging in large, sumptuous meals can reap cardiac consequences. Foods particularly rich in salt can temporarily spike blood pressure. High blood pressure, even if transient, exerts additional pressure on the cardiac walls, potentially leading to arrhythmias.
Furthermore, fatty foods, especially those rich in saturated fats, elevate cholesterol levels, contributing to atherosclerosis — a condition in which arteries become narrowed and hardened. This can further compromise heart health. Additionally, consistent overindulgence can lead to weight gain, a prominent risk factor for both heart diseases and AFib.
Exercise plays a vital role in maintaining cardiovascular health by regulating weight, reducing blood pressure, and enhancing heart efficiency. The holiday season, coupled with the chill of winter (for northern hemisphere folks), can lead many of us away from our exercise routines.
Abandoning physical activity can lead to weight gain, pushing the heart to work harder. High blood pressure and reduced cardiac efficiency, common consequences of a sedentary lifestyle, set the stage for conditions such as holiday heart syndrome.
Holidays, while celebratory, come with their share of stressors: the pressures of perfecting celebrations, managing finances, and navigating complex family dynamics. This heightened stress stimulates the adrenal glands to release hormones such as cortisol and adrenaline.
Elevated levels of these hormones increase heart rate and blood pressure — factors known to cause arrhythmias. Moreover, chronic stress can lead to inflammation, further jeopardizing heart health.
Sleep is the body's natural reset button, especially for the cardiovascular system. Holidays often bring with them late-night revelries, travel across time zones, or simply the anxiety of preparations, all of which can upset regular sleep patterns.
A sleep-deprived body struggles to regulate stress hormones, leading to increased blood pressure and heart rate. Fatigue and irritability stemming from poor sleep can further escalate stress, creating a feedback loop detrimental to heart health.

In most cases, the symptoms of HHS (including palpitations, shortness of breath, or a feeling of unease in the chest) manifest within a few hours to 48 hours after heavy alcohol consumption. Their duration can vary significantly from person to person.
For many, holiday heart syndrome is transient, lasting only a few hours to a couple of days. With adequate rest, hydration, and abstaining from further alcohol or triggering foods, the heart often corrects its rhythm spontaneously, returning to its baseline state without medical intervention. This brief manifestation of holiday heart, especially in those who experience it for the first time, can make it seem unproblematic. However, even transient episodes can have implications for future cardiac health.
In some people, especially those with pre-existing heart conditions or those who have had recurrent episodes of holiday heart syndrome, the irregular rhythm might persist. AFib or other arrhythmias could continue for several days or even weeks, requiring medical intervention. In these cases, healthcare professionals might use medication or electrical cardioversion to restore the heart's normal rhythm.
It's worth noting that even after the heart's rhythm normalizes, some residual effects of holiday heart syndrome might linger. People may feel fatigued, experience bouts of dizziness, or have a general sense of malaise for a few days after the episode.
Finally, and perhaps most critically, if repeated, even brief episodes of holiday heart syndrome can reshape the heart's electrical framework. The more frequently we experience holiday heart syndrome, the more predisposed we become to potentially more dangerous episodes in the future. This cumulative effect underscores the importance of recognizing and addressing the syndrome early.
While the holiday season can be a time of increased risk for heart-related issues, you can protect your heart and enjoy the festivities without worry. Here are some tips for preventing holiday heart.
Alcohol, while a staple in many celebrations, can slowly take a toll on our heart. Moderation is key! The Centers for Disease Control and Prevention (CDC) has guidelines that recommend no more than one to two alcoholic drinks per day for men and one drink per day for women. Staying within these boundaries shields our heart (and prevents a myriad of other alcohol-related complications!).
Binge drinking, characterized by consuming an excessive amount of alcohol in a short time frame, is particularly detrimental. It can lead to dehydration, electrolyte imbalances, and a transient spike in blood pressure, all of which strain the heart. If alcohol is a part of your holiday festivities, pacing your consumption and interspersing with water can make a significant difference.
Holiday feasts can tempt us to eat more than we’d intended. While indulgence is part of the celebrations, a discerning approach to food choices can stave off potential cardiac repercussions. Foods loaded with excessive fats and salt can acutely raise blood pressure and increase the heart’s workload.
Mindfulness during meals involves being cognizant of portion sizes, savoring each bite, and recognizing satiety cues. Prioritizing fresh, whole foods and limiting processed, high-sodium options can be a game-changer. Additionally, eating substantial meals late into the night can exacerbate reflux and strain the heart, making timing as crucial as the food choices.
The festive season often disrupts regular exercise routines. Physical activity is paramount in safeguarding cardiovascular health. The American Heart Association recommends at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity each week.
Holiday fitness doesn't have to be a structured gym session. Integrating activity into celebrations — a post-feast stroll, dancing the night away, or even participating in themed fun runs — ensures that the heart remains safe.
The holidays, ironically, often come riddled with stress. From the pressures of executing perfect celebrations to managing year-end deadlines, stress can spike cortisol levels, inadvertently increasing our heart rate and blood pressure. Embracing relaxation techniques such as deep breathing, meditation, or even simple mindfulness practices can mitigate these effects. Setting realistic expectations, delegating tasks, and leaning on loved ones for support can also help diffuse holiday pressures.
Sleep is the body's natural restorative. Amid the holiday chaos, carve out your regular (we hope!) seven to nine hours of quality sleep. Practice the same good sleep hygiene during the holidays that you practice the rest of the year: regularizing sleep patterns, cultivating a serene bedtime environment, and minimizing screen time before bed. A rested body ensures the heart functions optimally, ready to participate in the festivities with vigor.
Holiday heart syndrome is a real phenomenon that can put a damper on your festive celebrations. By understanding the causes and taking steps to prevent it, you can protect your heart and enjoy the holiday season without worry. Remember to practice moderation, maintain a healthy lifestyle, and prioritize self-care during this busy time of year. Doing so not only reduces your risk of holiday heart — it also sets yourself up for a healthier, happier new year.

Navigating the world of autoimmune diseases and alcohol is tricky, but science shows that the increase in inflammation spells trouble for conditions such as Lupus, psoriasis, Celiac disease, MS, and Type 1 Diabetes.
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually, with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet millions of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app today!
It’s Friday night. Ah, the magical allure of the weekend after a long work week! You're sitting in your cozy home, finally unwinding, staring at that inviting bottle of your favorite cabernet. But there's a tiny voice whispering at the back of your mind: “What about that autoimmune disease?” Can you really partake? While it’s always a good idea to check with a healthcare provider first, there are some common patterns when it comes to alcohol and autoimmune diseases. Let’s find out more!
Let's begin by understanding autoimmune diseases. These conditions flare up when our immune system — usually our trusty guardian against viruses and bacteria — gets a little confused. It mistakes our healthy cells for foreign invaders and attacks them accordingly. It’s as if the trusty guard dog suddenly sees the mail carrier as an intruder!
There are over 80 types of autoimmune diseases. Some, like rheumatoid arthritis and lupus, can affect many parts of the body. Others, such as type 1 diabetes and psoriasis, are more specific. Managing these diseases often requires a careful balancing act of lifestyle, diet, medication, and yes — our Friday night libations.
Autoimmune diseases thrive on inflammation. Here's where it gets tricky. Alcohol, in moderate amounts, can have an anti-inflammatory effect. Sounds good, right? Not so fast! Remember, the key word here is "moderate.” Higher amounts of alcohol consumption can lead to chronic inflammation, exacerbating autoimmune diseases.
It's also important to remember that many autoimmune diseases have organ-specific effects. For example, in autoimmune liver disease, consuming alcohol can cause more harm, accelerating liver damage. Similarly, autoimmune diseases that affect the digestive system — such as Crohn's or celiac disease — don’t mix well with alcohol, which can irritate the digestive tract.
In a nutshell, while a glass of wine might not spell disaster for everyone with an autoimmune disease, the effects of alcohol can vary widely depending on the type and severity of the autoimmune disease, the amount and frequency of alcohol intake, and individual genetic factors.
Rheumatoid arthritis (RA) isn’t your average joint pain. In this chronic autoimmune condition, the immune system mistakenly attacks the joints, leading to inflammation, swelling, and pain. Over time, it can damage joints and even cause joint deformity. RA can also affect other parts of the body including the skin, eyes, lungs, heart, and blood vessels.
Here are some common symptoms of RA:
So, where does alcohol fit into the RA picture? There’s good news here: research shows that moderate alcohol consumption won’t increase symptoms for those who already have the disease. But again, the key word is “moderate” — so no more than one drink in a sitting for women and no more than two drinks for men, according to the CDC’s definition of moderate drinking.
In spite of the low risk associated with moderate drinking and RA, alcohol can interfere with medications commonly used to treat it, such as methotrexate. Mixing alcohol and RA medications can heighten the risk of liver problems and diminish the medication's effectiveness.
Moreover, while alcohol might be anti-inflammatory, it can also cause dehydration which might exacerbate RA symptoms.
First things first, what is lupus? Like other autoimmune diseases, lupus develops when the immune system turns against parts of the body it's designed to protect, leading to inflammation and damage to various body tissues. Lupus can affect the joints, skin, kidneys, blood cells, brain, heart, and lungs. Think of it like an overeager security system that's a bit too enthusiastic, mistaking friendly visitors (the body's cells) for intruders.
Lupus can be a bit of a chameleon, presenting a range of symptoms that often mimic other ailments. Lupus has some common indicators:
How does alcohol play with lupus? Can you drink with lupus? Alcohol and lupus together is kind of a mixed bag. The main concern is that alcohol can interact negatively with medications that are often prescribed to treat lupus, such as non-steroidal anti-inflammatory drugs (NSAIDs), antimalarials, and corticosteroids. Combining alcohol with these medications can increase the risk of liver complications and stomach bleeding. Alcohol can also amplify the side effects of these meds, making us feel more tired or dizzy.
Does alcohol cause joint inflammation? Alcohol can exacerbate lupus-related skin flares, especially for someone who is sensitive. Plus, alcohol may exacerbate symptoms such as fatigue and joint pain, adding fuel to the lupus fire.
The lupus-alcohol equation isn't one-size-fits-all. It's about knowledge, understanding your body, and making choices that support your well-being.
Multiple sclerosis, commonly known as MS, is a chronic autoimmune disease that affects the central nervous system. Once again, the body's defense system gets a bit too overzealous. In this case, it starts damaging the protective covering of nerve fibers (called myelin), leading to communication issues between the brain and the rest of the body.
MS can also lead to a range of symptoms that differ from person to person, but these are some common signs:
When it comes to MS and alcohol, things can get tricky. MS already stirs up issues with balance and coordination, and — as we all know — alcohol does, too. Plus, alcohol may not play nice with certain MS medications, so that's another hurdle to watch out for.
Moderate alcohol consumption does not appear to increase the risk of developing MS, nor does it seem to influence disease progression. However, the keyword here, once again, is "moderate." Binge drinking or consistent heavy drinking can have adverse effects on anyone's health, and with MS, the risks might be even more pronounced.
Psoriasis is an autoimmune condition caused by accelerated skin cell growth, which causes thick, red, scaly patches to form on the skin. These patches can be itchy and sometimes painful. Imagine the skin's production line going into overdrive, causing a pile-up of cells on the surface. That is psoriasis in action.
Psoriasis can manifest in various forms, but here are some common signs:
Alcohol and psoriasis can be a tricky combination. Excessive alcohol consumption is known to trigger psoriasis outbreaks for some people. It can also interfere with the body's ability to process and eliminate medications used to treat psoriasis, rendering them less effective.
Moreover, alcohol can dehydrate the body, including the skin, possibly making psoriasis symptoms worse. And, in some cases, alcohol has been known to have an inflammatory effect which may potentially flare up psoriasis patches.
Alcohol consumption, especially in excess, can trigger psoriasis flares and worsen symptoms. That’s why it’s essential for those living with this condition to drink mindfully and consider healthier options such as mocktails.
Type 1 diabetes is an autoimmune condition caused by the immune system mistakenly attacking and destroying the insulin-producing beta cells in the pancreas. Insulin allows glucose (sugar) from our food to enter our cells and provide energy. Without enough insulin, glucose builds up in the bloodstream, leading to high blood sugar levels.
Type 1 diabetes has some hallmark symptoms:
What happens when type 1 diabetes and alcohol mix? This is a pairing that needs careful attention.
Alcohol can interfere with the liver's ability to release glucose, increasing the risk of low blood sugar (hypoglycemia) for those with type 1 diabetes. While it might initially elevate blood sugar, it can drop later on, especially if we’re taking insulin or other diabetes medications.
Additionally, many alcoholic beverages, especially cocktails, contain sugars and carbs that can spike blood sugar levels. It's essential to factor in these carbs as part of our overall daily intake.
Symptoms of hypoglycemia can sometimes mirror the effects of too much alcohol: dizziness, disorientation, and sleepiness. This can make it challenging for those around us to distinguish between intoxication and a medical emergency.
When navigating the alcohol-diabetes combo, keep these points in mind:
Alcohol consumption, especially in excess, can mess with blood sugar and be potentially dangerous for those living with type 1 diabetes. Always consult with a healthcare provider, such as an endocrinologist, before imbibing when living with this condition.
Finally, celiac disease is an autoimmune condition triggered by gluten — a protein found in wheat, barley, and rye — that leads to damage in the small intestine when ingested by those who are sensitive to it. The body misinterprets gluten as a harmful invader and prompts the immune system to attack the inner lining of the small intestine, disrupting the absorption of vital nutrients.
Celiac can be a bit sneaky, presenting a wide array of symptoms. These are some of the common signs to look out for:
Where does alcohol stand in the world of celiac disease? Here’s the scoop.
The primary concern with celiac disease and alcohol is the source of the alcohol. Many alcoholic beverages, including beers, ales, lagers, malt beverages, and even some hard ciders, contain gluten. Consuming these would be a no-go for someone with celiac disease.
However, pure distilled spirits, even if they're made from wheat, barley, or rye, are considered gluten-free due to the distillation process. This means spirits like vodka, gin, and whiskey might be safe. Similarly, wines and some ciders are naturally gluten-free and safe for most people with celiac disease. But always read labels or check with manufacturers when in doubt.
Considering a drink and living with celiac disease? Here's the mantra: be informed and vigilant. Not all alcoholic beverages will label their gluten content, so doing a bit of homework might be necessary. Additionally, always listen to your body; even gluten-free options might not sit well with everyone.

Well, as you can see, there's really no one-size-fits-all answer here. It all depends on the specific autoimmune disease, your overall health, and the type and amount of alcohol consumed. It’s essential to talk to professionals and take all these factors into consideration to make an informed decision.
As you figure out how alcohol fits into your life — and whether or not it’s ultimately a no-go because of your autoimmune disease — here are some practical steps to navigate this journey:
All in all, understanding the interaction between autoimmune diseases and alcohol can be tricky, but ultimately it comes down to understanding your body’s unique needs. It requires patience, discernment, and an appreciation for the nuances. And remember —you're not alone!
Whether we're raising a glass of bubbly or a cup of herbal tea, let's toast to knowledge, health, and the confidence to make the best choices for our wellness.
It’s Friday night. Ah, the magical allure of the weekend after a long work week! You're sitting in your cozy home, finally unwinding, staring at that inviting bottle of your favorite cabernet. But there's a tiny voice whispering at the back of your mind: “What about that autoimmune disease?” Can you really partake? While it’s always a good idea to check with a healthcare provider first, there are some common patterns when it comes to alcohol and autoimmune diseases. Let’s find out more!
Let's begin by understanding autoimmune diseases. These conditions flare up when our immune system — usually our trusty guardian against viruses and bacteria — gets a little confused. It mistakes our healthy cells for foreign invaders and attacks them accordingly. It’s as if the trusty guard dog suddenly sees the mail carrier as an intruder!
There are over 80 types of autoimmune diseases. Some, like rheumatoid arthritis and lupus, can affect many parts of the body. Others, such as type 1 diabetes and psoriasis, are more specific. Managing these diseases often requires a careful balancing act of lifestyle, diet, medication, and yes — our Friday night libations.
Autoimmune diseases thrive on inflammation. Here's where it gets tricky. Alcohol, in moderate amounts, can have an anti-inflammatory effect. Sounds good, right? Not so fast! Remember, the key word here is "moderate.” Higher amounts of alcohol consumption can lead to chronic inflammation, exacerbating autoimmune diseases.
It's also important to remember that many autoimmune diseases have organ-specific effects. For example, in autoimmune liver disease, consuming alcohol can cause more harm, accelerating liver damage. Similarly, autoimmune diseases that affect the digestive system — such as Crohn's or celiac disease — don’t mix well with alcohol, which can irritate the digestive tract.
In a nutshell, while a glass of wine might not spell disaster for everyone with an autoimmune disease, the effects of alcohol can vary widely depending on the type and severity of the autoimmune disease, the amount and frequency of alcohol intake, and individual genetic factors.
Rheumatoid arthritis (RA) isn’t your average joint pain. In this chronic autoimmune condition, the immune system mistakenly attacks the joints, leading to inflammation, swelling, and pain. Over time, it can damage joints and even cause joint deformity. RA can also affect other parts of the body including the skin, eyes, lungs, heart, and blood vessels.
Here are some common symptoms of RA:
So, where does alcohol fit into the RA picture? There’s good news here: research shows that moderate alcohol consumption won’t increase symptoms for those who already have the disease. But again, the key word is “moderate” — so no more than one drink in a sitting for women and no more than two drinks for men, according to the CDC’s definition of moderate drinking.
In spite of the low risk associated with moderate drinking and RA, alcohol can interfere with medications commonly used to treat it, such as methotrexate. Mixing alcohol and RA medications can heighten the risk of liver problems and diminish the medication's effectiveness.
Moreover, while alcohol might be anti-inflammatory, it can also cause dehydration which might exacerbate RA symptoms.
First things first, what is lupus? Like other autoimmune diseases, lupus develops when the immune system turns against parts of the body it's designed to protect, leading to inflammation and damage to various body tissues. Lupus can affect the joints, skin, kidneys, blood cells, brain, heart, and lungs. Think of it like an overeager security system that's a bit too enthusiastic, mistaking friendly visitors (the body's cells) for intruders.
Lupus can be a bit of a chameleon, presenting a range of symptoms that often mimic other ailments. Lupus has some common indicators:
How does alcohol play with lupus? Can you drink with lupus? Alcohol and lupus together is kind of a mixed bag. The main concern is that alcohol can interact negatively with medications that are often prescribed to treat lupus, such as non-steroidal anti-inflammatory drugs (NSAIDs), antimalarials, and corticosteroids. Combining alcohol with these medications can increase the risk of liver complications and stomach bleeding. Alcohol can also amplify the side effects of these meds, making us feel more tired or dizzy.
Does alcohol cause joint inflammation? Alcohol can exacerbate lupus-related skin flares, especially for someone who is sensitive. Plus, alcohol may exacerbate symptoms such as fatigue and joint pain, adding fuel to the lupus fire.
The lupus-alcohol equation isn't one-size-fits-all. It's about knowledge, understanding your body, and making choices that support your well-being.
Multiple sclerosis, commonly known as MS, is a chronic autoimmune disease that affects the central nervous system. Once again, the body's defense system gets a bit too overzealous. In this case, it starts damaging the protective covering of nerve fibers (called myelin), leading to communication issues between the brain and the rest of the body.
MS can also lead to a range of symptoms that differ from person to person, but these are some common signs:
When it comes to MS and alcohol, things can get tricky. MS already stirs up issues with balance and coordination, and — as we all know — alcohol does, too. Plus, alcohol may not play nice with certain MS medications, so that's another hurdle to watch out for.
Moderate alcohol consumption does not appear to increase the risk of developing MS, nor does it seem to influence disease progression. However, the keyword here, once again, is "moderate." Binge drinking or consistent heavy drinking can have adverse effects on anyone's health, and with MS, the risks might be even more pronounced.
Psoriasis is an autoimmune condition caused by accelerated skin cell growth, which causes thick, red, scaly patches to form on the skin. These patches can be itchy and sometimes painful. Imagine the skin's production line going into overdrive, causing a pile-up of cells on the surface. That is psoriasis in action.
Psoriasis can manifest in various forms, but here are some common signs:
Alcohol and psoriasis can be a tricky combination. Excessive alcohol consumption is known to trigger psoriasis outbreaks for some people. It can also interfere with the body's ability to process and eliminate medications used to treat psoriasis, rendering them less effective.
Moreover, alcohol can dehydrate the body, including the skin, possibly making psoriasis symptoms worse. And, in some cases, alcohol has been known to have an inflammatory effect which may potentially flare up psoriasis patches.
Alcohol consumption, especially in excess, can trigger psoriasis flares and worsen symptoms. That’s why it’s essential for those living with this condition to drink mindfully and consider healthier options such as mocktails.
Type 1 diabetes is an autoimmune condition caused by the immune system mistakenly attacking and destroying the insulin-producing beta cells in the pancreas. Insulin allows glucose (sugar) from our food to enter our cells and provide energy. Without enough insulin, glucose builds up in the bloodstream, leading to high blood sugar levels.
Type 1 diabetes has some hallmark symptoms:
What happens when type 1 diabetes and alcohol mix? This is a pairing that needs careful attention.
Alcohol can interfere with the liver's ability to release glucose, increasing the risk of low blood sugar (hypoglycemia) for those with type 1 diabetes. While it might initially elevate blood sugar, it can drop later on, especially if we’re taking insulin or other diabetes medications.
Additionally, many alcoholic beverages, especially cocktails, contain sugars and carbs that can spike blood sugar levels. It's essential to factor in these carbs as part of our overall daily intake.
Symptoms of hypoglycemia can sometimes mirror the effects of too much alcohol: dizziness, disorientation, and sleepiness. This can make it challenging for those around us to distinguish between intoxication and a medical emergency.
When navigating the alcohol-diabetes combo, keep these points in mind:
Alcohol consumption, especially in excess, can mess with blood sugar and be potentially dangerous for those living with type 1 diabetes. Always consult with a healthcare provider, such as an endocrinologist, before imbibing when living with this condition.
Finally, celiac disease is an autoimmune condition triggered by gluten — a protein found in wheat, barley, and rye — that leads to damage in the small intestine when ingested by those who are sensitive to it. The body misinterprets gluten as a harmful invader and prompts the immune system to attack the inner lining of the small intestine, disrupting the absorption of vital nutrients.
Celiac can be a bit sneaky, presenting a wide array of symptoms. These are some of the common signs to look out for:
Where does alcohol stand in the world of celiac disease? Here’s the scoop.
The primary concern with celiac disease and alcohol is the source of the alcohol. Many alcoholic beverages, including beers, ales, lagers, malt beverages, and even some hard ciders, contain gluten. Consuming these would be a no-go for someone with celiac disease.
However, pure distilled spirits, even if they're made from wheat, barley, or rye, are considered gluten-free due to the distillation process. This means spirits like vodka, gin, and whiskey might be safe. Similarly, wines and some ciders are naturally gluten-free and safe for most people with celiac disease. But always read labels or check with manufacturers when in doubt.
Considering a drink and living with celiac disease? Here's the mantra: be informed and vigilant. Not all alcoholic beverages will label their gluten content, so doing a bit of homework might be necessary. Additionally, always listen to your body; even gluten-free options might not sit well with everyone.

Well, as you can see, there's really no one-size-fits-all answer here. It all depends on the specific autoimmune disease, your overall health, and the type and amount of alcohol consumed. It’s essential to talk to professionals and take all these factors into consideration to make an informed decision.
As you figure out how alcohol fits into your life — and whether or not it’s ultimately a no-go because of your autoimmune disease — here are some practical steps to navigate this journey:
All in all, understanding the interaction between autoimmune diseases and alcohol can be tricky, but ultimately it comes down to understanding your body’s unique needs. It requires patience, discernment, and an appreciation for the nuances. And remember —you're not alone!
Whether we're raising a glass of bubbly or a cup of herbal tea, let's toast to knowledge, health, and the confidence to make the best choices for our wellness.

Alcohol can wreak havoc on our digestive system, causing heartburn, damaging the stomach lining, inflaming the pancreas, disrupting nutrient absorption, and upsetting the balance of bacteria in the large intestine. However, through gradual reduction of alcohol intake, hydration, a nutrient-rich diet, and regular exercise, we can help our bodies heal and promote a healthier digestive system.
If you’re ready to give your stomach — as well as the rest of your body and mind — a break from alcohol, Reframe is here to help! While the Reframe app isn’t a cure for alcohol use disorder (AUD), it serves as a useful tool to help you rethink the role of alcohol in your life in an intuitive way that is backed by neuroscience. Hundreds of thousands of people around the world have found our method to be useful in curbing their drinking habits, and we believe you can, too!
Reframe is designed to provide you with the necessary knowledge and skills that enable you not just to survive with reduced alcohol intake but to flourish throughout this journey. We offer daily readings backed by research, enlightening you on the neuroscience of alcohol, and an in-app Toolkit filled with useful resources and activities to overcome each hurdle.
Join a global community of Reframers on our 24/7 Forum chat to gain motivation from people worldwide who can empathize with your experiences. You can engage with our certified coaches for personalized advice and guidance.
To enhance your user experience, we continually update our app with novel features. Our latest addition is an in-app chatbot, Melody, powered by the most advanced AI technology. Melody is here to assist you as you transition towards a life with less alcohol — or none at all.
And there’s more! Each month, we present engaging challenges, such as Dry/Damp January, Mental Health May, and Outdoorsy June. Participate with fellow Reframers or individually — the choice is yours!
You can try the Reframe app for free for seven days. Why wait when there's nothing to lose? Are you prepared to take control and explore life beyond alcohol? Download our app today!
In the words of Nancy Mure, “In understanding the basics of digestion, you'll discover who's in charge. Here's a hint. It's not you.”
When all is well, we don’t give digestion much thought. However, as soon as problems arise, it’s hard to think about anything else. For many, stomach pain after drinking alcohol is a recurring problem, while others experience lower abdominal pain after drinking alcohol. So, how does alcohol affect the digestive system? What does alcohol do to your stomach? Does wine help with digestion? Are there any digestive problems caused by alcohol or stomach issues from alcohol misuse? And what is the connection between alcohol and gut health? If you’ve ever wondered what causes stomach inflammation or wanted to explore the link between alcohol and gastritis, alcohol and IBS, alcohol and ulcers, or alcohol and digestive cancer, it’s time to dig deeper. Let’s look at the connection more closely by examining five ways in which alcohol affects the stomach and digestive system.

Let’s take a brief tour through the digestive system to see what happens when alcohol enters the scene to understand the link between alcohol and digestive issues and find out how alcohol affects your gut.
With our first sip of alcohol, we’re introducing booze to our body through the tissues of our mouth. Alcohol is an irritant, and studies show that excessive intake can increase the chances of mouth and throat cancers.
When it comes to alcohol and digestion, one of the first victims is the esophagus. Alcohol relaxes the lower esophageal sphincter (LES), the small ring of muscle separating our esophagus and stomach that keeps stomach acid right in the stomach where it belongs. However, when we drink alcohol, the LES gets a bit lax, and it allows some acid to leak back into the esophagus — a process known as acid reflux.
Picture it like this: the LES is like a bouncer at a club, diligently keeping troublemakers — stomach acid — from entering the esophagus. But when alcohol comes on the scene, the bouncer gets distracted, letting the party crashers slip through and cause a ruckus. Hello, heartburn!
Alcohol's next target is the stomach lining, the resilient protective layer that keeps stomach acid from harming our stomach tissues. Does wine help with digestion? In fact, it’s more likely to do the opposite. Science says we can get stomach problems from drinking. In fact, alcohol’s effects on the stomach can be quite serious. Does alcohol cause stomach pain? It can indeed. Alcohol can cause inflammation and erosion of the stomach lining, and researchers have found links between alcohol and gastritis, alcohol and ulcers, and alcohol and gi issues that can cause pain and discomfort. While the stomach lining is very durable, the relentless onslaught of booze can gradually wear it down, leaving the stomach tissue increasingly vulnerable.
The liver is the main player when it comes to getting alcohol — a toxin, as far as our body is concerned — out of our system. It does this by converting ethanol to acetaldehyde (a compound that’s actually more toxic than alcohol) before turning it into harmless acetic acid that can be excreted in urine. Needless to say, this process takes a toll. Over time, excessive alcohol use can damage the liver, leading to inflammation, fatty liver, and, eventually, cirrhosis.
The pancreas — a busy factory producing digestive enzymes and insulin — helps control the body’s blood sugar levels. Under normal conditions, digestive enzymes produced by the pancreas are inactive until they reach the small intestine, where they begin breaking down food.
However, when we drink alcohol, our pancreas gets inflamed, a condition called pancreatitis. In its eagerness to break down alcohol, the pancreas starts to "overheat" and actually begins digesting itself — a process that’s every bit as uncomfortable as it sounds!
Pancreatitis can cause intense abdominal pain and lead to serious complications, including type 1 diabetes if the insulin-producing cells in the pancreas are damaged. It can also result in malnutrition due to our food not being properly broken down and absorbed. In extreme cases, the condition can be life-threatening.
Most nutrient absorption happens in the small intestine, a 20-foot-long tube coiled in our abdomen. Alcohol can interfere with this process, leading to nutrient deficiencies.
How does alcohol slow digestion? Imagine our small intestine as a busy highway, with alcohol a traffic jam blocking the roads and preventing essential nutrients from reaching their destinations. This digestive log jam can wreak havoc on different body systems.
The final stage of our digestive journey — the large intestine — is not spared alcohol's effects. Regular drinking disrupts the balance of bacteria in the large intestine, leading to issues such as diarrhea and constipation. Picture our large intestine as a well-managed city with a balance of good bacteria (the citizens) and bad bacteria (the troublemakers). When alcohol comes to town, it upsets this balance, causing all kinds of chaos. There is a well-established link between alcohol and IBS, as well as between alcohol and digestive cancer.

Yes, alcohol can be quite problematic for our digestive system — but our bodies are remarkably resilient. If you frequently experience lower abdominal pain after drinking alcohol or have discomfort anywhere in the digestive tract after drinking, it’s worth taking a closer look at your drinking habits before things get worse. The great news is that as soon as we start cutting back on alcohol, our bodies begin to heal. Now, let's explore some specific actions we can take to support this process:
By understanding how alcohol affects our bodies and making an effort to reduce our intake, we're well on our way to a healthier digestive system!
In the words of Nancy Mure, “In understanding the basics of digestion, you'll discover who's in charge. Here's a hint. It's not you.”
When all is well, we don’t give digestion much thought. However, as soon as problems arise, it’s hard to think about anything else. For many, stomach pain after drinking alcohol is a recurring problem, while others experience lower abdominal pain after drinking alcohol. So, how does alcohol affect the digestive system? What does alcohol do to your stomach? Does wine help with digestion? Are there any digestive problems caused by alcohol or stomach issues from alcohol misuse? And what is the connection between alcohol and gut health? If you’ve ever wondered what causes stomach inflammation or wanted to explore the link between alcohol and gastritis, alcohol and IBS, alcohol and ulcers, or alcohol and digestive cancer, it’s time to dig deeper. Let’s look at the connection more closely by examining five ways in which alcohol affects the stomach and digestive system.

Let’s take a brief tour through the digestive system to see what happens when alcohol enters the scene to understand the link between alcohol and digestive issues and find out how alcohol affects your gut.
With our first sip of alcohol, we’re introducing booze to our body through the tissues of our mouth. Alcohol is an irritant, and studies show that excessive intake can increase the chances of mouth and throat cancers.
When it comes to alcohol and digestion, one of the first victims is the esophagus. Alcohol relaxes the lower esophageal sphincter (LES), the small ring of muscle separating our esophagus and stomach that keeps stomach acid right in the stomach where it belongs. However, when we drink alcohol, the LES gets a bit lax, and it allows some acid to leak back into the esophagus — a process known as acid reflux.
Picture it like this: the LES is like a bouncer at a club, diligently keeping troublemakers — stomach acid — from entering the esophagus. But when alcohol comes on the scene, the bouncer gets distracted, letting the party crashers slip through and cause a ruckus. Hello, heartburn!
Alcohol's next target is the stomach lining, the resilient protective layer that keeps stomach acid from harming our stomach tissues. Does wine help with digestion? In fact, it’s more likely to do the opposite. Science says we can get stomach problems from drinking. In fact, alcohol’s effects on the stomach can be quite serious. Does alcohol cause stomach pain? It can indeed. Alcohol can cause inflammation and erosion of the stomach lining, and researchers have found links between alcohol and gastritis, alcohol and ulcers, and alcohol and gi issues that can cause pain and discomfort. While the stomach lining is very durable, the relentless onslaught of booze can gradually wear it down, leaving the stomach tissue increasingly vulnerable.
The liver is the main player when it comes to getting alcohol — a toxin, as far as our body is concerned — out of our system. It does this by converting ethanol to acetaldehyde (a compound that’s actually more toxic than alcohol) before turning it into harmless acetic acid that can be excreted in urine. Needless to say, this process takes a toll. Over time, excessive alcohol use can damage the liver, leading to inflammation, fatty liver, and, eventually, cirrhosis.
The pancreas — a busy factory producing digestive enzymes and insulin — helps control the body’s blood sugar levels. Under normal conditions, digestive enzymes produced by the pancreas are inactive until they reach the small intestine, where they begin breaking down food.
However, when we drink alcohol, our pancreas gets inflamed, a condition called pancreatitis. In its eagerness to break down alcohol, the pancreas starts to "overheat" and actually begins digesting itself — a process that’s every bit as uncomfortable as it sounds!
Pancreatitis can cause intense abdominal pain and lead to serious complications, including type 1 diabetes if the insulin-producing cells in the pancreas are damaged. It can also result in malnutrition due to our food not being properly broken down and absorbed. In extreme cases, the condition can be life-threatening.
Most nutrient absorption happens in the small intestine, a 20-foot-long tube coiled in our abdomen. Alcohol can interfere with this process, leading to nutrient deficiencies.
How does alcohol slow digestion? Imagine our small intestine as a busy highway, with alcohol a traffic jam blocking the roads and preventing essential nutrients from reaching their destinations. This digestive log jam can wreak havoc on different body systems.
The final stage of our digestive journey — the large intestine — is not spared alcohol's effects. Regular drinking disrupts the balance of bacteria in the large intestine, leading to issues such as diarrhea and constipation. Picture our large intestine as a well-managed city with a balance of good bacteria (the citizens) and bad bacteria (the troublemakers). When alcohol comes to town, it upsets this balance, causing all kinds of chaos. There is a well-established link between alcohol and IBS, as well as between alcohol and digestive cancer.

Yes, alcohol can be quite problematic for our digestive system — but our bodies are remarkably resilient. If you frequently experience lower abdominal pain after drinking alcohol or have discomfort anywhere in the digestive tract after drinking, it’s worth taking a closer look at your drinking habits before things get worse. The great news is that as soon as we start cutting back on alcohol, our bodies begin to heal. Now, let's explore some specific actions we can take to support this process:
By understanding how alcohol affects our bodies and making an effort to reduce our intake, we're well on our way to a healthier digestive system!

Alcohol metabolism demands extra work from our liver, impacting the immune system and making us more susceptible to illness. Additionally, it sabotages the immune response by interfering with gut microbiota and disrupting white blood cells.
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually, with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet millions of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
It's a Tuesday evening, not a Friday, but hey, who's counting? You've wrapped up another day of work, and as you flop into your favorite armchair, you fancy a glass of your go-to red. You pour the rich, robust vino, and with the first sip, it's like a mini vacation. Ah, bliss!
But then the next day … what a bummer. You wake up with a sore throat, cough, and maybe even a fever. What gives? Does alcohol weaken your immune system — or, more precisely, does alcohol lower your immune system’s ability to fight off infections? Unfortunately, yes — alcohol, especially when it’s consumed regularly over a long time, can do a number on the immune system. In fact, a single session of 5 to 6 drinks has been shown to shut down the immune system for as long as 24 hours, leaving us open to catching anything from the common cold to a more serious disease!

Before we get into alcohol and immune system interactions, let's get the lowdown on our immune system itself. It has an army of cells and proteins ever-ready to battle villains such as bacteria and viruses. Here’s how it works:
How does alcohol affect immune system functioning? — when alcohol enters the scene, it can potentially derail our superhero squad, wreaking havoc in the immune system and undermining its effectiveness.
Alcohol — just like everything else we ingest — gets metabolized in our body. It's primarily processed in the liver, which works tirelessly to detoxify and cleanse our system.
Why does this matter for our immune system? Because our body sees alcohol as a toxin, something dangerous to remove as quickly as possible, the liver prioritizes processing it above everything else. While our liver is dealing with alcohol, it has less energy and resources to support our immunity, leaving us more susceptible.
But that’s not the whole story — let’s dig a bit deeper and find out more!
First, let's talk about our innate immunity — the frontline of our immune system. When we throw back a shot or sip a cocktail, it can mess with our immune cells’ ability to effectively deal with invading pathogens. So, that cold or flu we're trying to fight off might stick around longer than it would have if we'd skipped that drink.
Here’s what happens in more detail:
While enjoying a single drink might not sound the alarms throughout the entire immune system, even moderate drinking can extend the time it takes your body to recover from illnesses. How does drinking lower your immune system’s ability to defend you against diseases? That cold that should've been gone in three days? It lingers for a week or more. The flu that should've lasted a week? It stays for almost twice as long. This is our immune system, compromised and lagging, all because alcohol distracted our guards.
Then comes round two: alcohol versus our adaptive immunity. This part of our immune system learns and adapts to specific threats. The adaptive immunity system is our body's elite force, specialized and refined through experience. Unlike the innate immunity, which reacts instantly to all invaders, the adaptive immune system has a memory. It recalls past encounters with specific pathogens, enabling it to swiftly and effectively target these familiar foes. But when alcohol enters our body, this elite force faces significant challenges:
Considering all these disruptions, it's no surprise that alcohol slows the adaptive immune response. Instead of swiftly recognizing and counteracting a known threat, our system stumbles, taking longer to rally its defenses.
While a single drink might not dismantle our defenses, consistent and excessive consumption can dull the sharp edge of our adaptive immunity, leaving us more susceptible to infections and reducing the efficiency of vaccinations.
As we've seen, alcohol can hinder the work of our innate and adaptive immunity. But there’s more! Booze doesn't stop at just hampering our immune response — it can even misdirect it.
Here's another twist: our gut, which plays a key role in maintaining our immune system, also bears the brunt of our alcohol consumption. The gut microbiota — a whole universe of bacteria that call our intestines home — plays a crucial role in keeping us healthy.
As it turns out, alcohol interacts directly with these little residents in a way that can lead to a cascade of health issues. By disrupting the balance of good and bad bacteria, alcohol leads to something called "leaky gut." And — as you might guess — stuff leaking from your gut is bad news: it leads to harmful substances sneaking into the bloodstream, like toxins from the sewer leaking into our water supply. What's more, it can trigger our immune system to respond, which can lead to chronic inflammation, a condition associated with a host of health problems, from arthritis to heart disease.

And what if alcohol becomes a regular guest, week after week, year after year? Well, things get even worse: long-term heavy drinking can leave our immune system in a perpetual state of confusion and disarray, making us more susceptible to infections and even cancer. Yikes!
On the flip side, our bodies are amazing and are capable of making remarkable recoveries. How long does it take for the immune system to recover from alcohol misuse? It depends on our overall health, but recovery starts as soon as we quit or cut back.
Now that we know how problematic alcohol can be for our immune system, let's talk about how we can show it the door — or at least keep it in check.
As for supporting your immune system, here are some more specific tips:
Just like all of our other bodily systems, our immune system needs a bit of care and consideration to function at its best. You need to find the balance that lets you enjoy your life without compromising your body's defenses.
As author and neuroscientist Abhijit Naskar explains, “Symptoms of a sickness are not necessarily signs of weakness, rather they imply that your body is actively fighting the sickness. And when all the resources of the body fall short to fight the sickness, that's when the real trouble begins.” Let’s give our bodies the opportunity to use the amazing resources that have evolved to keep us in top shape.
It's a Tuesday evening, not a Friday, but hey, who's counting? You've wrapped up another day of work, and as you flop into your favorite armchair, you fancy a glass of your go-to red. You pour the rich, robust vino, and with the first sip, it's like a mini vacation. Ah, bliss!
But then the next day … what a bummer. You wake up with a sore throat, cough, and maybe even a fever. What gives? Does alcohol weaken your immune system — or, more precisely, does alcohol lower your immune system’s ability to fight off infections? Unfortunately, yes — alcohol, especially when it’s consumed regularly over a long time, can do a number on the immune system. In fact, a single session of 5 to 6 drinks has been shown to shut down the immune system for as long as 24 hours, leaving us open to catching anything from the common cold to a more serious disease!

Before we get into alcohol and immune system interactions, let's get the lowdown on our immune system itself. It has an army of cells and proteins ever-ready to battle villains such as bacteria and viruses. Here’s how it works:
How does alcohol affect immune system functioning? — when alcohol enters the scene, it can potentially derail our superhero squad, wreaking havoc in the immune system and undermining its effectiveness.
Alcohol — just like everything else we ingest — gets metabolized in our body. It's primarily processed in the liver, which works tirelessly to detoxify and cleanse our system.
Why does this matter for our immune system? Because our body sees alcohol as a toxin, something dangerous to remove as quickly as possible, the liver prioritizes processing it above everything else. While our liver is dealing with alcohol, it has less energy and resources to support our immunity, leaving us more susceptible.
But that’s not the whole story — let’s dig a bit deeper and find out more!
First, let's talk about our innate immunity — the frontline of our immune system. When we throw back a shot or sip a cocktail, it can mess with our immune cells’ ability to effectively deal with invading pathogens. So, that cold or flu we're trying to fight off might stick around longer than it would have if we'd skipped that drink.
Here’s what happens in more detail:
While enjoying a single drink might not sound the alarms throughout the entire immune system, even moderate drinking can extend the time it takes your body to recover from illnesses. How does drinking lower your immune system’s ability to defend you against diseases? That cold that should've been gone in three days? It lingers for a week or more. The flu that should've lasted a week? It stays for almost twice as long. This is our immune system, compromised and lagging, all because alcohol distracted our guards.
Then comes round two: alcohol versus our adaptive immunity. This part of our immune system learns and adapts to specific threats. The adaptive immunity system is our body's elite force, specialized and refined through experience. Unlike the innate immunity, which reacts instantly to all invaders, the adaptive immune system has a memory. It recalls past encounters with specific pathogens, enabling it to swiftly and effectively target these familiar foes. But when alcohol enters our body, this elite force faces significant challenges:
Considering all these disruptions, it's no surprise that alcohol slows the adaptive immune response. Instead of swiftly recognizing and counteracting a known threat, our system stumbles, taking longer to rally its defenses.
While a single drink might not dismantle our defenses, consistent and excessive consumption can dull the sharp edge of our adaptive immunity, leaving us more susceptible to infections and reducing the efficiency of vaccinations.
As we've seen, alcohol can hinder the work of our innate and adaptive immunity. But there’s more! Booze doesn't stop at just hampering our immune response — it can even misdirect it.
Here's another twist: our gut, which plays a key role in maintaining our immune system, also bears the brunt of our alcohol consumption. The gut microbiota — a whole universe of bacteria that call our intestines home — plays a crucial role in keeping us healthy.
As it turns out, alcohol interacts directly with these little residents in a way that can lead to a cascade of health issues. By disrupting the balance of good and bad bacteria, alcohol leads to something called "leaky gut." And — as you might guess — stuff leaking from your gut is bad news: it leads to harmful substances sneaking into the bloodstream, like toxins from the sewer leaking into our water supply. What's more, it can trigger our immune system to respond, which can lead to chronic inflammation, a condition associated with a host of health problems, from arthritis to heart disease.

And what if alcohol becomes a regular guest, week after week, year after year? Well, things get even worse: long-term heavy drinking can leave our immune system in a perpetual state of confusion and disarray, making us more susceptible to infections and even cancer. Yikes!
On the flip side, our bodies are amazing and are capable of making remarkable recoveries. How long does it take for the immune system to recover from alcohol misuse? It depends on our overall health, but recovery starts as soon as we quit or cut back.
Now that we know how problematic alcohol can be for our immune system, let's talk about how we can show it the door — or at least keep it in check.
As for supporting your immune system, here are some more specific tips:
Just like all of our other bodily systems, our immune system needs a bit of care and consideration to function at its best. You need to find the balance that lets you enjoy your life without compromising your body's defenses.
As author and neuroscientist Abhijit Naskar explains, “Symptoms of a sickness are not necessarily signs of weakness, rather they imply that your body is actively fighting the sickness. And when all the resources of the body fall short to fight the sickness, that's when the real trouble begins.” Let’s give our bodies the opportunity to use the amazing resources that have evolved to keep us in top shape.

Scientists have found that alcohol can trigger migraines through several mechanisms, including dehydration, vasodilation, effects of additives, and disruption of sleep patterns.
Ready to say goodbye to alcohol-induced migraines for good? The Reframe app can help! While we’re not a cure for alcohol use disorder (AUD), we can help you cut back on drinking gradually by using science-backed methods to empower you throughout your journey. Our program has helped millions of people just like you to drink less and live more!
The Reframe app gives you the tools and knowledge to cut back or quit drinking less in an intuitive, effective way. You’ll receive daily science-backed readings and will have access to our in-app Toolkit, filled with the resources and activities you need to navigate anything life throws at you.
You’ll meet millions of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
Alcohol can be a real conundrum for those of us who get migraines. Perhaps you've experienced that splitting headache after a night of indulgence. Let's delve into the world of migraine research and explore how alcohol might be a contributing factor.
When we think about migraines, we often picture intense, throbbing headaches. But migraines are often accompanied by a whole carnival of symptoms — including nausea, sensitivity to light and sound, and sometimes visual disturbances known as “auras.”
What happens when alcohol enters the equation? We're all familiar with the infamous “hangover headache,” but can alcohol cause migraines? And what’s the connection between cocktails and headaches?
In a word: yes. Research studies have shown that alcohol can, indeed, act as a migraine trigger for some people. But why does this happen? The answer lies in the way alcohol interacts with our bodies.
A growing body of scientific research suggests a possible connection between alcohol consumption and migraines. A 2018 study found that alcohol was reported to be a trigger in 35.6% of migraine patients. However, the relationship between alcohol and migraines is complex, involving several scientific theories.
First off, alcohol is a diuretic: it encourages our kidneys to produce more urine, leading to dehydration. Since dehydration is a well-known trigger for migraines, it's no surprise that our beloved drinks can push us towards a throbbing headache.
Moreover, alcohol can cause blood vessels in our brain to expand, a process called vasodilation. This change in the body's internal roadways can trigger migraines in some people.
But the story doesn't end there. Alcohol — especially dark drinks such as red wine and whiskey — contain chemicals known as congeners, which can set off migraines for some of us.
Finally, alcohol affects our sleep patterns. Even though a couple of drinks might make us feel sleepy, they actually disrupt our sleep cycle, causing poor sleep quality over the course of the night. Our brains don't appreciate this, and they often retaliate with a migraine.

It's important to distinguish between a “cause” and a “trigger.” The cause of migraines is multifaceted, often involving genetic factors and imbalances in brain chemicals. Alcohol is not a “cause” of migraines per se, but it can be a “trigger” for migraine attacks in those of us prone to them for other reasons.
Red wine is widely believed to be a major offender. However, research has demonstrated that all types of alcoholic beverages can trigger migraines. A study in the European Journal of Neurology found that while red wine was the most frequently reported trigger, other alcoholic drinks were not far behind.
It's essential to note that everyone's experience with alcohol and migraines is unique. Some of us may have a migraine episode after just a single glass of champagne, while others may not experience any adverse effects even after consuming multiple drinks. This variability is attributed to our individual genetic makeup, lifestyle factors, and the type of alcohol consumed.
For those of us who are frequent drinkers and are considering quitting, it's important to understand that alcohol withdrawal may trigger migraines, too. This is because our brain has adapted to the regular presence of alcohol and reacts to its absence. This is only a factor until our brain becomes accustomed to life without alcohol, so don’t let this deter you from quitting, if that’s your goal.
So, what can we do about the migraine-alcohol connection? Here are some specific action steps for those of us considering cutting back on or quitting alcohol.
Everyone’s journey towards a migraine-free future is unique. While it may seem like a tall order, armed with knowledge and determination, we can take a step towards it by managing our alcohol intake. Remember, alcohol is not the only potential trigger for migraines. A holistic lifestyle change, which includes balanced nutrition, regular exercise, and stress management, along with reducing alcohol consumption, can have a profound impact on our overall well-being.
Alcohol can be a real conundrum for those of us who get migraines. Perhaps you've experienced that splitting headache after a night of indulgence. Let's delve into the world of migraine research and explore how alcohol might be a contributing factor.
When we think about migraines, we often picture intense, throbbing headaches. But migraines are often accompanied by a whole carnival of symptoms — including nausea, sensitivity to light and sound, and sometimes visual disturbances known as “auras.”
What happens when alcohol enters the equation? We're all familiar with the infamous “hangover headache,” but can alcohol cause migraines? And what’s the connection between cocktails and headaches?
In a word: yes. Research studies have shown that alcohol can, indeed, act as a migraine trigger for some people. But why does this happen? The answer lies in the way alcohol interacts with our bodies.
A growing body of scientific research suggests a possible connection between alcohol consumption and migraines. A 2018 study found that alcohol was reported to be a trigger in 35.6% of migraine patients. However, the relationship between alcohol and migraines is complex, involving several scientific theories.
First off, alcohol is a diuretic: it encourages our kidneys to produce more urine, leading to dehydration. Since dehydration is a well-known trigger for migraines, it's no surprise that our beloved drinks can push us towards a throbbing headache.
Moreover, alcohol can cause blood vessels in our brain to expand, a process called vasodilation. This change in the body's internal roadways can trigger migraines in some people.
But the story doesn't end there. Alcohol — especially dark drinks such as red wine and whiskey — contain chemicals known as congeners, which can set off migraines for some of us.
Finally, alcohol affects our sleep patterns. Even though a couple of drinks might make us feel sleepy, they actually disrupt our sleep cycle, causing poor sleep quality over the course of the night. Our brains don't appreciate this, and they often retaliate with a migraine.

It's important to distinguish between a “cause” and a “trigger.” The cause of migraines is multifaceted, often involving genetic factors and imbalances in brain chemicals. Alcohol is not a “cause” of migraines per se, but it can be a “trigger” for migraine attacks in those of us prone to them for other reasons.
Red wine is widely believed to be a major offender. However, research has demonstrated that all types of alcoholic beverages can trigger migraines. A study in the European Journal of Neurology found that while red wine was the most frequently reported trigger, other alcoholic drinks were not far behind.
It's essential to note that everyone's experience with alcohol and migraines is unique. Some of us may have a migraine episode after just a single glass of champagne, while others may not experience any adverse effects even after consuming multiple drinks. This variability is attributed to our individual genetic makeup, lifestyle factors, and the type of alcohol consumed.
For those of us who are frequent drinkers and are considering quitting, it's important to understand that alcohol withdrawal may trigger migraines, too. This is because our brain has adapted to the regular presence of alcohol and reacts to its absence. This is only a factor until our brain becomes accustomed to life without alcohol, so don’t let this deter you from quitting, if that’s your goal.
So, what can we do about the migraine-alcohol connection? Here are some specific action steps for those of us considering cutting back on or quitting alcohol.
Everyone’s journey towards a migraine-free future is unique. While it may seem like a tall order, armed with knowledge and determination, we can take a step towards it by managing our alcohol intake. Remember, alcohol is not the only potential trigger for migraines. A holistic lifestyle change, which includes balanced nutrition, regular exercise, and stress management, along with reducing alcohol consumption, can have a profound impact on our overall well-being.

Learn how alcohol and cancer are connected, the science behind the risk, and practical steps you can take to protect your long-term health.
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually, with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet millions of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app through the App Store or Google Play today!
A glass of wine after a long day can feel like a simple pleasure, right? We often hear about alcohol's effect on the liver, but there's a quieter, more serious conversation we need to have about alcohol and cancer. The truth is, the risk is real, even for moderate drinkers. The process of alcohol causing cancer starts the moment you take a sip, as your body breaks it down into a harmful chemical. Let's look at the facts behind the alcohol and cancer risk so you can make informed choices for your health.
When we talk about the health effects of alcohol, we often think of liver damage or addiction. But the conversation is shifting to include a significant, and often overlooked, connection to cancer. It’s a heavy topic, I know, but understanding the science is the first step toward making informed choices for our health. The evidence isn't just correlational; major health organizations have identified alcohol as a carcinogen, meaning it has the potential to cause cancer. This happens through a few different mechanisms, like how our bodies break down alcohol into a toxic chemical called acetaldehyde, which can damage our DNA and stop our cells from repairing themselves. It’s not about fear, but about awareness and empowerment.
So, which cancers are we talking about? The list is more extensive than many people realize. According to health authorities like the CDC, drinking alcohol raises your risk for several types of cancer. This includes cancers of the mouth, throat, and voice box (larynx). It doesn't stop there; the risk extends to the esophagus, colon and rectum, and liver. For women, alcohol consumption is also a known risk factor for breast cancer. The connection is clear and well-documented, showing that alcohol can affect various parts of the body, particularly along the digestive tract where it comes into direct contact with tissues. Knowing exactly where the risks lie helps to create a fuller picture of alcohol's impact on our long-term health.
The numbers behind this connection are pretty sobering. Research shows that alcohol is a significant contributor to both cancer cases and cancer deaths globally. In the United States alone, about 20,000 adults die each year from cancers linked to alcohol. To put it another way, roughly 5.5% of all new cancer cases are associated with drinking. The risk also increases with the amount you drink. For example, drinking about 3.5 drinks per day can double or even triple your risk for cancers of the mouth and throat. These statistics aren't meant to scare you, but to highlight the real-world impact. This knowledge can be a powerful motivator for anyone looking to re-evaluate their habits and explore a more mindful approach to drinking.
Is alcohol a carcinogen? Yes, but the real risk is its metabolite, acetaldehyde. When we consume alcohol, our bodies set out to break it down, primarily in the liver. In this process, a compound called acetaldehyde is formed. Acetaldehyde is a bit of a rascal. It's a carcinogen, which means it can cause cancer by damaging DNA and stopping our cells from repairing this damage. Over time, this can lead to abnormal cell growth, potentially developing into cancer.
Let’s look into the mechanics of acetaldehyde in a bit more detail. The International Agency for Research on Cancer has classified this volatile compound in the highest risk category: it’s a Group 1 carcinogen alongside substances like tobacco smoke and asbestos.
But how exactly does acetaldehyde contribute to cancer development? There are several ways it exerts its harmful effects:
Our bodies do have defense mechanisms against acetaldehyde, such as the enzyme aldehyde dehydrogenase (ALDH), which breaks down acetaldehyde into a non-toxic substance. However, certain individuals have a variant of the ALDH enzyme that works less efficiently, leading to a flushed complexion and an accumulation of acetaldehyde after drinking. This population may have a higher risk of alcohol-related cancers.
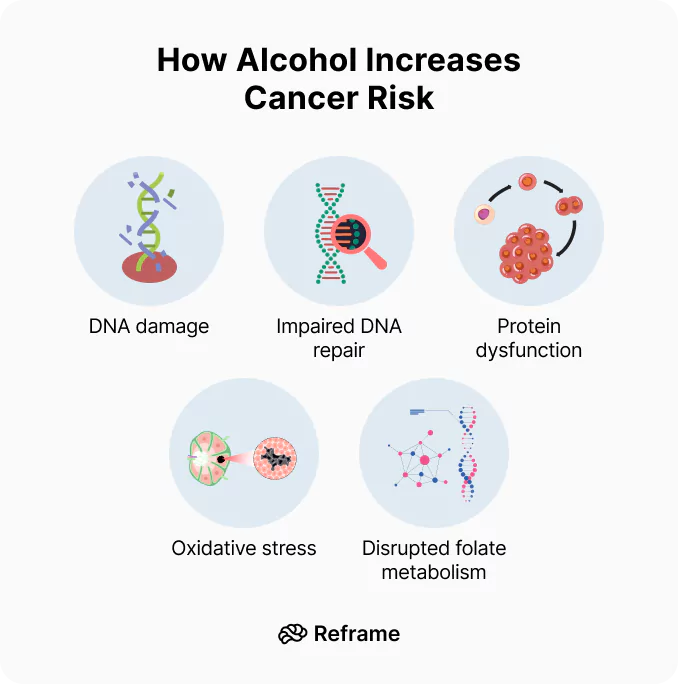
As we’ve touched on, acetaldehyde is the primary villain in this story. This toxic chemical directly attacks our DNA, the very instruction manual for our cells. It creates what scientists call “DNA adducts,” which are essentially harmful attachments that distort our DNA’s structure. Think of it like a typo in a critical line of code. When our cells try to replicate with this damaged code, it can lead to mutations. These mutations can cause cells to grow uncontrollably, which is the hallmark of cancer. This direct damage is one of the most significant ways alcohol consumption increases cancer risk, fundamentally altering our cellular blueprints over time.
It’s easy to forget that alcoholic drinks can be packed with calories, often with little to no nutritional value. These "empty calories" can contribute to weight gain, and carrying excess body weight is a well-established risk factor for several types of cancer, including breast, colon, and pancreatic cancer. Alcohol can also lower our inhibitions and stimulate appetite, leading to poor food choices. The connection is straightforward: regular drinking can make it harder to maintain a healthy weight, and that extra weight creates an environment in the body that’s more favorable for cancer to develop. You can get a clearer picture of your own consumption by using a tool to calculate the calories in the drinks you have.
Our liver is a powerhouse organ, responsible for filtering toxins from our blood, and alcohol is one of the biggest toxins it has to process. Heavy or consistent drinking puts immense strain on the liver, leading to inflammation and cell damage. Over time, this can result in a condition called cirrhosis, where healthy liver tissue is replaced by scar tissue. This scarring severely impairs liver function and dramatically increases the risk of developing liver cancer. Essentially, by overwhelming the liver, alcohol creates the very conditions—damage and scarring—that can pave the way for malignant cells to grow.
Drinking alcohol doesn't just add harmful substances to your body; it also hinders your body's ability to absorb the good stuff. Alcohol can irritate the lining of the stomach and intestines, which interferes with the absorption of essential vitamins and nutrients from the food you eat. One of the most critical nutrients affected is folate, a B vitamin that is vital for creating and repairing DNA. When your body is low on folate, it’s less equipped to fix the DNA damage caused by factors like acetaldehyde. This nutritional deficiency weakens your body's natural cancer defenses, making cells more vulnerable to mutations.
Inflammation is your body's natural response to injury or infection—a short-term defense mechanism. However, when your body is constantly exposed to irritants like alcohol, this response can become chronic. This state of ongoing, low-grade inflammation can be incredibly damaging. It produces free radicals that can harm your DNA, and it signals cells to divide more rapidly to repair the damage. This constant cycle of damage and rapid regeneration increases the chances of errors occurring during cell division, which can ultimately lead to the formation of cancerous tumors. Chronic inflammation essentially creates a fertile ground for cancer to take root and grow.
Alcohol also impacts hormone levels, especially sex hormones such as estrogen and testosterone. These hormonal imbalances are another route by which alcohol can increase cancer risk — particularly breast cancer. Breast cancer and alcohol have a well-established relationship. Let’s discuss the connection!
In women, estrogen promotes the development and maintenance of female characteristics, but it also regulates the growth and division of breast cells. Consuming alcohol can increase levels of estrogen in the body. A higher estrogen level means more cell divisions in breast tissue, increasing the likelihood of mutations and the development of cancer cells. Some of these cell divisions can lead to mutations, and over time, these mutations can accumulate and result in cancer.
Alcohol can also impact other hormones. For instance, it can raise levels of the hormone insulin-like growth factor 1 (IGF-1), which encourages cells to divide. Higher levels of IGF-1 have been associated with an increased risk of certain cancers, including breast and prostate cancer.
Additionally, alcohol can affect the liver's ability to regulate hormone levels due to the liver's role in detoxifying alcohol and metabolizing hormones. This can lead to hormonal imbalances and further increase the risk of cancer.
The hormonal effects of alcohol contribute to the risk of several cancers. Apart from breast cancer, alcohol-related hormonal imbalances can increase the risk of ovarian and endometrial cancers in women, and possibly prostate cancer in men.
So, why does alcohol pose a greater cancer risk for women? It largely comes down to our unique physiology and how our bodies process alcohol. Women generally have less body water than men of the same weight, which means alcohol becomes more concentrated in our system. On top of that, our stomachs produce less of the enzyme that breaks down alcohol before it even reaches the bloodstream. This combination means we absorb more alcohol and it takes longer to metabolize, leading to more prolonged exposure to the carcinogen acetaldehyde. This increased exposure, combined with alcohol’s tendency to disrupt our hormonal health, creates a perfect storm that elevates the risk for cancers of the breast, ovaries, and endometrium.
In addition to triggering these internal mechanisms, alcohol can increase cancer risk indirectly by making it easier for other harmful processes to take place.
Alcohol can act as a solvent, making it easier for carcinogenic chemicals — such as tobacco smoke — to enter our cells. It can also weaken our immune system, making it harder for us to fight off diseases, including cancer.
We’ve all heard it, right? That a glass of red wine with dinner is actually good for you, especially your heart. But this popular belief often glosses over a much more serious reality: the significant cancer risks tied to drinking any kind of alcohol. The truth is, when it comes to cancer, your body doesn't distinguish between a fancy Merlot and a cheap beer. The common denominator in all alcoholic drinks is ethanol, and that's where the trouble begins. All types of alcohol, whether it's wine, beer, or liquor, carry the same cancer risk because they all contain this compound.
So, what about drinking in moderation? Unfortunately, experts are clear that there is no safe amount of alcohol when it comes to cancer. Even a small amount increases your risk. While some studies have pointed to potential heart benefits from the antioxidants in red wine, these benefits simply don't outweigh the proven cancer risks. The more alcohol you consume, the higher your risk becomes. It's a straightforward relationship that puts the "healthy glass of wine" idea into a much different perspective, encouraging us to look at the complete picture of how alcohol affects our long-term health.
So how can we use this information to live healthier lives? For one, cutting back on alcohol or abstaining altogether can significantly reduce our risk.
Here are some additional changes that can make a big difference:
Together, we can navigate the journey to a healthier, happier life. Remember, every little step counts!
When it comes to alcohol and health, it helps to have a clear benchmark. Official guidelines from health organizations like the Centers for Disease Control and Prevention (CDC) provide a framework based on scientific evidence. These recommendations aren't about judgment; they're about giving you the information you need to make choices that align with your health goals. Understanding what experts consider moderate consumption is a crucial first step in evaluating your own habits. It allows you to see where you stand and decide what, if any, changes you’d like to make. Think of it as a map — it shows you the terrain so you can choose your path forward.
One of the biggest hurdles in tracking alcohol intake is knowing what a “standard drink” actually is. It’s easy to underestimate how much you’re consuming when drink sizes vary so much. According to the MD Anderson Cancer Center, one standard drink is defined as 12 ounces of beer, 5 ounces of wine, or 1.5 ounces of 80-proof liquor. That generous glass of wine you pour at home could easily count as two standard drinks. Being aware of these measurements is key to accurately assessing your consumption and understanding your risk. It’s the foundation of mindful drinking and helps you stay honest with yourself about your habits.
So, what do the experts recommend? The CDC advises that if you choose to drink, you do so in moderation. For women, this means one standard drink or less per day, and for men, it’s two standard drinks or less per day. It’s important to remember that these are upper limits for the days you do drink, not daily targets to aim for. The healthiest option is always to drink less. These guidelines are designed to help minimize health risks, including the risk of cancer. Sticking to them is a powerful way to protect your long-term well-being while still allowing yourself to enjoy a drink on occasion if you choose to.
The link between how much you drink and your cancer risk is direct and significant. It’s not just heavy drinking that poses a threat; even moderate amounts can increase your chances of developing certain cancers. According to the Canadian Cancer Society, consuming about 3.5 drinks a day can double or even triple your risk of cancers in the mouth, throat, and esophagus. The same amount increases the risk of colon and breast cancer by 1.5 times. This dose-response relationship is clear: the more you drink, the higher your risk. This knowledge is empowering because it puts the control back in your hands. Every drink you skip is a step toward lowering that risk.
If you're feeling concerned, here’s some good news: it’s never too late to make a positive change. When you stop drinking, your risk for alcohol-related cancers begins to decrease over time. While it may take many years for the risk to be fully removed, quitting is a significant and proactive step for your health. Your body has an incredible capacity for healing, and reducing its exposure to carcinogens like acetaldehyde gives it a chance to repair. This journey of mindful drinking or quitting entirely is one of the most impactful things you can do for your future self, and every day alcohol-free is a victory for your long-term health.
For anyone currently facing a cancer diagnosis or in recovery, the conversation around alcohol becomes even more critical. It’s essential to talk to your doctor about your alcohol use. Drinking can interfere with treatment, worsen side effects, and potentially increase the risk of developing new cancers. Your healthcare team can provide personalized advice based on your specific diagnosis, treatment plan, and overall health. This conversation is a vital part of your care, ensuring that your lifestyle choices support your recovery and help protect your health moving forward. Don't hesitate to bring it up; your medical team is there to support you in every aspect of your journey.
I've always heard that a glass of red wine is good for you. Is that not true when it comes to cancer? That's a common belief, but when we're talking about cancer risk, the type of alcohol doesn't matter. Whether it's wine, beer, or liquor, they all contain ethanol, which your body converts into a cancer-causing chemical. While some studies point to antioxidants in red wine for heart health, those benefits don't cancel out the proven cancer risk that comes with any alcoholic drink.
Does even light or moderate drinking really increase my cancer risk? Yes, unfortunately, the evidence is clear that even small amounts of alcohol can increase your risk for certain cancers. There isn't a "safe" threshold when it comes to cancer prevention. The relationship is straightforward: the more you drink over time, the higher your risk becomes. This is why understanding what a standard drink is and being mindful of your intake is so important.
Why is the cancer risk from alcohol higher for women? It really comes down to our physiology. Women tend to have less body water than men, which means alcohol becomes more concentrated in our systems. We also produce less of a key enzyme in our stomachs that breaks down alcohol. This combination leads to higher blood alcohol concentrations and longer exposure to its harmful byproducts, which, along with alcohol's effect on hormones like estrogen, elevates our risk.
What is the main way alcohol actually causes cancer? The primary culprit is a toxic chemical called acetaldehyde. When you drink alcohol, your body works to break it down, and acetaldehyde is the main byproduct of that process. This chemical is a known carcinogen that can directly damage the DNA in your cells and prevent your body from repairing that damage. Over time, this can lead to mutations that cause cells to grow uncontrollably.
If I cut back or stop drinking now, can I actually lower my risk? Absolutely. It's one of the most empowering things to know. While it can take time, your body has an amazing ability to heal. When you reduce or eliminate alcohol, you lower your exposure to its cancer-causing effects, and your risk for developing alcohol-related cancers begins to decrease. Every step you take toward drinking less is a positive move for your long-term health.
A glass of wine after a long day can feel like a simple pleasure, right? We often hear about alcohol's effect on the liver, but there's a quieter, more serious conversation we need to have about alcohol and cancer. The truth is, the risk is real, even for moderate drinkers. The process of alcohol causing cancer starts the moment you take a sip, as your body breaks it down into a harmful chemical. Let's look at the facts behind the alcohol and cancer risk so you can make informed choices for your health.
When we talk about the health effects of alcohol, we often think of liver damage or addiction. But the conversation is shifting to include a significant, and often overlooked, connection to cancer. It’s a heavy topic, I know, but understanding the science is the first step toward making informed choices for our health. The evidence isn't just correlational; major health organizations have identified alcohol as a carcinogen, meaning it has the potential to cause cancer. This happens through a few different mechanisms, like how our bodies break down alcohol into a toxic chemical called acetaldehyde, which can damage our DNA and stop our cells from repairing themselves. It’s not about fear, but about awareness and empowerment.
So, which cancers are we talking about? The list is more extensive than many people realize. According to health authorities like the CDC, drinking alcohol raises your risk for several types of cancer. This includes cancers of the mouth, throat, and voice box (larynx). It doesn't stop there; the risk extends to the esophagus, colon and rectum, and liver. For women, alcohol consumption is also a known risk factor for breast cancer. The connection is clear and well-documented, showing that alcohol can affect various parts of the body, particularly along the digestive tract where it comes into direct contact with tissues. Knowing exactly where the risks lie helps to create a fuller picture of alcohol's impact on our long-term health.
The numbers behind this connection are pretty sobering. Research shows that alcohol is a significant contributor to both cancer cases and cancer deaths globally. In the United States alone, about 20,000 adults die each year from cancers linked to alcohol. To put it another way, roughly 5.5% of all new cancer cases are associated with drinking. The risk also increases with the amount you drink. For example, drinking about 3.5 drinks per day can double or even triple your risk for cancers of the mouth and throat. These statistics aren't meant to scare you, but to highlight the real-world impact. This knowledge can be a powerful motivator for anyone looking to re-evaluate their habits and explore a more mindful approach to drinking.
Is alcohol a carcinogen? Yes, but the real risk is its metabolite, acetaldehyde. When we consume alcohol, our bodies set out to break it down, primarily in the liver. In this process, a compound called acetaldehyde is formed. Acetaldehyde is a bit of a rascal. It's a carcinogen, which means it can cause cancer by damaging DNA and stopping our cells from repairing this damage. Over time, this can lead to abnormal cell growth, potentially developing into cancer.
Let’s look into the mechanics of acetaldehyde in a bit more detail. The International Agency for Research on Cancer has classified this volatile compound in the highest risk category: it’s a Group 1 carcinogen alongside substances like tobacco smoke and asbestos.
But how exactly does acetaldehyde contribute to cancer development? There are several ways it exerts its harmful effects:
Our bodies do have defense mechanisms against acetaldehyde, such as the enzyme aldehyde dehydrogenase (ALDH), which breaks down acetaldehyde into a non-toxic substance. However, certain individuals have a variant of the ALDH enzyme that works less efficiently, leading to a flushed complexion and an accumulation of acetaldehyde after drinking. This population may have a higher risk of alcohol-related cancers.
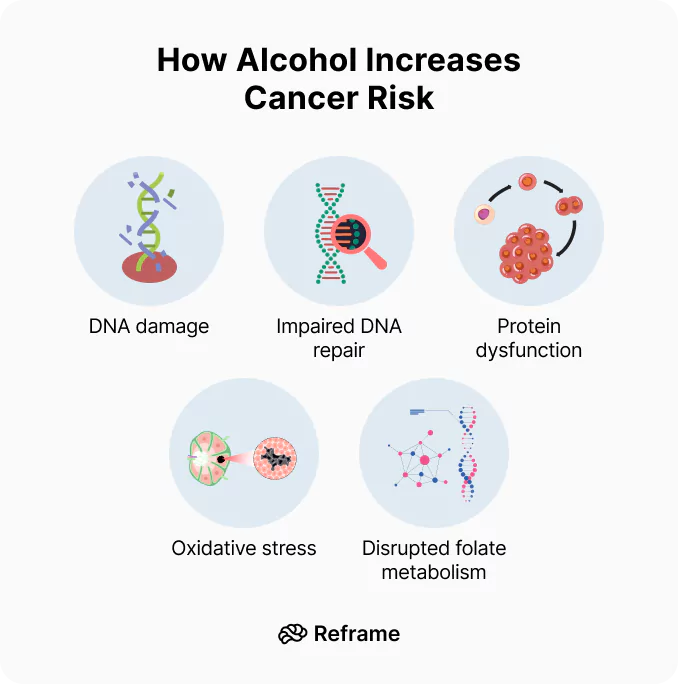
As we’ve touched on, acetaldehyde is the primary villain in this story. This toxic chemical directly attacks our DNA, the very instruction manual for our cells. It creates what scientists call “DNA adducts,” which are essentially harmful attachments that distort our DNA’s structure. Think of it like a typo in a critical line of code. When our cells try to replicate with this damaged code, it can lead to mutations. These mutations can cause cells to grow uncontrollably, which is the hallmark of cancer. This direct damage is one of the most significant ways alcohol consumption increases cancer risk, fundamentally altering our cellular blueprints over time.
It’s easy to forget that alcoholic drinks can be packed with calories, often with little to no nutritional value. These "empty calories" can contribute to weight gain, and carrying excess body weight is a well-established risk factor for several types of cancer, including breast, colon, and pancreatic cancer. Alcohol can also lower our inhibitions and stimulate appetite, leading to poor food choices. The connection is straightforward: regular drinking can make it harder to maintain a healthy weight, and that extra weight creates an environment in the body that’s more favorable for cancer to develop. You can get a clearer picture of your own consumption by using a tool to calculate the calories in the drinks you have.
Our liver is a powerhouse organ, responsible for filtering toxins from our blood, and alcohol is one of the biggest toxins it has to process. Heavy or consistent drinking puts immense strain on the liver, leading to inflammation and cell damage. Over time, this can result in a condition called cirrhosis, where healthy liver tissue is replaced by scar tissue. This scarring severely impairs liver function and dramatically increases the risk of developing liver cancer. Essentially, by overwhelming the liver, alcohol creates the very conditions—damage and scarring—that can pave the way for malignant cells to grow.
Drinking alcohol doesn't just add harmful substances to your body; it also hinders your body's ability to absorb the good stuff. Alcohol can irritate the lining of the stomach and intestines, which interferes with the absorption of essential vitamins and nutrients from the food you eat. One of the most critical nutrients affected is folate, a B vitamin that is vital for creating and repairing DNA. When your body is low on folate, it’s less equipped to fix the DNA damage caused by factors like acetaldehyde. This nutritional deficiency weakens your body's natural cancer defenses, making cells more vulnerable to mutations.
Inflammation is your body's natural response to injury or infection—a short-term defense mechanism. However, when your body is constantly exposed to irritants like alcohol, this response can become chronic. This state of ongoing, low-grade inflammation can be incredibly damaging. It produces free radicals that can harm your DNA, and it signals cells to divide more rapidly to repair the damage. This constant cycle of damage and rapid regeneration increases the chances of errors occurring during cell division, which can ultimately lead to the formation of cancerous tumors. Chronic inflammation essentially creates a fertile ground for cancer to take root and grow.
Alcohol also impacts hormone levels, especially sex hormones such as estrogen and testosterone. These hormonal imbalances are another route by which alcohol can increase cancer risk — particularly breast cancer. Breast cancer and alcohol have a well-established relationship. Let’s discuss the connection!
In women, estrogen promotes the development and maintenance of female characteristics, but it also regulates the growth and division of breast cells. Consuming alcohol can increase levels of estrogen in the body. A higher estrogen level means more cell divisions in breast tissue, increasing the likelihood of mutations and the development of cancer cells. Some of these cell divisions can lead to mutations, and over time, these mutations can accumulate and result in cancer.
Alcohol can also impact other hormones. For instance, it can raise levels of the hormone insulin-like growth factor 1 (IGF-1), which encourages cells to divide. Higher levels of IGF-1 have been associated with an increased risk of certain cancers, including breast and prostate cancer.
Additionally, alcohol can affect the liver's ability to regulate hormone levels due to the liver's role in detoxifying alcohol and metabolizing hormones. This can lead to hormonal imbalances and further increase the risk of cancer.
The hormonal effects of alcohol contribute to the risk of several cancers. Apart from breast cancer, alcohol-related hormonal imbalances can increase the risk of ovarian and endometrial cancers in women, and possibly prostate cancer in men.
So, why does alcohol pose a greater cancer risk for women? It largely comes down to our unique physiology and how our bodies process alcohol. Women generally have less body water than men of the same weight, which means alcohol becomes more concentrated in our system. On top of that, our stomachs produce less of the enzyme that breaks down alcohol before it even reaches the bloodstream. This combination means we absorb more alcohol and it takes longer to metabolize, leading to more prolonged exposure to the carcinogen acetaldehyde. This increased exposure, combined with alcohol’s tendency to disrupt our hormonal health, creates a perfect storm that elevates the risk for cancers of the breast, ovaries, and endometrium.
In addition to triggering these internal mechanisms, alcohol can increase cancer risk indirectly by making it easier for other harmful processes to take place.
Alcohol can act as a solvent, making it easier for carcinogenic chemicals — such as tobacco smoke — to enter our cells. It can also weaken our immune system, making it harder for us to fight off diseases, including cancer.
We’ve all heard it, right? That a glass of red wine with dinner is actually good for you, especially your heart. But this popular belief often glosses over a much more serious reality: the significant cancer risks tied to drinking any kind of alcohol. The truth is, when it comes to cancer, your body doesn't distinguish between a fancy Merlot and a cheap beer. The common denominator in all alcoholic drinks is ethanol, and that's where the trouble begins. All types of alcohol, whether it's wine, beer, or liquor, carry the same cancer risk because they all contain this compound.
So, what about drinking in moderation? Unfortunately, experts are clear that there is no safe amount of alcohol when it comes to cancer. Even a small amount increases your risk. While some studies have pointed to potential heart benefits from the antioxidants in red wine, these benefits simply don't outweigh the proven cancer risks. The more alcohol you consume, the higher your risk becomes. It's a straightforward relationship that puts the "healthy glass of wine" idea into a much different perspective, encouraging us to look at the complete picture of how alcohol affects our long-term health.
So how can we use this information to live healthier lives? For one, cutting back on alcohol or abstaining altogether can significantly reduce our risk.
Here are some additional changes that can make a big difference:
Together, we can navigate the journey to a healthier, happier life. Remember, every little step counts!
When it comes to alcohol and health, it helps to have a clear benchmark. Official guidelines from health organizations like the Centers for Disease Control and Prevention (CDC) provide a framework based on scientific evidence. These recommendations aren't about judgment; they're about giving you the information you need to make choices that align with your health goals. Understanding what experts consider moderate consumption is a crucial first step in evaluating your own habits. It allows you to see where you stand and decide what, if any, changes you’d like to make. Think of it as a map — it shows you the terrain so you can choose your path forward.
One of the biggest hurdles in tracking alcohol intake is knowing what a “standard drink” actually is. It’s easy to underestimate how much you’re consuming when drink sizes vary so much. According to the MD Anderson Cancer Center, one standard drink is defined as 12 ounces of beer, 5 ounces of wine, or 1.5 ounces of 80-proof liquor. That generous glass of wine you pour at home could easily count as two standard drinks. Being aware of these measurements is key to accurately assessing your consumption and understanding your risk. It’s the foundation of mindful drinking and helps you stay honest with yourself about your habits.
So, what do the experts recommend? The CDC advises that if you choose to drink, you do so in moderation. For women, this means one standard drink or less per day, and for men, it’s two standard drinks or less per day. It’s important to remember that these are upper limits for the days you do drink, not daily targets to aim for. The healthiest option is always to drink less. These guidelines are designed to help minimize health risks, including the risk of cancer. Sticking to them is a powerful way to protect your long-term well-being while still allowing yourself to enjoy a drink on occasion if you choose to.
The link between how much you drink and your cancer risk is direct and significant. It’s not just heavy drinking that poses a threat; even moderate amounts can increase your chances of developing certain cancers. According to the Canadian Cancer Society, consuming about 3.5 drinks a day can double or even triple your risk of cancers in the mouth, throat, and esophagus. The same amount increases the risk of colon and breast cancer by 1.5 times. This dose-response relationship is clear: the more you drink, the higher your risk. This knowledge is empowering because it puts the control back in your hands. Every drink you skip is a step toward lowering that risk.
If you're feeling concerned, here’s some good news: it’s never too late to make a positive change. When you stop drinking, your risk for alcohol-related cancers begins to decrease over time. While it may take many years for the risk to be fully removed, quitting is a significant and proactive step for your health. Your body has an incredible capacity for healing, and reducing its exposure to carcinogens like acetaldehyde gives it a chance to repair. This journey of mindful drinking or quitting entirely is one of the most impactful things you can do for your future self, and every day alcohol-free is a victory for your long-term health.
For anyone currently facing a cancer diagnosis or in recovery, the conversation around alcohol becomes even more critical. It’s essential to talk to your doctor about your alcohol use. Drinking can interfere with treatment, worsen side effects, and potentially increase the risk of developing new cancers. Your healthcare team can provide personalized advice based on your specific diagnosis, treatment plan, and overall health. This conversation is a vital part of your care, ensuring that your lifestyle choices support your recovery and help protect your health moving forward. Don't hesitate to bring it up; your medical team is there to support you in every aspect of your journey.
I've always heard that a glass of red wine is good for you. Is that not true when it comes to cancer? That's a common belief, but when we're talking about cancer risk, the type of alcohol doesn't matter. Whether it's wine, beer, or liquor, they all contain ethanol, which your body converts into a cancer-causing chemical. While some studies point to antioxidants in red wine for heart health, those benefits don't cancel out the proven cancer risk that comes with any alcoholic drink.
Does even light or moderate drinking really increase my cancer risk? Yes, unfortunately, the evidence is clear that even small amounts of alcohol can increase your risk for certain cancers. There isn't a "safe" threshold when it comes to cancer prevention. The relationship is straightforward: the more you drink over time, the higher your risk becomes. This is why understanding what a standard drink is and being mindful of your intake is so important.
Why is the cancer risk from alcohol higher for women? It really comes down to our physiology. Women tend to have less body water than men, which means alcohol becomes more concentrated in our systems. We also produce less of a key enzyme in our stomachs that breaks down alcohol. This combination leads to higher blood alcohol concentrations and longer exposure to its harmful byproducts, which, along with alcohol's effect on hormones like estrogen, elevates our risk.
What is the main way alcohol actually causes cancer? The primary culprit is a toxic chemical called acetaldehyde. When you drink alcohol, your body works to break it down, and acetaldehyde is the main byproduct of that process. This chemical is a known carcinogen that can directly damage the DNA in your cells and prevent your body from repairing that damage. Over time, this can lead to mutations that cause cells to grow uncontrollably.
If I cut back or stop drinking now, can I actually lower my risk? Absolutely. It's one of the most empowering things to know. While it can take time, your body has an amazing ability to heal. When you reduce or eliminate alcohol, you lower your exposure to its cancer-causing effects, and your risk for developing alcohol-related cancers begins to decrease. Every step you take toward drinking less is a positive move for your long-term health.

Scientists have established that alcohol consumption increases the risk of breast cancer through two mechanisms: elevated levels of certain hormones and potential DNA damage.
Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back on drinking gradually, with the science-backed knowledge to empower you 100% of the way. Our proven program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
The Reframe app equips you with the knowledge and skills you need to not only survive drinking less, but to thrive while you navigate the journey. Our daily research-backed readings teach you the neuroscience of alcohol, and our in-app Toolkit provides the resources and activities you need to navigate each challenge.
You’ll meet millions of fellow Reframers in our 24/7 Forum chat and daily Zoom check-in meetings. Receive encouragement from people worldwide who know exactly what you’re going through! You’ll also have the opportunity to connect with our licensed Reframe coaches for more personalized guidance.
Plus, we’re always introducing new features to optimize your in-app experience. We recently launched our in-app chatbot, Melody, powered by the world’s most powerful AI technology. Melody is here to help as you adjust to a life with less (or no) alcohol.
And that’s not all! Every month, we launch fun challenges, like Dry/Damp January, Mental Health May, and Outdoorsy June. You won’t want to miss out on the chance to participate alongside fellow Reframers (or solo if that’s more your thing!).
The Reframe app is free for 7 days, so you don’t have anything to lose by trying it. Are you ready to feel empowered and discover life beyond alcohol? Then download our app today!
We all know someone who’s been affected by breast cancer — a family member, a coworker, or a friend of a friend. It's a topic that's never far from our minds. As many as 1 in 8 women will experience it at some point, and it accounts for over 12% of new cancer cases diagnosed around the globe every year. In the U.S. alone, there are currently around 4 million women with a history of breast cancer.
However, it's not all doom and gloom. The more we understand about breast cancer and its risk factors, the more empowered we are to take control of our health.
One connection that’s often overlooked is the link between breast cancer risk and alcohol. There's been a flurry of scientific research in this area in the last few decades, and we're here to make sense of it all.
Breast cancer (like all cancers) begins when cells in the breast start growing in an uncontrolled way. These rogue cells can band together to form a lump or tumor and might even spread to other parts of the body if left unchecked.
Breast cancer comes in two major types:
While the exact "why" behind many cancers is a mystery, certain factors make breast cancer more likely.
Breast cancer isn't about who you are or where you live — women all over the globe face it, and it's the leading cancer among women. However, with knowledge and support, we can face it head-on.
Catching breast cancer early makes a world of difference, and there are several ways to do so.
Because of its impact on women and families around the world, breast cancer awareness has become a global movement. Breast Cancer Awareness Month (BCAM), observed every October, was established in the United States in 1985 as a partnership between the pharmaceutical company AstraZeneca, which produced several breast cancer drugs, and various cancer charities and organizations.
The primary aim of this initiative was two-fold:
While Breast Cancer Awareness Month started in the mid-80s, the pink ribbon symbol for breast cancer awareness came onto the scene a few years later, when an activist named Charlotte Haley began making peach-colored ribbons in her home. She distributed the ribbons with cards that read, "The National Cancer Institute's annual budget is $1.8 billion, with only 5% going to cancer prevention. Help us wake up our legislators and America by wearing this ribbon."
In 1991, the Susan G. Komen Foundation first handed out pink ribbons at a New York City race for breast cancer survivors — an event that turned the pink ribbon into the symbol we all recognize today. By 1992, several major breast cancer charities had officially adopted it as the symbol for Breast Cancer Awareness Month.
From its beginnings in the United States, Breast Cancer Awareness Month rapidly gained traction around the world. Today, it’s more than just a month on the calendar — it’s a global movement. Advancements in medical science and the power of social media have expanded the scope and reach of the awareness campaigns. Personal stories of battles fought and won, tributes to those lost, and the unwavering commitment of organizations and advocates have helped humanize the cause.
Numerous countries worldwide now recognize October as a month dedicated to breast cancer awareness, research, fundraising, and community events. Here are just a few examples:

But what does an occasional glass of wine have to do with breast cancer? It's a valid question, and we've got some science-based answers.
Over the years, the evidence has become clear and strong: the more alcohol we consume, the higher our risk of breast cancer.
Recent research has brought more insight into this connection, with several studies worldwide confirming the link between alcohol and breast cancer. Scientists report that even light to moderate drinking — up to one drink per day — significantly increased the chances of developing the disease. This risk also appears to be cumulative: the more alcohol we drink over our lifetime, the higher our risk becomes.
When we drink, our bodies convert it into a chemical called acetaldehyde — a potent carcinogen that can damage our DNA and proteins, leading to cancerous changes in cells. While our liver enzymes further break down acetaldehyde into non-toxic substances, high levels of alcohol consumption can lead to a buildup of acetaldehyde, which the liver can't process quickly enough.
This buildup of acetaldehyde may play a crucial role in the development of cancer cells. Acetaldehyde can bind to proteins and DNA in cells, causing mutations that can lead to cancer. This DNA damage is cumulative: the more alcohol we consume over time, the greater the potential for harm and the increased risk of developing cancer.
Breast tissue is particularly sensitive to this process, which explains why the risk of breast cancer is especially high.
There's another angle to consider as well. Alcohol can increase levels of estrogen and other hormones associated with breast cancer. Let’s explore this connection in more detail.
Hormones are chemical messengers produced by our endocrine glands. They travel through our bloodstream, instructing tissues and organs on what to do in our bodies. Estrogen, a primary female sex hormone, plays a vital role in a woman's reproductive cycle and overall health.
It’s responsible for the growth and development of female sexual characteristics, including the breasts. Estrogen spikes during the menstrual cycle have been linked to breast cell proliferation. While this is a natural process, an overexposure or prolonged exposure to estrogen can increase the risk of breast cancer by increasing cell division and raising the chance of DNA mutations.
Many breast cancers are estrogen-receptor-positive: they have receptors for estrogen. When estrogen binds to these receptors, it can stimulate the cancer to grow. This is why hormone therapies that reduce the body's estrogen levels or block estrogen from binding to its receptors are often used to treat these types of breast cancer.
Alcohol can increase levels of estrogen in the body in different ways:
In breast cancers that are estrogen-receptor-positive, the presence of the hormone can also accelerate tumor growth. Since alcohol increases estrogen levels, it can indirectly promote the growth of these estrogen-sensitive tumors.
While estrogen is a primary concern, alcohol also affects other hormones that can indirectly influence breast cancer risk:
While all of this might sound alarming, let's put these findings in perspective. It's important to remember that while alcohol influences hormone levels, not everyone who drinks will develop breast cancer (just as not everyone who doesn’t drink is guaranteed to not get it). In the end, this is about risk — not certainty — and factors like genetics, overall health, and other lifestyle choices all play a role. Alcohol is just one piece of the puzzle.
Still, the research is clear: this is one puzzle piece we shouldn’t ignore! The good news is that this is also a piece we have some control over.
By understanding the connection between alcohol and breast cancer, we can balance our choices to maximize our health and enjoyment of life. When it comes to reducing our risk of breast cancer, so much power is in our hands. We might not be able to change our genes, but our lifestyle choices can have a big impact on our health. Let's explore what we actually can control.
By incorporating these steps into our routine, we're not just reducing our risk of breast cancer — we're also boosting our overall health, vitality, and well-being. It's all about making choices that respect and nurture our bodies.
All in all, the journey to reduce our risk of breast cancer is one of awareness, informed decisions, and empowerment. Despite how it feels at times, we’re not alone. We're part of a community, a collective of strong individuals making daily decisions to promote our health. Every small choice matters. Every step we take towards healthier habits, like reducing our alcohol intake, is a step towards reducing our breast cancer risk!
We all know someone who’s been affected by breast cancer — a family member, a coworker, or a friend of a friend. It's a topic that's never far from our minds. As many as 1 in 8 women will experience it at some point, and it accounts for over 12% of new cancer cases diagnosed around the globe every year. In the U.S. alone, there are currently around 4 million women with a history of breast cancer.
However, it's not all doom and gloom. The more we understand about breast cancer and its risk factors, the more empowered we are to take control of our health.
One connection that’s often overlooked is the link between breast cancer risk and alcohol. There's been a flurry of scientific research in this area in the last few decades, and we're here to make sense of it all.
Breast cancer (like all cancers) begins when cells in the breast start growing in an uncontrolled way. These rogue cells can band together to form a lump or tumor and might even spread to other parts of the body if left unchecked.
Breast cancer comes in two major types:
While the exact "why" behind many cancers is a mystery, certain factors make breast cancer more likely.
Breast cancer isn't about who you are or where you live — women all over the globe face it, and it's the leading cancer among women. However, with knowledge and support, we can face it head-on.
Catching breast cancer early makes a world of difference, and there are several ways to do so.
Because of its impact on women and families around the world, breast cancer awareness has become a global movement. Breast Cancer Awareness Month (BCAM), observed every October, was established in the United States in 1985 as a partnership between the pharmaceutical company AstraZeneca, which produced several breast cancer drugs, and various cancer charities and organizations.
The primary aim of this initiative was two-fold:
While Breast Cancer Awareness Month started in the mid-80s, the pink ribbon symbol for breast cancer awareness came onto the scene a few years later, when an activist named Charlotte Haley began making peach-colored ribbons in her home. She distributed the ribbons with cards that read, "The National Cancer Institute's annual budget is $1.8 billion, with only 5% going to cancer prevention. Help us wake up our legislators and America by wearing this ribbon."
In 1991, the Susan G. Komen Foundation first handed out pink ribbons at a New York City race for breast cancer survivors — an event that turned the pink ribbon into the symbol we all recognize today. By 1992, several major breast cancer charities had officially adopted it as the symbol for Breast Cancer Awareness Month.
From its beginnings in the United States, Breast Cancer Awareness Month rapidly gained traction around the world. Today, it’s more than just a month on the calendar — it’s a global movement. Advancements in medical science and the power of social media have expanded the scope and reach of the awareness campaigns. Personal stories of battles fought and won, tributes to those lost, and the unwavering commitment of organizations and advocates have helped humanize the cause.
Numerous countries worldwide now recognize October as a month dedicated to breast cancer awareness, research, fundraising, and community events. Here are just a few examples:

But what does an occasional glass of wine have to do with breast cancer? It's a valid question, and we've got some science-based answers.
Over the years, the evidence has become clear and strong: the more alcohol we consume, the higher our risk of breast cancer.
Recent research has brought more insight into this connection, with several studies worldwide confirming the link between alcohol and breast cancer. Scientists report that even light to moderate drinking — up to one drink per day — significantly increased the chances of developing the disease. This risk also appears to be cumulative: the more alcohol we drink over our lifetime, the higher our risk becomes.
When we drink, our bodies convert it into a chemical called acetaldehyde — a potent carcinogen that can damage our DNA and proteins, leading to cancerous changes in cells. While our liver enzymes further break down acetaldehyde into non-toxic substances, high levels of alcohol consumption can lead to a buildup of acetaldehyde, which the liver can't process quickly enough.
This buildup of acetaldehyde may play a crucial role in the development of cancer cells. Acetaldehyde can bind to proteins and DNA in cells, causing mutations that can lead to cancer. This DNA damage is cumulative: the more alcohol we consume over time, the greater the potential for harm and the increased risk of developing cancer.
Breast tissue is particularly sensitive to this process, which explains why the risk of breast cancer is especially high.
There's another angle to consider as well. Alcohol can increase levels of estrogen and other hormones associated with breast cancer. Let’s explore this connection in more detail.
Hormones are chemical messengers produced by our endocrine glands. They travel through our bloodstream, instructing tissues and organs on what to do in our bodies. Estrogen, a primary female sex hormone, plays a vital role in a woman's reproductive cycle and overall health.
It’s responsible for the growth and development of female sexual characteristics, including the breasts. Estrogen spikes during the menstrual cycle have been linked to breast cell proliferation. While this is a natural process, an overexposure or prolonged exposure to estrogen can increase the risk of breast cancer by increasing cell division and raising the chance of DNA mutations.
Many breast cancers are estrogen-receptor-positive: they have receptors for estrogen. When estrogen binds to these receptors, it can stimulate the cancer to grow. This is why hormone therapies that reduce the body's estrogen levels or block estrogen from binding to its receptors are often used to treat these types of breast cancer.
Alcohol can increase levels of estrogen in the body in different ways:
In breast cancers that are estrogen-receptor-positive, the presence of the hormone can also accelerate tumor growth. Since alcohol increases estrogen levels, it can indirectly promote the growth of these estrogen-sensitive tumors.
While estrogen is a primary concern, alcohol also affects other hormones that can indirectly influence breast cancer risk:
While all of this might sound alarming, let's put these findings in perspective. It's important to remember that while alcohol influences hormone levels, not everyone who drinks will develop breast cancer (just as not everyone who doesn’t drink is guaranteed to not get it). In the end, this is about risk — not certainty — and factors like genetics, overall health, and other lifestyle choices all play a role. Alcohol is just one piece of the puzzle.
Still, the research is clear: this is one puzzle piece we shouldn’t ignore! The good news is that this is also a piece we have some control over.
By understanding the connection between alcohol and breast cancer, we can balance our choices to maximize our health and enjoyment of life. When it comes to reducing our risk of breast cancer, so much power is in our hands. We might not be able to change our genes, but our lifestyle choices can have a big impact on our health. Let's explore what we actually can control.
By incorporating these steps into our routine, we're not just reducing our risk of breast cancer — we're also boosting our overall health, vitality, and well-being. It's all about making choices that respect and nurture our bodies.
All in all, the journey to reduce our risk of breast cancer is one of awareness, informed decisions, and empowerment. Despite how it feels at times, we’re not alone. We're part of a community, a collective of strong individuals making daily decisions to promote our health. Every small choice matters. Every step we take towards healthier habits, like reducing our alcohol intake, is a step towards reducing our breast cancer risk!

Alcohol poisoning brain damage is a real risk. Learn the signs, symptoms, and steps you can take to protect your brain and support safer drinking habits.
The Reframe app is here for you! We've already helped hundreds of thousands of people just like you examine their drinking habits and develop healthier routines. We would love to do the same for you!
Everyone has a different story, and our goal is to help you understand how your relationship with alcohol has affected your life. Once you join our vibrant community, you'll receive daily Readings to help you deal with all kinds of stressors. You’ll also have 24/7 access to our Forum chat. We're an eclectic, lively bunch from all corners of the globe, all tackling similar questions and challenges.
Best of all, you can try the Reframe app for a full 7 days, completely free! There's absolutely no risk and so much potential benefit! Think about finally getting back the mental clarity, energy, and happiness you deserve. We're here to help, cheering you on to live your best life. See you soon in the app!
Nobody heads out for a birthday celebration or happy hour with friends expecting the night to end in the ER. But sometimes, one drink turns into too many, and we don't see the dangerous path we're on. This path can lead to a medical emergency and, in severe cases, permanent alcohol poisoning brain damage. The risk of long-term alcohol brain damage is real, and it happens more often than you might think. Understanding how to respond when someone has had too much is critical—and it could save a life.
Let’s start from the beginning — how does alcohol affect the brain? Alcohol, a central nervous system depressant, slows down brain function and alters its structure. Prolonged heavy drinking can lead to brain shrinkage, specifically impacting regions associated with cognition and learning, and impairing neurogenesis.
Moreover, alcohol interferes with the neurotransmitters, the chemicals that transmit signals within the brain and throughout the body. This disruption can lead to changes in mood, behavior, and bodily functions. So what does alcohol do to your brain? Let’s find out!
When we talk about heavy drinking, we’re discussing a pattern that directly exposes the brain to a toxin. According to the Better Health Channel, “Alcohol is poisonous to the brain. It can also change how the body uses nutrients, affect blood flow to the brain, and stop the brain from getting enough vitamin B1 (thiamine), which is very important.” This isn't just a minor issue; a thiamine deficiency can lead to severe and permanent brain disorders, such as Wernicke-Korsakoff syndrome, which impacts memory and coordination. Essentially, excessive alcohol consumption starves the brain of critical nutrients it needs to function and repair itself, leading to significant and lasting damage over time.
Beyond the slow-burn damage from nutrient deficiencies, alcohol poses immediate, life-threatening risks. An overdose can overwhelm the body’s systems, and as the National Institute on Alcohol Abuse and Alcoholism (NIAAA) states, “Alcohol overdose can lead to permanent brain damage or death.” This often happens because high levels of alcohol can suppress the central nervous system so much that breathing becomes dangerously slow or stops altogether. This lack of oxygen, known as hypoxia, can cause irreversible brain damage within minutes. Seizures during severe intoxication can also lead to oxygen deprivation, further compounding the harm to brain cells.
While the brain is incredibly vulnerable, it’s not the only organ at risk from heavy alcohol use. The liver, which is responsible for metabolizing alcohol, can become fatty, inflamed (alcoholic hepatitis), and eventually scarred (cirrhosis), impairing its ability to function. The heart can weaken, leading to conditions like cardiomyopathy, where the heart muscle struggles to pump blood effectively. The pancreas is also at risk for pancreatitis, a painful and dangerous inflammation. As noted by Futures Recovery, “If the brain doesn't get enough oxygen during severe alcohol poisoning (for example, during seizures), it can cause permanent brain damage,” highlighting how a single event can have cascading effects throughout the body’s most critical systems.
It’s crucial to understand what alcohol poisoning actually is and how it happens. Sober.com defines it clearly: “Alcohol poisoning, also called alcohol overdose, is a very serious and sometimes deadly problem caused by drinking too much alcohol too quickly.” When you drink, your liver works to filter the alcohol out of your blood. However, it can only process about one standard drink per hour. If you drink faster than your liver can work, your blood alcohol concentration (BAC) rises. This is the point where the toxic effects of alcohol begin to overwhelm the brain’s control over basic life-support functions like breathing, heart rate, and temperature regulation.
What many people don’t realize is that your BAC can continue to rise even after you’ve stopped drinking. Alcohol in the stomach and intestines continues to enter the bloodstream, meaning a dangerous situation can become critical even after a person has passed out. This is why it’s never safe to just “let someone sleep it off.” Understanding your own limits and practicing mindful drinking by pacing yourself, staying hydrated, and eating food can help prevent your body from becoming overwhelmed. It’s about being aware of not just what you drink, but how you drink it.
The most common path to alcohol poisoning is through binge drinking. This isn’t about having a few drinks over an entire evening; it’s about consuming a large amount in a very short period. Sober.com defines binge drinking as a pattern that brings a person’s BAC to 0.08% or higher, which typically happens after “4 or more drinks for women, or 5 or more for men, within 2 hours.” This rapid intake floods the system, giving the liver no chance to keep up. The result is a sharp spike in BAC that can quickly reach dangerous levels, leading to impaired judgment, loss of coordination, and, in severe cases, a complete shutdown of vital bodily functions.
Part of the reason people accidentally binge drink is a misunderstanding of what constitutes a “standard” drink. The NIAAA clarifies that in the U.S., “one standard drink has 0.6 fluid ounces or 14 grams of pure alcohol.” This translates to 12 ounces of regular beer (at 5% ABV), 5 ounces of wine (at 12% ABV), or 1.5 ounces of distilled spirits (at 40% ABV, or 80 proof). Think about the drinks you’re often served—a heavy-handed pour of wine, a pint of high-gravity craft beer, or a mixed drink with multiple shots. These often contain far more than one standard drink, making it easy to lose track and consume a dangerous amount of alcohol much faster than you realize.
While anyone can be at risk for alcohol poisoning, certain behaviors dramatically increase the danger. As Futures Recovery points out, “Binge drinking is the main cause. This means drinking a lot of alcohol in a short time.” This single factor—speed of consumption—is the most significant contributor. However, other elements play a role as well. Your body size and weight, whether you’ve eaten recently, your overall health, and your individual tolerance level all influence how quickly your BAC rises. Someone who rarely drinks may be at higher risk than a regular drinker, but even those with a high tolerance can easily cross the line into overdose territory during a binge.
Combining alcohol with other substances is one of the most dangerous things you can do. The Better Health Channel warns, “Mixing alcohol with other drugs (like opioids) is very dangerous and greatly increases the risk.” Alcohol is a central nervous system depressant, and when you mix it with other depressants—such as opioids, sedatives, or even some over-the-counter cold medications—you create a synergistic effect. This means the combined impact is far greater than the sum of its parts. This combination can severely slow breathing and heart rate, leading to respiratory failure, coma, and death. It’s a risk that is simply not worth taking.
Your personal biology and history also contribute to your risk. The Better Health Channel notes, “People who drink heavily for a long time are most at risk. However, even binge drinking can cause brain damage in just a few years.” Factors like age, gender, genetics, and pre-existing health conditions can affect how your body metabolizes alcohol. For example, women tend to have a higher BAC than men after consuming the same amount of alcohol. Understanding how these factors apply to you is key to making safer choices. Using a tool like a Blood Alcohol Content (BAC) calculator can provide a rough estimate, but it’s always wisest to err on the side of caution.
How does alcohol poisoning fit into all this? Consuming alcohol faster than our liver can process it overloads our system, causing a rapid increase in our blood alcohol concentration (BAC). A BAC that’s too high can lead to alcohol poisoning.
BAC levels higher than 0.3% can potentially be life-threatening, causing breathing difficulties and seizures. The effects of alcohol on the brain during binge drinking can be fatal. Although you might not be thinking about brain damage from alcohol when you sit down at the bar, things can take a dark turn if you aren’t careful.
During an episode of alcohol poisoning, the high level of alcohol depresses the nervous system so much that it can't perform its regular functions, such as controlling heart rate and breathing. This acute stress can trigger inflammation and oxidative stress in the brain — the sudden spike can impair the brain's ability to function properly, leading to unconsciousness, respiratory failure, and even death.
For this reason, alcohol poisoning is not a mere hangover — it's a medical emergency! In the most severe cases, it can result in alcohol-related brain damage (ARBD), characterized by cognitive deficits, impaired executive function, and difficulty with balance.
Knowing the signs of alcohol poisoning can be the difference between life and death. It’s not just about being very drunk; it’s a serious medical state. According to the National Institute on Alcohol Abuse and Alcoholism (NIAAA), key symptoms include mental confusion, vomiting, and seizures. You might also notice someone has trouble staying conscious, very slow breathing (fewer than eight breaths a minute), a slow heart rate, or clammy skin. Another critical sign is a dulled gag reflex, which is dangerous because it can lead to choking on vomit. An extremely low body temperature, which can cause the skin to look pale or bluish, is also a major red flag.
If you suspect someone has alcohol poisoning, treat it as the emergency it is. The most important step is to call 911 immediately. Don't wait for all the symptoms to appear or second-guess yourself. While you wait for medical help to arrive, try to keep the person awake and sitting up. If they must lie down, turn them onto their side to prevent them from choking if they vomit — this is known as the recovery position. Never leave them alone. Having someone there to monitor their breathing and consciousness can provide crucial information to the paramedics when they arrive.
There are many myths about how to sober someone up, and trying them can make a dangerous situation even worse. The NIAAA warns against common but ineffective methods. Do not give the person coffee; caffeine can dehydrate them further. Do not put them in a cold shower, as this can increase the risk of hypothermia, especially since their body temperature may already be dangerously low. Trying to make them walk it off is also a bad idea, as it can lead to falls and injuries. None of these "remedies" will lower a person's BAC, and they can create additional complications for someone in a vulnerable state.
One of the most dangerous mistakes you can make is assuming an unconscious person will simply "sleep it off." Even after someone stops drinking and passes out, their body continues to absorb alcohol from their stomach into their bloodstream. This means their BAC can keep rising to a fatal level. An unconscious person is also at high risk of choking on their own vomit because their gag reflex is suppressed. Never leave an unconscious person alone. Stay with them and get medical help right away.
So, what’s actually happening in the body during an overdose? Alcohol poisoning occurs when you drink a large amount of alcohol in a short period, overwhelming your liver's ability to process it. This causes your blood alcohol content (BAC) to spike to dangerous levels. Alcohol is a depressant, meaning it slows down brain functions. When your BAC gets too high, it can start to shut down the critical areas of your brain that control essential life-sustaining functions like breathing, heart rate, and body temperature. This isn't just a more intense version of being drunk; it's a life-threatening medical event that can cause permanent brain damage or death.
Understanding how BAC works is key to understanding the risk of an overdose. When you drink, alcohol is absorbed into your bloodstream through your stomach and small intestine. As the NIAAA explains, this process continues even after you’ve stopped drinking. This is why someone can seem fine one moment and be in serious trouble the next. Their BAC can continue to climb long after their last sip, especially if they drank a lot very quickly. If you're curious about how different factors affect your own BAC, you can use a Blood Alcohol Content (BAC) calculator to get a better sense of how your body processes alcohol.
Alcohol poisoning progresses through distinct stages as BAC levels rise. At a BAC of .11 to .15, the body often tries to expel the toxin, leading to vomiting. As the BAC climbs to between .17 and .30, a person may experience a blackout, where the brain temporarily stops recording memories. This is a sign of severe impairment. The most dangerous stage occurs when BAC reaches .31 or higher. At this point, the body’s vital functions can shut down, leading to a coma or even death. Recognizing these escalating signs is crucial for intervening before it’s too late.
When someone is hospitalized for alcohol poisoning, they receive immediate medical care to manage their symptoms and prevent long-term damage. This isn't something that can be treated at home. Medical professionals will carefully monitor their vital signs, including their heart rate and breathing. They might provide oxygen through a mask or insert a tube to help with breathing. An IV is often used to deliver fluids, which helps prevent dehydration and flush toxins from the body. They may also administer vitamins and glucose to prevent other serious complications associated with alcohol poisoning. In some cases, they may even pump the stomach to remove any unabsorbed alcohol.
If detected early, ARBD can be partially reversed with abstinence or a significant reduction in alcohol intake. Our brains are incredibly resilient: research has shown that after a period of abstinence, some damage can be reversed, and cognitive function can improve.
However, persistent episodes of alcohol poisoning can potentially cause brain damage to be permanent, eventually leading to Wernicke-Korsakoff syndrome, a severe form of ARBD.
Wernicke-Korsakoff syndrome comprises two separate conditions: Wernicke's encephalopathy and Korsakoff's psychosis. Wernicke's encephalopathy is a short-term but severe condition caused by a lack of vitamin B1 (thiamine) commonly seen in heavy drinkers. It is characterized by mental confusion, oculomotor disturbances (problems with eye movements), and difficulty with muscle coordination. If left untreated, this condition can lead to irreversible brain damage and even death.
If not treated immediately, it can lead to Korsakoff's psychosis, a long-term condition marked by learning and memory problems. While people with this condition may be able to recall events from long ago, they often struggle with new information or recent memories. They might also experience hallucinations or make up events to fill in memory gaps, a phenomenon known as confabulation.
Unfortunately, there's no specific cure for WKS. However, thiamine can be administered to prevent further deterioration of the brain, and in some cases, it may reverse some of the symptoms of Wernicke's encephalopathy and brain damage from alcohol.
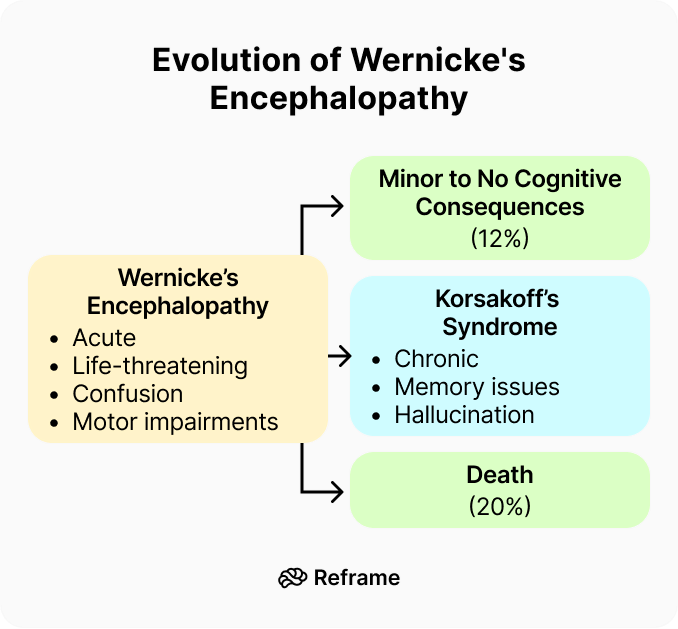
Alcohol-related brain damage, or ARBD, isn't a single condition but an umbrella term for the harm that can happen to the brain from long-term heavy drinking. It’s a direct result of alcohol's toxic effects on brain cells, often worsened by the nutritional gaps that can come with heavy alcohol use. Unlike other forms of dementia, the progression of ARBD can often be stopped — and sometimes even partially reversed — if a person stops drinking and gets the right support. This potential for recovery is a powerful motivator and makes catching the signs early absolutely critical for protecting your long-term health.
When we think of brain damage, memory loss is usually the first thing that comes to mind. But with ARBD, the symptoms are much broader and can impact your entire life. It can affect your ability to think clearly, make sound decisions, and plan your day. According to the Alzheimer's Society, you might find it hard to focus on tasks, feel unusually irritable or sad, or struggle with balance and coordination. Forgetting recent conversations, having trouble with planning, and experiencing sudden mood swings are all common signs. It’s a condition that affects your cognitive and physical well-being, not just your ability to recall information.
As we touched on earlier, one of the most severe forms of ARBD is Wernicke-Korsakoff syndrome (WKS). This isn't just one disease, but two distinct stages that are linked. First comes Wernicke's encephalopathy, an acute condition caused by a severe deficiency of thiamine (vitamin B1). This can lead to confusion, vision problems, and a loss of muscle coordination. If it’s not treated right away with high-dose thiamine, it can progress to Korsakoff's syndrome, a chronic and more permanent condition defined by severe short-term memory loss and difficulty forming new memories.
While any pattern of heavy, long-term drinking increases the risk of ARBD, some people are more vulnerable than others. It’s not just about how much you drink on a single occasion, but the cumulative effect of alcohol over months and years. Factors like your genetics, general health, and nutrition also play a significant role in how your body and brain respond to alcohol. Understanding the risk factors can help you recognize the warning signs in yourself or a loved one before the damage becomes more serious.
The numbers might be higher than you think. Research suggests that about one in three people who are dependent on alcohol show some signs of ARBD. The risk starts to climb for anyone regularly drinking 25 or more units per week — that’s equivalent to about eight pints of strong beer or just over two bottles of wine spread across the week. Consistent drinking above these levels can begin to impact your thinking skills and memory over time. It’s a stark reminder that what might feel like a normal habit can have serious long-term consequences for your brain health.
One of the most surprising things about ARBD is the age at which it typically appears. While we often associate dementia with older age, ARBD usually develops in people between 40 and 60. This is significantly younger than the typical onset for conditions like Alzheimer's. It tends to affect more men than women, largely because, historically, men have had higher rates of heavy drinking. Recognizing that ARBD can affect people in the prime of their lives underscores the importance of addressing drinking habits early on to protect your future.
Let's be clear: not every person who enjoys an occasional drink is destined for brain damage. It's all about understanding our limits and forming habits that ensure we drink responsibly. Here are five ways to do just that:
We live in a world where alcohol is often at the heart of social events. We don’t want to miss out on the fun of socializing and spending time with people we love … but we need to look after our health and to make sure we're not veering into dangerous territory. Does alcohol cause brain damage? Yes, but with the right decisions, we can stay safe. No alcohol poisoning or potential brain damage for us! Armed with knowledge, and by practicing responsible drinking habits, we can be part of the fun while socializing safely.
If you're worried about the impact alcohol is having on your brain, the first and most important step is to talk to a healthcare professional. While it can be scary to think about, there’s some good news. If it’s caught early, some alcohol-related brain damage can be reversed by stopping or significantly reducing your drinking. Our brains have an amazing capacity for healing; research shows that after a period of abstinence, some cognitive functions can improve. A doctor can help you create a safe plan to cut back and can also check for common nutritional deficiencies, like a lack of thiamine (vitamin B1), which can contribute to brain-related issues.
For those who drink heavily and consistently, the stakes are higher. Repeated episodes of alcohol poisoning can lead to permanent brain damage and may result in severe conditions like Wernicke-Korsakoff syndrome. This is why professional medical advice is not just helpful—it's critical. If you have a physical dependence on alcohol, quitting abruptly without medical supervision can be dangerous and lead to severe withdrawal symptoms. A doctor can provide the support and resources needed to manage withdrawal safely, setting you on a path toward recovery without risking your health further. Please don't try to go it alone.
If you or a loved one is dealing with ARBD, recovery is centered on a few key strategies. The most critical action is to stop drinking alcohol, which halts further damage and gives the brain a chance to heal. Alongside this, nutrition plays a huge role. As mentioned, many heavy drinkers are deficient in thiamine, which can cause severe neurological problems like Wernicke's encephalopathy. A doctor will often recommend thiamine supplements and a balanced diet rich in vitamins and minerals. Engaging in cognitive exercises, staying physically active, and maintaining a structured daily routine can also support brain function and help rebuild neural pathways.
Protecting your brain doesn't have to be an all-or-nothing battle. It’s really about understanding your personal limits and creating habits that support responsible drinking. This shift in mindset is powerful because it puts you back in control. Instead of focusing on what you’re giving up, you can focus on what you’re gaining: better health, clearer thinking, and more energy. The key is to start small. You don’t have to overhaul your entire life overnight. Begin by simply becoming more aware of your patterns. How much are you really drinking in a week? How does it make you feel the next day?
Once you have a clearer picture, you can set realistic goals. Maybe it’s committing to two alcohol-free days a week or deciding you’ll have only one drink at your next social gathering. Tools and apps designed for habit change, like Reframe, can be incredibly helpful for tracking your progress and providing support when you need it. Exploring the world of non-alcoholic cocktails or finding new hobbies that don’t revolve around drinking can also make the process feel less like a sacrifice and more like an exciting new chapter. You can find answers to common questions about this process in our FAQ section.
A great way to build healthier habits is to practice mindful drinking. This just means being more present and intentional with your choices around alcohol. It’s about asking yourself *why* you want a drink instead of reaching for one automatically. A simple mindful technique is to always eat a meal before you drink. Having food in your stomach slows the absorption of alcohol, giving your body more time to process it. Other practices include sipping your drink slowly to savor it, alternating each alcoholic beverage with a glass of water, and pausing before you get a refill to check in with how you’re feeling.
What’s the difference between being really drunk and having alcohol poisoning? Think of it this way: being drunk affects your coordination, judgment, and mood. Alcohol poisoning is a medical emergency where the amount of alcohol in your bloodstream is so high that it starts to shut down the parts of your brain that control basic life-support functions. If you see someone who is confused, vomiting, breathing very slowly, or can't be woken up, it's no longer about being drunk—it's a potential overdose that requires an immediate 911 call.
Can just one night of heavy drinking cause permanent brain damage? A single episode of severe alcohol poisoning can cause permanent brain damage, but not in the way you might think. The immediate danger comes from the body being deprived of oxygen, either from breathing that slows or stops, or from seizures. This lack of oxygen can harm brain cells. The more gradual brain damage, often called ARBD, typically develops from a pattern of heavy drinking over many years.
If someone passes out from drinking, isn't it best to just let them sleep it off? This is one of the most dangerous myths about alcohol. A person's blood alcohol level can continue to rise even after they've stopped drinking and passed out. This means they can go from being unconscious to having a fatal overdose while they're "sleeping." They are also at serious risk of choking if they vomit, as their gag reflex is suppressed. An unconscious person needs monitoring and immediate medical help.
Is brain damage from alcohol always permanent? Not always. The brain has a remarkable ability to heal. When someone stops drinking, especially if the damage is caught early, they can often see improvements in their cognitive function and memory. The key is to stop the exposure to alcohol to prevent further harm and give the brain a chance to recover. However, in very severe and long-term cases, such as Wernicke-Korsakoff syndrome, the damage can be lasting.
How do I know if I’m binge drinking if I don’t feel that drunk? Binge drinking is defined by the amount of alcohol consumed in a short time, not by how you feel. It's typically defined as having four or more drinks for women, or five or more for men, within about two hours. It's easy to hit this number without realizing it, especially since many cocktails, glasses of wine, or craft beers contain more than one "standard" serving of alcohol. It’s about the math, not the buzz.
Nobody heads out for a birthday celebration or happy hour with friends expecting the night to end in the ER. But sometimes, one drink turns into too many, and we don't see the dangerous path we're on. This path can lead to a medical emergency and, in severe cases, permanent alcohol poisoning brain damage. The risk of long-term alcohol brain damage is real, and it happens more often than you might think. Understanding how to respond when someone has had too much is critical—and it could save a life.
Let’s start from the beginning — how does alcohol affect the brain? Alcohol, a central nervous system depressant, slows down brain function and alters its structure. Prolonged heavy drinking can lead to brain shrinkage, specifically impacting regions associated with cognition and learning, and impairing neurogenesis.
Moreover, alcohol interferes with the neurotransmitters, the chemicals that transmit signals within the brain and throughout the body. This disruption can lead to changes in mood, behavior, and bodily functions. So what does alcohol do to your brain? Let’s find out!
When we talk about heavy drinking, we’re discussing a pattern that directly exposes the brain to a toxin. According to the Better Health Channel, “Alcohol is poisonous to the brain. It can also change how the body uses nutrients, affect blood flow to the brain, and stop the brain from getting enough vitamin B1 (thiamine), which is very important.” This isn't just a minor issue; a thiamine deficiency can lead to severe and permanent brain disorders, such as Wernicke-Korsakoff syndrome, which impacts memory and coordination. Essentially, excessive alcohol consumption starves the brain of critical nutrients it needs to function and repair itself, leading to significant and lasting damage over time.
Beyond the slow-burn damage from nutrient deficiencies, alcohol poses immediate, life-threatening risks. An overdose can overwhelm the body’s systems, and as the National Institute on Alcohol Abuse and Alcoholism (NIAAA) states, “Alcohol overdose can lead to permanent brain damage or death.” This often happens because high levels of alcohol can suppress the central nervous system so much that breathing becomes dangerously slow or stops altogether. This lack of oxygen, known as hypoxia, can cause irreversible brain damage within minutes. Seizures during severe intoxication can also lead to oxygen deprivation, further compounding the harm to brain cells.
While the brain is incredibly vulnerable, it’s not the only organ at risk from heavy alcohol use. The liver, which is responsible for metabolizing alcohol, can become fatty, inflamed (alcoholic hepatitis), and eventually scarred (cirrhosis), impairing its ability to function. The heart can weaken, leading to conditions like cardiomyopathy, where the heart muscle struggles to pump blood effectively. The pancreas is also at risk for pancreatitis, a painful and dangerous inflammation. As noted by Futures Recovery, “If the brain doesn't get enough oxygen during severe alcohol poisoning (for example, during seizures), it can cause permanent brain damage,” highlighting how a single event can have cascading effects throughout the body’s most critical systems.
It’s crucial to understand what alcohol poisoning actually is and how it happens. Sober.com defines it clearly: “Alcohol poisoning, also called alcohol overdose, is a very serious and sometimes deadly problem caused by drinking too much alcohol too quickly.” When you drink, your liver works to filter the alcohol out of your blood. However, it can only process about one standard drink per hour. If you drink faster than your liver can work, your blood alcohol concentration (BAC) rises. This is the point where the toxic effects of alcohol begin to overwhelm the brain’s control over basic life-support functions like breathing, heart rate, and temperature regulation.
What many people don’t realize is that your BAC can continue to rise even after you’ve stopped drinking. Alcohol in the stomach and intestines continues to enter the bloodstream, meaning a dangerous situation can become critical even after a person has passed out. This is why it’s never safe to just “let someone sleep it off.” Understanding your own limits and practicing mindful drinking by pacing yourself, staying hydrated, and eating food can help prevent your body from becoming overwhelmed. It’s about being aware of not just what you drink, but how you drink it.
The most common path to alcohol poisoning is through binge drinking. This isn’t about having a few drinks over an entire evening; it’s about consuming a large amount in a very short period. Sober.com defines binge drinking as a pattern that brings a person’s BAC to 0.08% or higher, which typically happens after “4 or more drinks for women, or 5 or more for men, within 2 hours.” This rapid intake floods the system, giving the liver no chance to keep up. The result is a sharp spike in BAC that can quickly reach dangerous levels, leading to impaired judgment, loss of coordination, and, in severe cases, a complete shutdown of vital bodily functions.
Part of the reason people accidentally binge drink is a misunderstanding of what constitutes a “standard” drink. The NIAAA clarifies that in the U.S., “one standard drink has 0.6 fluid ounces or 14 grams of pure alcohol.” This translates to 12 ounces of regular beer (at 5% ABV), 5 ounces of wine (at 12% ABV), or 1.5 ounces of distilled spirits (at 40% ABV, or 80 proof). Think about the drinks you’re often served—a heavy-handed pour of wine, a pint of high-gravity craft beer, or a mixed drink with multiple shots. These often contain far more than one standard drink, making it easy to lose track and consume a dangerous amount of alcohol much faster than you realize.
While anyone can be at risk for alcohol poisoning, certain behaviors dramatically increase the danger. As Futures Recovery points out, “Binge drinking is the main cause. This means drinking a lot of alcohol in a short time.” This single factor—speed of consumption—is the most significant contributor. However, other elements play a role as well. Your body size and weight, whether you’ve eaten recently, your overall health, and your individual tolerance level all influence how quickly your BAC rises. Someone who rarely drinks may be at higher risk than a regular drinker, but even those with a high tolerance can easily cross the line into overdose territory during a binge.
Combining alcohol with other substances is one of the most dangerous things you can do. The Better Health Channel warns, “Mixing alcohol with other drugs (like opioids) is very dangerous and greatly increases the risk.” Alcohol is a central nervous system depressant, and when you mix it with other depressants—such as opioids, sedatives, or even some over-the-counter cold medications—you create a synergistic effect. This means the combined impact is far greater than the sum of its parts. This combination can severely slow breathing and heart rate, leading to respiratory failure, coma, and death. It’s a risk that is simply not worth taking.
Your personal biology and history also contribute to your risk. The Better Health Channel notes, “People who drink heavily for a long time are most at risk. However, even binge drinking can cause brain damage in just a few years.” Factors like age, gender, genetics, and pre-existing health conditions can affect how your body metabolizes alcohol. For example, women tend to have a higher BAC than men after consuming the same amount of alcohol. Understanding how these factors apply to you is key to making safer choices. Using a tool like a Blood Alcohol Content (BAC) calculator can provide a rough estimate, but it’s always wisest to err on the side of caution.
How does alcohol poisoning fit into all this? Consuming alcohol faster than our liver can process it overloads our system, causing a rapid increase in our blood alcohol concentration (BAC). A BAC that’s too high can lead to alcohol poisoning.
BAC levels higher than 0.3% can potentially be life-threatening, causing breathing difficulties and seizures. The effects of alcohol on the brain during binge drinking can be fatal. Although you might not be thinking about brain damage from alcohol when you sit down at the bar, things can take a dark turn if you aren’t careful.
During an episode of alcohol poisoning, the high level of alcohol depresses the nervous system so much that it can't perform its regular functions, such as controlling heart rate and breathing. This acute stress can trigger inflammation and oxidative stress in the brain — the sudden spike can impair the brain's ability to function properly, leading to unconsciousness, respiratory failure, and even death.
For this reason, alcohol poisoning is not a mere hangover — it's a medical emergency! In the most severe cases, it can result in alcohol-related brain damage (ARBD), characterized by cognitive deficits, impaired executive function, and difficulty with balance.
Knowing the signs of alcohol poisoning can be the difference between life and death. It’s not just about being very drunk; it’s a serious medical state. According to the National Institute on Alcohol Abuse and Alcoholism (NIAAA), key symptoms include mental confusion, vomiting, and seizures. You might also notice someone has trouble staying conscious, very slow breathing (fewer than eight breaths a minute), a slow heart rate, or clammy skin. Another critical sign is a dulled gag reflex, which is dangerous because it can lead to choking on vomit. An extremely low body temperature, which can cause the skin to look pale or bluish, is also a major red flag.
If you suspect someone has alcohol poisoning, treat it as the emergency it is. The most important step is to call 911 immediately. Don't wait for all the symptoms to appear or second-guess yourself. While you wait for medical help to arrive, try to keep the person awake and sitting up. If they must lie down, turn them onto their side to prevent them from choking if they vomit — this is known as the recovery position. Never leave them alone. Having someone there to monitor their breathing and consciousness can provide crucial information to the paramedics when they arrive.
There are many myths about how to sober someone up, and trying them can make a dangerous situation even worse. The NIAAA warns against common but ineffective methods. Do not give the person coffee; caffeine can dehydrate them further. Do not put them in a cold shower, as this can increase the risk of hypothermia, especially since their body temperature may already be dangerously low. Trying to make them walk it off is also a bad idea, as it can lead to falls and injuries. None of these "remedies" will lower a person's BAC, and they can create additional complications for someone in a vulnerable state.
One of the most dangerous mistakes you can make is assuming an unconscious person will simply "sleep it off." Even after someone stops drinking and passes out, their body continues to absorb alcohol from their stomach into their bloodstream. This means their BAC can keep rising to a fatal level. An unconscious person is also at high risk of choking on their own vomit because their gag reflex is suppressed. Never leave an unconscious person alone. Stay with them and get medical help right away.
So, what’s actually happening in the body during an overdose? Alcohol poisoning occurs when you drink a large amount of alcohol in a short period, overwhelming your liver's ability to process it. This causes your blood alcohol content (BAC) to spike to dangerous levels. Alcohol is a depressant, meaning it slows down brain functions. When your BAC gets too high, it can start to shut down the critical areas of your brain that control essential life-sustaining functions like breathing, heart rate, and body temperature. This isn't just a more intense version of being drunk; it's a life-threatening medical event that can cause permanent brain damage or death.
Understanding how BAC works is key to understanding the risk of an overdose. When you drink, alcohol is absorbed into your bloodstream through your stomach and small intestine. As the NIAAA explains, this process continues even after you’ve stopped drinking. This is why someone can seem fine one moment and be in serious trouble the next. Their BAC can continue to climb long after their last sip, especially if they drank a lot very quickly. If you're curious about how different factors affect your own BAC, you can use a Blood Alcohol Content (BAC) calculator to get a better sense of how your body processes alcohol.
Alcohol poisoning progresses through distinct stages as BAC levels rise. At a BAC of .11 to .15, the body often tries to expel the toxin, leading to vomiting. As the BAC climbs to between .17 and .30, a person may experience a blackout, where the brain temporarily stops recording memories. This is a sign of severe impairment. The most dangerous stage occurs when BAC reaches .31 or higher. At this point, the body’s vital functions can shut down, leading to a coma or even death. Recognizing these escalating signs is crucial for intervening before it’s too late.
When someone is hospitalized for alcohol poisoning, they receive immediate medical care to manage their symptoms and prevent long-term damage. This isn't something that can be treated at home. Medical professionals will carefully monitor their vital signs, including their heart rate and breathing. They might provide oxygen through a mask or insert a tube to help with breathing. An IV is often used to deliver fluids, which helps prevent dehydration and flush toxins from the body. They may also administer vitamins and glucose to prevent other serious complications associated with alcohol poisoning. In some cases, they may even pump the stomach to remove any unabsorbed alcohol.
If detected early, ARBD can be partially reversed with abstinence or a significant reduction in alcohol intake. Our brains are incredibly resilient: research has shown that after a period of abstinence, some damage can be reversed, and cognitive function can improve.
However, persistent episodes of alcohol poisoning can potentially cause brain damage to be permanent, eventually leading to Wernicke-Korsakoff syndrome, a severe form of ARBD.
Wernicke-Korsakoff syndrome comprises two separate conditions: Wernicke's encephalopathy and Korsakoff's psychosis. Wernicke's encephalopathy is a short-term but severe condition caused by a lack of vitamin B1 (thiamine) commonly seen in heavy drinkers. It is characterized by mental confusion, oculomotor disturbances (problems with eye movements), and difficulty with muscle coordination. If left untreated, this condition can lead to irreversible brain damage and even death.
If not treated immediately, it can lead to Korsakoff's psychosis, a long-term condition marked by learning and memory problems. While people with this condition may be able to recall events from long ago, they often struggle with new information or recent memories. They might also experience hallucinations or make up events to fill in memory gaps, a phenomenon known as confabulation.
Unfortunately, there's no specific cure for WKS. However, thiamine can be administered to prevent further deterioration of the brain, and in some cases, it may reverse some of the symptoms of Wernicke's encephalopathy and brain damage from alcohol.
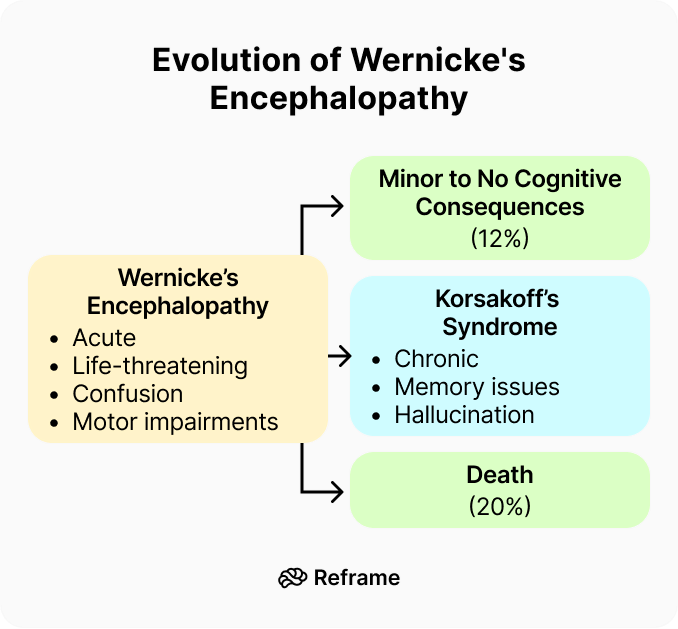
Alcohol-related brain damage, or ARBD, isn't a single condition but an umbrella term for the harm that can happen to the brain from long-term heavy drinking. It’s a direct result of alcohol's toxic effects on brain cells, often worsened by the nutritional gaps that can come with heavy alcohol use. Unlike other forms of dementia, the progression of ARBD can often be stopped — and sometimes even partially reversed — if a person stops drinking and gets the right support. This potential for recovery is a powerful motivator and makes catching the signs early absolutely critical for protecting your long-term health.
When we think of brain damage, memory loss is usually the first thing that comes to mind. But with ARBD, the symptoms are much broader and can impact your entire life. It can affect your ability to think clearly, make sound decisions, and plan your day. According to the Alzheimer's Society, you might find it hard to focus on tasks, feel unusually irritable or sad, or struggle with balance and coordination. Forgetting recent conversations, having trouble with planning, and experiencing sudden mood swings are all common signs. It’s a condition that affects your cognitive and physical well-being, not just your ability to recall information.
As we touched on earlier, one of the most severe forms of ARBD is Wernicke-Korsakoff syndrome (WKS). This isn't just one disease, but two distinct stages that are linked. First comes Wernicke's encephalopathy, an acute condition caused by a severe deficiency of thiamine (vitamin B1). This can lead to confusion, vision problems, and a loss of muscle coordination. If it’s not treated right away with high-dose thiamine, it can progress to Korsakoff's syndrome, a chronic and more permanent condition defined by severe short-term memory loss and difficulty forming new memories.
While any pattern of heavy, long-term drinking increases the risk of ARBD, some people are more vulnerable than others. It’s not just about how much you drink on a single occasion, but the cumulative effect of alcohol over months and years. Factors like your genetics, general health, and nutrition also play a significant role in how your body and brain respond to alcohol. Understanding the risk factors can help you recognize the warning signs in yourself or a loved one before the damage becomes more serious.
The numbers might be higher than you think. Research suggests that about one in three people who are dependent on alcohol show some signs of ARBD. The risk starts to climb for anyone regularly drinking 25 or more units per week — that’s equivalent to about eight pints of strong beer or just over two bottles of wine spread across the week. Consistent drinking above these levels can begin to impact your thinking skills and memory over time. It’s a stark reminder that what might feel like a normal habit can have serious long-term consequences for your brain health.
One of the most surprising things about ARBD is the age at which it typically appears. While we often associate dementia with older age, ARBD usually develops in people between 40 and 60. This is significantly younger than the typical onset for conditions like Alzheimer's. It tends to affect more men than women, largely because, historically, men have had higher rates of heavy drinking. Recognizing that ARBD can affect people in the prime of their lives underscores the importance of addressing drinking habits early on to protect your future.
Let's be clear: not every person who enjoys an occasional drink is destined for brain damage. It's all about understanding our limits and forming habits that ensure we drink responsibly. Here are five ways to do just that:
We live in a world where alcohol is often at the heart of social events. We don’t want to miss out on the fun of socializing and spending time with people we love … but we need to look after our health and to make sure we're not veering into dangerous territory. Does alcohol cause brain damage? Yes, but with the right decisions, we can stay safe. No alcohol poisoning or potential brain damage for us! Armed with knowledge, and by practicing responsible drinking habits, we can be part of the fun while socializing safely.
If you're worried about the impact alcohol is having on your brain, the first and most important step is to talk to a healthcare professional. While it can be scary to think about, there’s some good news. If it’s caught early, some alcohol-related brain damage can be reversed by stopping or significantly reducing your drinking. Our brains have an amazing capacity for healing; research shows that after a period of abstinence, some cognitive functions can improve. A doctor can help you create a safe plan to cut back and can also check for common nutritional deficiencies, like a lack of thiamine (vitamin B1), which can contribute to brain-related issues.
For those who drink heavily and consistently, the stakes are higher. Repeated episodes of alcohol poisoning can lead to permanent brain damage and may result in severe conditions like Wernicke-Korsakoff syndrome. This is why professional medical advice is not just helpful—it's critical. If you have a physical dependence on alcohol, quitting abruptly without medical supervision can be dangerous and lead to severe withdrawal symptoms. A doctor can provide the support and resources needed to manage withdrawal safely, setting you on a path toward recovery without risking your health further. Please don't try to go it alone.
If you or a loved one is dealing with ARBD, recovery is centered on a few key strategies. The most critical action is to stop drinking alcohol, which halts further damage and gives the brain a chance to heal. Alongside this, nutrition plays a huge role. As mentioned, many heavy drinkers are deficient in thiamine, which can cause severe neurological problems like Wernicke's encephalopathy. A doctor will often recommend thiamine supplements and a balanced diet rich in vitamins and minerals. Engaging in cognitive exercises, staying physically active, and maintaining a structured daily routine can also support brain function and help rebuild neural pathways.
Protecting your brain doesn't have to be an all-or-nothing battle. It’s really about understanding your personal limits and creating habits that support responsible drinking. This shift in mindset is powerful because it puts you back in control. Instead of focusing on what you’re giving up, you can focus on what you’re gaining: better health, clearer thinking, and more energy. The key is to start small. You don’t have to overhaul your entire life overnight. Begin by simply becoming more aware of your patterns. How much are you really drinking in a week? How does it make you feel the next day?
Once you have a clearer picture, you can set realistic goals. Maybe it’s committing to two alcohol-free days a week or deciding you’ll have only one drink at your next social gathering. Tools and apps designed for habit change, like Reframe, can be incredibly helpful for tracking your progress and providing support when you need it. Exploring the world of non-alcoholic cocktails or finding new hobbies that don’t revolve around drinking can also make the process feel less like a sacrifice and more like an exciting new chapter. You can find answers to common questions about this process in our FAQ section.
A great way to build healthier habits is to practice mindful drinking. This just means being more present and intentional with your choices around alcohol. It’s about asking yourself *why* you want a drink instead of reaching for one automatically. A simple mindful technique is to always eat a meal before you drink. Having food in your stomach slows the absorption of alcohol, giving your body more time to process it. Other practices include sipping your drink slowly to savor it, alternating each alcoholic beverage with a glass of water, and pausing before you get a refill to check in with how you’re feeling.
What’s the difference between being really drunk and having alcohol poisoning? Think of it this way: being drunk affects your coordination, judgment, and mood. Alcohol poisoning is a medical emergency where the amount of alcohol in your bloodstream is so high that it starts to shut down the parts of your brain that control basic life-support functions. If you see someone who is confused, vomiting, breathing very slowly, or can't be woken up, it's no longer about being drunk—it's a potential overdose that requires an immediate 911 call.
Can just one night of heavy drinking cause permanent brain damage? A single episode of severe alcohol poisoning can cause permanent brain damage, but not in the way you might think. The immediate danger comes from the body being deprived of oxygen, either from breathing that slows or stops, or from seizures. This lack of oxygen can harm brain cells. The more gradual brain damage, often called ARBD, typically develops from a pattern of heavy drinking over many years.
If someone passes out from drinking, isn't it best to just let them sleep it off? This is one of the most dangerous myths about alcohol. A person's blood alcohol level can continue to rise even after they've stopped drinking and passed out. This means they can go from being unconscious to having a fatal overdose while they're "sleeping." They are also at serious risk of choking if they vomit, as their gag reflex is suppressed. An unconscious person needs monitoring and immediate medical help.
Is brain damage from alcohol always permanent? Not always. The brain has a remarkable ability to heal. When someone stops drinking, especially if the damage is caught early, they can often see improvements in their cognitive function and memory. The key is to stop the exposure to alcohol to prevent further harm and give the brain a chance to recover. However, in very severe and long-term cases, such as Wernicke-Korsakoff syndrome, the damage can be lasting.
How do I know if I’m binge drinking if I don’t feel that drunk? Binge drinking is defined by the amount of alcohol consumed in a short time, not by how you feel. It's typically defined as having four or more drinks for women, or five or more for men, within about two hours. It's easy to hit this number without realizing it, especially since many cocktails, glasses of wine, or craft beers contain more than one "standard" serving of alcohol. It’s about the math, not the buzz.

Research shows that excessive alcohol consumption can lead to liver cirrhosis — and even moderate drinking can cause liver damage over an extended period of time.
Ready to give your liver a break and change your drinking patterns? Although it isn’t a treatment for alcohol use disorder (AUD), the Reframe app can help you cut back or quit. Our science-backed program has helped millions of people around the world drink less and live more. And we want to help you get there, too!
When you download the Reframe app, you will get the knowledge and skills you need to not only survive drinking less, but to thrive throughout your journey. In addition to daily research-backed readings that teach you all about the neuroscience of alcohol, you will have access to our in-app Toolkit full of resources and activities to help you navigate any situation you find yourself in.
Meet millions of fellow Reframers just like you in our 24/7 Forum chat and daily Zoom check-in meetings to get encouragement and inspiration from people all over the world who are on a similar journey. We can also connect you with our licensed Reframe coaches for more personalized guidance.
With the Reframe app, you will never get bored: we’re constantly adding new features to improve your in-app experience. Meet our in-app chatbot, Melody, powered by the world’s most powerful AI technology — she is here to help as you adjust to a life with less (or no) alcohol.
And there’s more! Every month, we launch fun challenges — like Dry/Damp January, Mental Health May, and Outdoorsy June — for you to participate alongside fellow Reframers (or solo if you prefer!).
The Reframe app is free for 7 days, so you can download it today with absolutely no risk! Are you ready to feel empowered and discover life beyond alcohol? Can’t wait to welcome you into our caring and fun community!
There’s no way around it — cirrhosis, a severe liver disease primarily caused by excessive alcohol consumption, is a heavy topic. But before you start to panic, rest assured that a single glass of Chianti isn’t the culprit here. When it comes to risk, it’s all about the amount and frequency of alcohol consumption. So, how much alcohol causes cirrhosis? What are alcoholic cirrhosis symptoms? And what is liver cirrhosis treatment like? Let’s find out!
First, let’s talk about the causes and risk of liver cirrhosis. When we’re talking about booze, the reason it causes liver cirrhosis has to do with the way our body processes alcohol. First the liver transforms it into a toxic substance called acetaldehyde, and then into the non-toxic acetate. This two-step process is taxing for the liver, and it supersedes any other duties the liver might otherwise be fulfilling.
Our livers are incredibly resilient. They can take the hit of moderate alcohol consumption, heal, and regenerate. However, long-term heavy drinking can overwhelm this regeneration process, leading to scarring of the liver, called cirrhosis.
Cirrhosis is a late stage of scarring — also known as liver fibrosis — of the liver caused by the repeated process of damaged tissue repairing itself. Over time, as more and more scar tissue forms, the structure of the liver changes: it becomes hard and lumpy and starts to function less efficiently. Eventually, liver fibrosis can progress to cirrhosis.
This inefficient functioning of the liver can have a significant impact on our bodies. Our livers perform hundreds of vital functions: filtering toxins from our blood, aiding digestion, metabolizing drugs and hormones, storing vitamins and nutrients, and even helping clot our blood.
In the early stages of cirrhosis, one might not experience any symptoms. As cirrhosis progresses, symptoms and complications can develop that indicate the liver is severely damaged. These can include fatigue, easy bruising, jaundice (yellow discoloration of the skin and eyes), intense itching, fluid accumulation in the abdomen, loss of appetite, and confusion, drowsiness, and slurred speech.
Cirrhosis doesn't occur overnight. The liver damage that leads to cirrhosis is gradual, often taking many years of consistent heavy drinking. The initial stage, “alcoholic fatty liver disease,” is reversible. The next phase — alcoholic hepatitis — is when inflammation and liver cell damage start to occur. With the right steps, it’s still manageable; however, if heavy drinking continues, alcoholic cirrhosis becomes a real risk.
Unfortunately, once cirrhosis is present it tends to be permanent; it's very difficult to repair the damaged liver tissue. However, if the cirrhosis is diagnosed early enough, damage can be minimized by treating the underlying cause or various complications arising from it. As far as liver cirrhosis treatment goes, this usually means setting booze aside. In severe cases of cirrhosis, liver transplantation may be the only treatment option.

Now for the million-dollar question: how much alcohol causes cirrhosis? There is no neat, one-size-fits-all answer, unfortunately. The process is complex, and it depends on a variety of factors such as drinking patterns, body weight, age, and genetics.
As a general rule, though, men who consume more than 3-4 drinks per day and women who have 2-3 drinks daily over a period of 10 to 12 years are more likely to develop cirrhosis. This might seem manageable, but keep in mind that one standard “drink” equals 14 grams of pure alcohol. That's about 1.5 ounces of distilled spirits, 5 ounces of wine, or 12 ounces of regular beer.
A common misconception is that cirrhosis is a problem for the “heavy drinkers” only. While it's true that the risk increases as consumption increases, even moderate drinking can, over time, contribute to liver disease. This is especially true if it’s combined with other liver stressors, like obesity or viral hepatitis. It's not just the number of drinks that count: it’s our overall health context.
What about if we’ve already been diagnosed — is drinking with cirrhosis an absolute no? Well, let’s just say it’s not the best idea. For one thing, it can exacerbate liver inflammation and increase the risk of liver failure. Drinking alcohol with cirrhosis can also increase the risk of developing other health complications, such as bleeding disorders, kidney problems, and an increased risk of liver cancer.
And occasional drinking with cirrhosis? Again, it’s best to tread carefully. It’s important to give our liver time to rest and recover to avoid making things worse, so even occasional drinking with cirrhosis can be asking for trouble.
It's not all doom and gloom! Just as our behavior contributed to the damage, our behavior has the power to help our livers heal. Cirrhosis is largely preventable by reducing alcohol consumption or abstaining entirely.
Here are some steps we can take on a journey to heal our liver:
Cirrhosis poses a very real threat to our liver, and alcohol consumption is its primary cause. But there’s no need to blame ourselves or dwell on past choices. Let’s empower ourselves with knowledge and make conscious decisions moving forward.
Our livers are some of the hardest workers in our bodies, and it's never too late to show them some love. Let's treat them kindly, and they'll pay us back in kind with health, vitality, and the freedom to enjoy life's pleasures.
There’s no way around it — cirrhosis, a severe liver disease primarily caused by excessive alcohol consumption, is a heavy topic. But before you start to panic, rest assured that a single glass of Chianti isn’t the culprit here. When it comes to risk, it’s all about the amount and frequency of alcohol consumption. So, how much alcohol causes cirrhosis? What are alcoholic cirrhosis symptoms? And what is liver cirrhosis treatment like? Let’s find out!
First, let’s talk about the causes and risk of liver cirrhosis. When we’re talking about booze, the reason it causes liver cirrhosis has to do with the way our body processes alcohol. First the liver transforms it into a toxic substance called acetaldehyde, and then into the non-toxic acetate. This two-step process is taxing for the liver, and it supersedes any other duties the liver might otherwise be fulfilling.
Our livers are incredibly resilient. They can take the hit of moderate alcohol consumption, heal, and regenerate. However, long-term heavy drinking can overwhelm this regeneration process, leading to scarring of the liver, called cirrhosis.
Cirrhosis is a late stage of scarring — also known as liver fibrosis — of the liver caused by the repeated process of damaged tissue repairing itself. Over time, as more and more scar tissue forms, the structure of the liver changes: it becomes hard and lumpy and starts to function less efficiently. Eventually, liver fibrosis can progress to cirrhosis.
This inefficient functioning of the liver can have a significant impact on our bodies. Our livers perform hundreds of vital functions: filtering toxins from our blood, aiding digestion, metabolizing drugs and hormones, storing vitamins and nutrients, and even helping clot our blood.
In the early stages of cirrhosis, one might not experience any symptoms. As cirrhosis progresses, symptoms and complications can develop that indicate the liver is severely damaged. These can include fatigue, easy bruising, jaundice (yellow discoloration of the skin and eyes), intense itching, fluid accumulation in the abdomen, loss of appetite, and confusion, drowsiness, and slurred speech.
Cirrhosis doesn't occur overnight. The liver damage that leads to cirrhosis is gradual, often taking many years of consistent heavy drinking. The initial stage, “alcoholic fatty liver disease,” is reversible. The next phase — alcoholic hepatitis — is when inflammation and liver cell damage start to occur. With the right steps, it’s still manageable; however, if heavy drinking continues, alcoholic cirrhosis becomes a real risk.
Unfortunately, once cirrhosis is present it tends to be permanent; it's very difficult to repair the damaged liver tissue. However, if the cirrhosis is diagnosed early enough, damage can be minimized by treating the underlying cause or various complications arising from it. As far as liver cirrhosis treatment goes, this usually means setting booze aside. In severe cases of cirrhosis, liver transplantation may be the only treatment option.

Now for the million-dollar question: how much alcohol causes cirrhosis? There is no neat, one-size-fits-all answer, unfortunately. The process is complex, and it depends on a variety of factors such as drinking patterns, body weight, age, and genetics.
As a general rule, though, men who consume more than 3-4 drinks per day and women who have 2-3 drinks daily over a period of 10 to 12 years are more likely to develop cirrhosis. This might seem manageable, but keep in mind that one standard “drink” equals 14 grams of pure alcohol. That's about 1.5 ounces of distilled spirits, 5 ounces of wine, or 12 ounces of regular beer.
A common misconception is that cirrhosis is a problem for the “heavy drinkers” only. While it's true that the risk increases as consumption increases, even moderate drinking can, over time, contribute to liver disease. This is especially true if it’s combined with other liver stressors, like obesity or viral hepatitis. It's not just the number of drinks that count: it’s our overall health context.
What about if we’ve already been diagnosed — is drinking with cirrhosis an absolute no? Well, let’s just say it’s not the best idea. For one thing, it can exacerbate liver inflammation and increase the risk of liver failure. Drinking alcohol with cirrhosis can also increase the risk of developing other health complications, such as bleeding disorders, kidney problems, and an increased risk of liver cancer.
And occasional drinking with cirrhosis? Again, it’s best to tread carefully. It’s important to give our liver time to rest and recover to avoid making things worse, so even occasional drinking with cirrhosis can be asking for trouble.
It's not all doom and gloom! Just as our behavior contributed to the damage, our behavior has the power to help our livers heal. Cirrhosis is largely preventable by reducing alcohol consumption or abstaining entirely.
Here are some steps we can take on a journey to heal our liver:
Cirrhosis poses a very real threat to our liver, and alcohol consumption is its primary cause. But there’s no need to blame ourselves or dwell on past choices. Let’s empower ourselves with knowledge and make conscious decisions moving forward.
Our livers are some of the hardest workers in our bodies, and it's never too late to show them some love. Let's treat them kindly, and they'll pay us back in kind with health, vitality, and the freedom to enjoy life's pleasures.